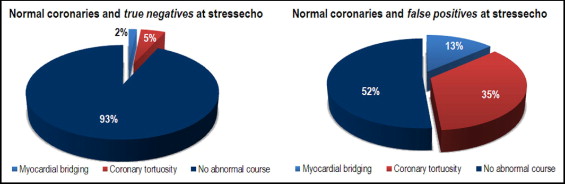
We reviewed patients with normal or near-normal coronary angiograms enrolled in the SPAM contrast stress echocardiographic diagnostic study in which 400 patients with chest pain syndrome of suspected cardiac origin with a clinical indication to coronary angiography were enrolled. Patients underwent dipyridamole contrast stress echocardiography (cSE) with sequential analysis of wall motion, myocardial perfusion, and Doppler coronary flow reserve before elective coronary angiography. Ninety-six patients with normal or near-normal epicardial coronary arteries were screened for the presence of 2 prespecified findings: severely tortuous coronary arteries and myocardial bridging. Patients were divided in 2 groups based on the presence (false-positive results, n = 37) or absence (true-negative results, n = 59) of reversible myocardial perfusion defects during cSE and compared for history and clinical and angiographic characteristics. Prevalence of severely tortuous coronary arteries (35% vs 5%, p <0.001) or myocardial bridging (13% vs 2%, p <0.05) was 7 times higher in patients who demonstrated reversible perfusion defects at cSE compared to those without reversible perfusion defects. No significant differences were found between the 2 groups for the main demographic variables and risk factors. Patients in the false-positive group more frequently had a history of effort angina (p <0.001) and ST-segment depression at treadmill electrocardiography (p <0.001). In conclusion, we hypothesize that patients with a positive myocardial perfusion finding at cSE but without obstructive epicardial coronary artery disease have a decreased myocardial blood flow reserve, which may be caused by a spectrum of causes other than obstructive coronary artery disease, among which severely tortuous coronary arteries/myocardial bridging may play a significant role.
Most diagnostic studies aiming at the detection of coronary artery disease rely solely on angiographic percent epicardial coronary stenosis as the reference, whereas functional measurements of the coronary circulation are seldom used. This attitude may have led to underappreciation of nonconventional mechanisms other than obstructive coronary plaques that can ultimately lead to impaired myocardial blood flow and angina during stress or exercise. We retrospectively reviewed all patients with normal or near-normal coronary angiograms enrolled in the Stress-echo PArma Mestre (SPAM) diagnostic study, in which 400 patients with chest pain syndrome of suspected cardiac origin with a clinical indication for coronary angiography were enrolled from 2 centers. Patients underwent high-dose dipyridamole contrast stress echocardiography (cSE) with sequential analysis of wall motion (WM), myocardial perfusion (MP), and Doppler coronary flow reserve of the left anterior descending coronary artery before elective coronary angiography. In the present analysis only patients with normal or near-normal epicardial coronary arteries from the SPAM study were considered and their angiograms were screened for the presence of 2 prespecified findings: severely tortuous coronary arteries (STCAs) and myocardial bridging (MB). Patients were divided in 2 groups based on the presence or absence of reversible MP defects during cSE. The 2 groups were then compared for history and clinical and angiographic characteristics. The study hypothesis was that patients with chest pain syndrome who demonstrated reversible MP defects at cSE but had angiographically normal coronary arteries would demonstrate a higher prevalence of STCAs or MB compared to patients without reversible MP defects.
