There has been controversy over the disparity between men and women with regard to the management and prognosis of acute myocardial infarction. Analyzing nationwide multicenter prospective registries in Korea, the aim of this study was to determine whether female gender independently imposes a risk for mortality. Data from 14,253 patients who were hospitalized for ST-segment elevation myocardial infarction from November 2005 to September 2010 were extracted from registries. Compared to men, women were older (mean age 56 ± 12 vs 67 ± 10 years, p <0.001), and female gender was associated with a higher frequency of co-morbidities, including hypertension, diabetes, and dyslipidemia. Women had longer pain-to-door time and more severe hemodynamic status than men. All-cause mortality rates were 13.6% in women and 7.0% in men at 1 year after the index admission (hazard ratio for women 2.01, 95% confidence interval 1.80 to 2.25, p <0.001). The risk for death after ST-segment elevation myocardial infarction corresponded highly with age. Although the risk remained high after adjusting for age, further analyses adjusting for medical history, clinical performance, and hemodynamic status diminished the gender effect (hazard ratio 1.00, 95% confidence interval 0.86 to 1.17, p = 0.821). Propensity score matching, as a sensitivity analysis, corroborated the results. In conclusion, this study shows that women have a comparable risk for death after ST-segment elevation myocardial infarction as men. The gender effect was accounted for mostly by the women’s older age, complex co-morbidities, and severe hemodynamic conditions at presentation.
The aim of this study was to identify differences due to gender with respect to risk factors, management patterns, and clinical outcomes in patients with ST-segment elevation myocardial infarction (STEMI) using the nationwide registries in Korea.
Methods
Efforts have been made to collect data nationwide and to standardize clinical practice regarding acute myocardial infarction (MI) in Korea. Part of that effort has been the Korean Acute Myocardial Infarction Registry (KAMIR), a nationwide registry conducted from November 2005 to January 2008, and its successor, the Korean Myocardial Infarction (KorMI) registry, conducted from January 2008 to July 2010. These registries were supported by the Korean Working Group of Acute Myocardial Infarction. The aims and protocols of the registries have been published elsewhere. The protocols of the 2 prospective cohorts were similar. Data from KAMIR and KorMI were purposely merged to maximize statistical power. Participating centers included 53 university or community hospitals that have high volumes of patients with facilities for primary percutaneous coronary intervention (PCI) and onsite cardiac surgery (details are provided in the Supplementary File ). The study protocol was reviewed and approved by the institutional review board at each participating center. In this study, data from patients diagnosed with STEMI were extracted from the database. Demographic data, procedural details, and clinical outcomes were available, and patients with invalid or incomplete data were excluded from this analysis.
Variables including demographic features, medical history, clinical characteristics, laboratory findings, clinical performance, and angiographic findings were obtained. Clinical follow-up was performed at 1, 6, and 12 months after the index admission. The primary end point was 1-year all-cause death. Clinical events were defined according to the Academic Research Consortium consensus. All deaths were considered cardiac in origin unless a noncardiac origin was definitely documented. Recurrent MI was defined as recurrent symptoms with new ST-segment elevation or recurrent elevation of cardiac markers to ≥2 times the upper limit of normal. Target vessel revascularization was defined as any repeat intervention (surgical or percutaneous) of any segment of the target vessel, which included upstream and downstream branches and the target lesion itself. Major adverse cardiovascular events were defined as a composite of all-cause death, MI, or target vessel revascularization.
Baseline data are presented as frequencies or as mean ± SD. Continuous variables were compared using Student’s t tests and categorical variables using the chi-square tests. The Kaplan-Meier method was used for survival analysis. The association of gender and the primary outcome was examined using univariate and multivariate Cox proportional-hazards models. A total of 4 multivariate models were constructed: the first adjusted for age; the second for age and medical history; the third for age, medical history, and clinical performance; and the fourth for age, medical history, clinical performance, and hemodynamic status.
Missing data were handled as follows: because missing data analysis showed monotonicity in the distribution of missing values, 129 patients with multiple missing values were excluded from the study. Then, missing binary data, whose proportion did not exceed 2% for each covariate, were coded as not present, an approach that may bias the relation between a covariate and outcome toward the null. Missing categorical data, such as body mass index, Killip class, pain-to-door time, door-to-needle time, and door-to-balloon time were coded as “missing.”
