We read with great interest the report by Broberg et al on seeking an optimal relation between oxygen saturation at rest and hemoglobin (Hb). In patients with Eisenmenger syndrome (ES), chronic hypoxia due to right-to-left shunting results in increased erythropoiesis with secondary erythrocytosis. This is a physiologic response to maintain arterial oxygen content and therefore oxygen delivery to the peripheral tissues. Iron replacement therapy in iron-deficient cyanotic congenital heart disease patients caused an increase in Hb, which resulted in a significant improvement in exercise tolerance. In contrast, an increase in whole-blood viscosity (WBV) is an unavoidable result of an increased erythropoiesis and, by increasing peripheral resistance, will increase the afterload in patients with ES. Broberg et al showed earlier that hematocrit (Hct) is the main determinant of WBV, independent of red cell size, red cell shape, or iron stores. However, it has also been shown that for a certain Hb concentration, WBV may be higher in iron-deficient patients. Should we focus on Hct or Hb in patients with ES?
In this study, 74 patients with ES included in the Belgian Congenital Heart Disease registry were evaluated. Laboratory measurements were performed at the different centers using the same techniques. Hct, Hb concentration, mean corpuscular volume, and mean corpuscular Hb were obtained with automated electronic particle counters. The laboratory test also included ferritin and transferrin saturation. Iron deficiency was defined as ferritin <30 ng/ml or ferritin 30 to 100 ng/ml and a transferring saturation <20%. WBV was estimated using the formula proposed by Hutton et al : ln(WBV) = [Hb concentration (g/dl)/ln(mean corpuscular Hb) (pg)] × [0.5696 − 0.0542 ln(shear rate + 0.3214)].
For the purposes of the study, a shear rate of 2.3 seconds −1 was considered. Oxygen-carrying capacity was estimated as 1.39 ml oxygen/g Hb × Hb (g/dl) × saturation (%). The small proportion of oxygen dissolved in the blood was not considered (0.003 × arterial oxygen pressure).
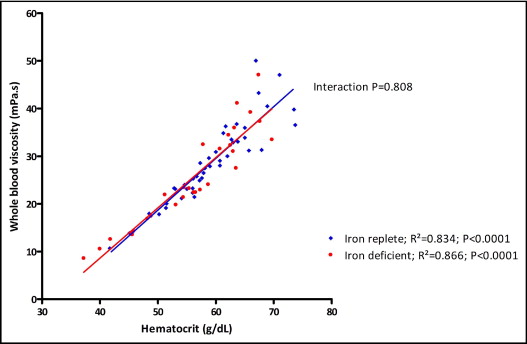
A linear regression was performed to assess the relation between Hct, Hb and oxygen-carrying capacity with WBV. To assess whether the relation was significantly different between iron-replete and iron-deficient patients, the interaction between the 2 groups was evaluated. All tests were 2 sided, and p values <0.05 were considered statistically significant.
Patients’ mean age was 36 ±14 years, and 28% were men. Forty-six percent of patients had Down syndrome. Thirty-eight percent of patients were in New York Heart Association class ≥III, and 57% were receiving specific pulmonary arterial hypertension treatment. Thirty-nine percent (n = 29) were iron deficient.
The Hct of iron-deficient patients was not statistically different (56 ± 9% vs 59 ± 7%, p = 0.093), whereas Hb was significantly lower (18 ± 3 vs 20 ± 2 g/dl, p <0.0001) compared to iron-replete patients. There was a linear relation between Hct and WBV in iron-replete (R 2 = 0.834, p <0.0001) and iron-deficient (R 2 = 0.866, p <0.0001) patients. Moreover, there was no significant interaction between the 2 groups (p = 0.808; Figure 1 ) . There was a linear relation between Hb and WBV in iron-replete (R 2 = 0.923, p <0.0001) and iron-deficient (R 2 = 0.854, p <0.0001) patients. The relation between the 2 groups was significantly different (interaction p <0.0001; Figure 2 ) . Finally, there was a weaker relation between oxygen-carrying capacity and WBV in iron-replete (R 2 = 0.507, p <0.0001) and iron-deficient (R 2 = 0.349, p = 0.001) patients. The relation differed significantly between the 2 groups (interaction p = 0.037; Figure 3 ) .