Methods
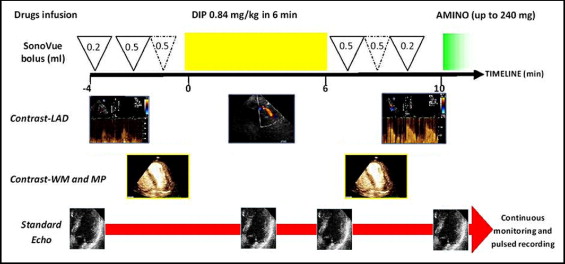
Of 400 patients originally enrolled in the SPAM study, we selected 96 patients with normal or near-normal coronary arteries (<30% stenosis on quantitative coronary angiogram) and without previous myocardial infarction and previous coronary revascularization; we divided them into a true-negative group (patients without reversible MP defects, n = 59) and a false-positive group (patients with reversible MP defects, n = 37) based on contrast stress echocardiographic MP data. We compared these 2 groups for cardiac history and clinical, echocardiographic, and angiographic characteristics. Briefly, in the SPAM study patients were prospectively enrolled from cardiology departments of Parma and Venice, Italy; 454 patients with chest pain syndrome scheduled for clinically indicated coronary angiography were considered; 32 refused their consent and 22 presented exclusion criteria; 400 patients represented the final study group. The study was approved by the institutional review boards. Two-dimensional echocardiographic, 12-lead electrocardiographic, and blood pressure monitoring were performed in combination with accelerated high-dose dipyridamole (0.84 mg/kg over 6 minutes) in accordance with a well-established protocol. The contrast stress echocardiographic protocol is graphically presented in Figure 1 . Stress echocardiograms were performed using commercially available ultrasound machines (iE33, Philips Ultrasound, Andover, Massachusetts) equipped with phased-array probe (S5) and low mechanical index power modulation technology. Contrast WM, coronary flow reserve of the left anterior descending coronary artery, and MP were assessed during stress echocardiography using the same probe by activation of the appropriate preset. The left ventricle was divided into 17 segments as suggested by the American Society of Echocardiography and European Society of Echocardiography. WM and MP were analyzed using a 0.5-ml repeated SonoVue bolus (Bracco Imaging Italia, s.r.l., Milan, Italy) at rest and at peak stress. Normal MP after dipyridamole was assigned if the myocardium was fully replenished 1.5 to 2 seconds after the end of flash impulse; MP was defined abnormal if the myocardium was not fully replenished after this time in ≥1 segment. The cutoff for normal replenishment at rest was considered 4 seconds after the flash impulse. Full details of the imaging protocol and settings are reported elsewhere. All patients underwent coronary angiography within 1 week after cSE. Angiograms were evaluated for the presence of significant stenosis in major epicardial coronary arteries and their branches (vessel diameter >2.0 mm) by an experienced cardiologist blinded to contrast stress echocardiographic data. Off-line maximum percent lumen decrease was determined for any visually evident stenosis using standard quantitative coronary angiographic software (Medis Medical Imaging Systems, Leiden, the Netherlands). For the present retrospective study all angiograms with <30% coronary artery stenosis at quantitative coronary angiography were also analyzed for the presence of these morphologic findings: (1) STCAs, defined as ≥1 coronary artery showing ≥3 consecutive curvatures ≤90° during diastole and (2) MB, based on >50% lumen diameter decrease from end-diastole to end-systole (“milking sign”). Continuous variables were presented as mean ± SD. Categorical variables were examined with chi-square or Fisher’s test, as appropriate. A p value <0.05 (2 sided) was considered statistically significant.
Results
The main demographic, clinical, echocardiographic, and angiographic characteristics of the 96 patients with normal/near-normal coronary arteries are listed in Table 1 . There were 16 patients with STCAs in ≥1 coronary artery (11 in the left anterior descending coronary artery, 2 in the left circumflex coronary artery, and 3 with ≥1 STCA) and 6 with angiographic MB (all involving the left anterior descending coronary artery); none had STCAs and MB. When patients were divided into 2 groups based on the presence (false positive) or absence (true negative) of reversible MP defects at cSE, there were no significant differences in the main demographic variables and risk factors, although there was a nonsignificant trend toward a higher prevalence of female gender in the false-positive group compared to the true-negative group (68% vs 54%, p = NS). Mean coronary flow reserve in the distal left anterior descending coronary artery was not different between the 2 groups (p = NS). The prevalence of STCAs (p <0.001) or MB (p <0.05) was 7 times higher in the false-positive group (i.e., patients with reversible MP defects; Figure 2 , Table 1 ). Patients in the false-positive group more frequently had a history of effort angina (p <0.001) and ST-segment depression at treadmill electrocardiography (p <0.001); compared to the true-negative group a larger number of patients in the false-positive group also presented reversible WM abnormalities (35% vs 0%, p <0.001). Table 2 presents demographic, echocardiographic, and clinical characteristics of the same 96 patients reclassified into groups based on the presence or absence of STCA/MB. No significant difference was apparent between these 2 groups for the main demographic and clinical variables; there was a trend toward a higher prevalence of reversible WM abnormalities but this difference was not statistically significant (27% vs 9%, p = 0.07). Patients with STCA or MB more frequently had a history of effort angina and ST-segment depression at treadmill electrocardiography (p <0.05) and more frequently had reversible MP defects at cSE (p <0.001; Figure 3 ) .