Propensity score matching and adjustment for the Global Registry of Acute Coronary Events (GRACE) score were performed as a sensitivity analysis. Although propensity score matching was originally developed to reduce the effects of the treatment selection bias or confounders when estimating the effects of treatments when using observational data, this method has also proved useful in controlling for the background covariates of interest over other matching techniques. The method of propensity score matching is detailed in the Supplementary File . The GRACE score is a widely used risk scoring system to predict mortality in patients with acute coronary syndromes. The Cox regression method was used to calculate the risk ratio adjusted for the GRACE score. A 2-sided p value <0.05 was considered significant. Statistical analyses were performed using the R programming language (R Project for Statistical Computing, Vienna, Austria).
Results
Figure 1 describes the study scheme. Among a total of 29,199 subjects from the 2 databases, data from 14,123 patients with STEMI were extracted for this study: 10,398 men (73.6%) and 3,725 women (26.4%). The proportion of women among the study subjects did not vary across time ( Supplementary Figure 1 ). The median follow-up duration was 222 days.
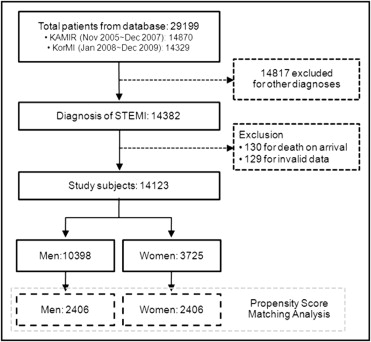
Table 1 lists the comparison of the baseline characteristics between men and women. Women were 11.1 ± 0.2 years older and had lower body mass indexes than men. Women were shown to be associated with a higher frequency of co-morbidities, including hypertension, diabetes mellitus, dyslipidemia, and familial history of coronary heart disease, than men. Compared to men, pain-to-door time was delayed, blood pressure at presentation was depressed, and Killip class was poor in women. Smoking status, meanwhile, was favorable for women, with a lower frequency of current or previous smokers.
| Variable | Men | Women | p Value |
|---|---|---|---|
| (n = 10,398) | (n = 3,725) | ||
| Age (years) | 56 ± 12 (10,322) | 67 ± 10 (3,693) | <0.001 |
| Body mass index (kg/m 2 ) | 24.1 ± 3.2 (9,511) | 23.5 ± 3.5 (3,227) | <0.001 |
| History of ischemic heart disease | 11.8% (1,243) | 11.2% (422) | 0.301 |
| Hypertension | 41.0% (4,266) | 61.2% (2,279) | <0.001 |
| Diabetes mellitus | 22.9% (2,380) | 30.9% (1,150) | <0.001 |
| Dyslipidemia | 9.6% (995) | 8.5% (316) | 0.050 |
| Smoking status | <0.001 | ||
| Ex-smoker | 17.8% (1,846) | 3.0% (110) | |
| Current smoker | 58.6% (6,098) | 12.9% (479) | |
| Familial history of coronary heart disease | 8.2% (850) | 4.7% (176) | <0.001 |
| Resuscitation before arrival | 2.5% (261) | 2.6% (96) | 0.823 |
| Systolic blood pressure (mm Hg) | 125 ± 29 (10,130) | 123 ± 32 (3,628) | <0.001 |
| Diastolic blood pressure (mm Hg) | 78 ± 21 (10,080) | 75 ± 19 (3,597) | <0.001 |
| Heart rate (per min) | 77 ± 20 (10,121) | 77 ± 22 (3,637) | 0.091 |
| Killip class | 100.0% (9,832) | 100.0% (3,530) | <0.001 |
| I | 72.5% (7,131) | 61.1% (2,157) | |
| II | 14.3% (1,403) | 17.0% (601) | |
| III | 6.3% (618) | 11.3% (398) | |
| IV | 6.9% (680) | 10.6% (374) | |
| Ejection fraction (%) | 51 ± 12 (9,245) | 50 ± 12 (3,222) | 0.004 |
| Serum glucose (mg/dl) | 171 ± 76 (10,118) | 191 ± 92 (3,625) | <0.001 |
| Serum creatinine (mg/d) | 1.2 ± 1.9 (10,252) | 1.1 ± 2.3 (3,671) | 0.024 |
| Creatine kinase-MB (mg/dl) | 187 ± 302 (10,235) | 168 ± 337 (3,656) | 0.001 |
| Troponin I (mg/dl) | 62.3 ± 109.9 (8,255) | 61.8 ± 246.3 (3,040) | 0.884 |
| Total cholesterol (mg/dl) | 181 ± 43 (9,947) | 186 ± 48 (3,502) | <0.001 |
| Triglyceride (mg/dl) | 130 ± 112 (9,683) | 115 ± 89 (3,378) | <0.001 |
| High-density lipoprotein cholesterol (mg/dl) | 44 ± 17 (9,610) | 46 ± 16 (3,335) | <0.001 |
| Low-density lipoprotein cholesterol (mg/dl) | 115 ± 38 (9,203) | 120 ± 48 (3,214) | <0.001 |
With regard to the initial treatment strategy, women were managed less aggressively than men: women were treated with conservative treatment more often than men were, and door-to-balloon time was delayed more in women among those who were treated with primary PCI according to the American Heart Association treatment goal (≤90 minutes). However, most patients underwent coronary angiography before discharge during the index admission, with a similar rate between the 2 genders ( Table 2 ). Although more women were associated with multivessel involvement, PCI was performed in a slightly smaller number of women than men, and apparently, the rest might have been managed with medical treatment alone.
| Variable | Men | Women | p Value |
|---|---|---|---|
| (n = 10,398) | (n = 3,725) | ||
| Clinical performance | |||
| Pain-to-door time (minutes) | 161 (75–330) (9,674) | 217 (115–420) (3,410) | <0.001 |
| Pain-to-door time ≤360 minutes | 71.8% (7,463) | 63.8% (2,376) | <0.001 |
| Initial treatment strategy | 100.0% (10,273) | 100.0% (3,694) | <0.001 |
| Conservative management | 9.1% (934) | 11.2% (412) | |
| Thrombolysis | 7.9% (814) | 5.5% (203) | |
| Primary PCI | 81.4% (8,360) | 81.7% (3,018) | |
| Facilitated PCI | 1.6% (165) | 1.6% (61) | |
| Door-to-balloon time (minutes) | 80 (58–115) (7,384) | 80 (60–118) (2,620) | 0.875 |
| Door-to-balloon time ≤90 minutes | 61.4% (4,536) | 59.0% (1,546) | 0.029 |
| Door-to-needle time (minutes) | 52 (32–89) (740) | 54 (31–97) (180) | 0.174 |
| Door-to-needle time ≤30 minutes | 24.3% (181) | 24.9% (45) | 0.913 |
| Coronary angiography | 98.9% (10,287) | 98.7% (3,675) | 0.160 |
| PCI performed | 97.0% (10,086) | 95.9% (3,574) | 0.002 |
| Coronary care unit/intensive care unit | 87.0% (9,044) | 87.0% (3,239) | 0.969 |
| Angiographic findings | |||
| Coronary angiographic findings | 100.0% (9,952) | 100.0% (3,508) | 0.649 |
| No significant stenosis | 2.4% (236) | 2.5% (88) | |
| Significant stenosis | 97.6% (9,716) | 97.5% (3,420) | |
| Number of coronary arteries narrowed | 100.0% (9,569) | 100.0% (3,374) | <0.001 |
| 1 | 47.2% (4,521) | 41.9% (1,415) | |
| 2 | 30.9% (2,958) | 31.6% (1,065) | |
| 3 | 21.8% (2,090) | 26.5% (894) | |
| Culprit coronary artery | 100.0% (9,561) | 100.0% (3,370) | 0.017 |
| Left anterior descending | 51.8% (4,950) | 50.5% (1,702) | |
| Left circumflex | 9.9% (943) | 9.3% (314) | |
| Right | 36.5% (3,491) | 38.9% (1,311) | |
| Left main | 1.9% (177) | 1.3% (43) | |
| Lesion type | 100.0% (8,588) | 100.0% (3,082) | 0.101 |
| A | 4.5% (386) | 4.4% (135) | |
| B1 | 17.6% (1,509) | 16.4% (506) | |
| B2 | 28.3% (2,434) | 27.0% (833) | |
| C | 49.6% (4,259) | 52.2% (1,608) |
The results of the clinical performance adjusting for baseline characteristics are listed in Table 3 . Adjustment analysis showed no significant difference in the performance of coronary angiography between the 2 groups, similar to the crude analysis. The rate of PCI still differed after adjustment, although the gap narrowed, losing statistical significance, when the model was expanded to include angiographic findings. The proportion of initiation of revascularization therapy within the recommended time frame (thrombolysis with door-to-needle time ≤30 minutes or primary PCI with door-to-balloon time ≤90 minutes) did not differ significantly after multivariate adjustment.