| Characteristics | Patients With Normal Coronary Arteries | True-Negative Results at cSE | False-Positive Results at cSE | p Value |
|---|---|---|---|---|
| (n = 96) | (n = 59) | (n = 37) | ||
| Age (years) | 60 ± 12 | 62 ± 11 | 58 ± 12 | NS |
| Age range | 29–85 | 34–85 | 29–78 | — |
| Women | 57 (59%) | 32 (54%) | 25 (68%) | NS |
| Risk factors and patient history | ||||
| Hypertension ⁎ | 55 (57%) | 34 (58%) | 21 (57%) | NS |
| Hypercholesterolemia † | 35 (36%) | 20 (34%) | 15 (41%) | NS |
| Smoker | 15 (16%) | 10 (17%) | 5 (14%) | NS |
| Diabetes mellitus | 14 (15%) | 10 (17%) | 4 (11%) | NS |
| Family history of coronary artery disease ‡ | 28 (29%) | 17 (29%) | 11 (30%) | NS |
| Predominantly effort-induced angina | 41/96 (43%) | 9/59 (15%) | 32/37 (86%) | <0.001 |
| Treadmill electrocardiography performed § | 47 (49%) | 22 (37%) | 25 (67%) | <0.01 |
| ST-segment depression on treadmill electrocardiogram ¶ | 28/47 (60%) | 7/22 (30%) | 21/25 (84%) | <0.001 |
| Echocardiographic data | ||||
| Ejection fraction (%) | 59 ± 9 | 57 ± 7 | 61 ± 11 | NS |
| Decreased ejection fraction (left ventricular ejection fraction <50%) | 5 (5%) | 3 (5%) | 2 (5%) | NS |
| Reversible myocardial perfusion abnormalities | 37 (39%) | 0 (0%) | 37 (100%) | — |
| Reversible wall motion abnormalities | 13 (14%) | 0 (0%) | 13 (35%) | <0.001 |
| Coronary flow reserve in distal left anterior descending coronary artery | 2.06 ± 0.4 | 2.0 ± 0.3 | 2.1 ± 0.6 | NS |
| Coronary angiographic results | ||||
| Patients with severe coronary tortuosity | 16 (17%) | 3 (5%) | 13 (35%) | <0.001 |
| Patients with myocardial bridging | 6 (6%) | 1 (2%) | 5 (13%) | <0.05 |
⁎ Blood pressure ≥140/90 mm Hg or treatment of hypertension.
† Total cholesterol level >180 mg/dl or treatment of hypercholesterolemia.
‡ History of myocardial infarction at any age in first-degree relatives.
§ Only 47 patients had a previous treadmill electrocardiogram available because this test was not part of the SPAM study protocol.
| Characteristics | Patients Without STCA or MB | Patients With STCA or MB | p Value |
|---|---|---|---|
| (n = 74) | (n = 22) | ||
| Age (years) | 60 ± 12 | 60 ± 12 | NS |
| Age range | 29–78 | 41–85 | — |
| Women | 40 (54%) | 16 (73%) | NS |
| Risk factors and patient history | |||
| Hypertension ⁎ | 42 (57%) | 13 (59%) | NS |
| Hypercholesterolemia † | 24 (32%) | 11 (50%) | NS |
| Smoker | 13 (18%) | 2 (9%) | NS |
| Diabetes mellitus | 11 (15%) | 3 (14%) | NS |
| Family history of coronary artery disease ‡ | 20 (27%) | 8 (36%) | NS |
| Predominantly effort-induced angina | 26 (35%) | 15 (68%) | <0.05 |
| Treadmill electrocardiography performed § | 34 (46%) | 13 (59%) | NS |
| ST-segment depression on treadmill electrocardiogram ¶ | 17 (53%) | 11 (85%) | <0.05 |
| Echocardiography data | |||
| Ejection fraction (%) | 60 ± 7 | 62 ± 16 | NS |
| Decreased ejection fraction (left ventricular ejection fraction <50%) | 4 (5%) | 1 (5%) | NS |
| Reversible wall motion abnormalities | 7 (9%) | 6 (27%) | NS |
| Reversible myocardial perfusion defects | 19 (26%) | 18 (82%) | <0.001 |
| Reversible myocardial perfusion defects matching coronary territory with tortuosity/bridging | — | 16/22 (73%) | — |
| Coronary flow reserve in distal left anterior descending coronary artery | 2.07 ± 0.31 | 2.2 ± 0.44 | NS |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