| Variable | Frequency (n) | Unadjusted Analysis | Adjusted Analysis ⁎ | ||||
|---|---|---|---|---|---|---|---|
| Men | Women | OR (95% CI) | p Value | OR (95% CI) | p Value | C Statistic | |
| Coronary angiography | 98.9% (10,287) | 98.7% (3,675) | 0.79 (0.56–1.10) | 0.161 | 1.14 (0.74–1.77) | 0.545 | 0.94 |
| Percutaneous coronary intervention | 97.0% (10,086) | 95.9% (3,574) | 0.73 (0.60–0.89) | 0.002 | 0.64 (0.50–0.82) | 0.001 | 0.86 |
| 0.66 (0.68–1.15) | 0.139 | 0.86 † | |||||
| Adherence to AHA goal ‡ | 45.3% (4,714) | 42.7% (1,590) | 0.90 (0.83–0.97) | 0.005 | 1.06 (0.96–1.17) | 0.224 | 0.71 |
| Death | 6.7% (693) | 13.3% (495) | 2.15 (1.90–2.43) | <0.001 | 1.01 (0.87–1.18) | 0.878 | 0.82 |
| Cardiac death | 5.7% (592) | 12.0% (447) | 2.26 (1.99–2.57) | <0.001 | 1.09 (0.93–1.28) | 0.309 | 0.83 |
| Noncardiac death | 1.0% (103) | 1.3% (48) | 1.31 (0.92–1.84) | 0.130 | 0.66 (0.45–0.96) | 0.031 | 0.75 |
| Recurrent MI | 0.7% (69) | 0.7% (27) | 1.09 (0.70–1.71) | 0.696 | 0.98 (0.58–1.65) | 0.936 | 0.66 |
| Target vessel revascularization | 2.9% (304) | 2.8% (104) | 0.95 (0.76–1.20) | 0.681 | 0.98 (0.75–1.27) | 0.857 | 0.59 |
| Major adverse cardiovascular events | 10.1% (1,046) | 16.6% (620) | 1.79 (1.60–1.99) | <0.001 | 1.03 (0.90–1.17) | 0.669 | 0.73 |
⁎ Model adjusted for age, body mass index (<18.5, 18.5 to 22.9, 23.0 to 24.9, 25.0 to 29.9, and ≥30 kg/m 2 or missing), history of ischemic heart disease, hypertension, diabetes, dyslipidemia, current smoking (yes or no), presence of familial history, pain-to-door time (<6 or ≥6 hours or unavailable), initial strategy (conservative management, thrombolysis, primary PCI, or facilitated PCI), adherence to AHA guideline (door-to-needle time ≤30 minutes, door-to-balloon time ≤90 minutes), admission to coronary care unit and/or intensive care unit, coronary angiography, PCI, Killip class (1.2 to 4 or missing), and provision of cardiopulmonary resuscitation.
† The model expands the variables listed above to include angiographic findings such as significant stenosis, extent of coronary involvement, culprit vessel, and AHA lesion classification. Accordingly, the number of patients included in the analysis shrank from 13,988 to 11,549.
‡ Adherence to AHA treatment goals was defined as thrombolysis with door-to-needle time ≤30 minutes or primary PCI with door-to-balloon time ≤90 minutes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


