Ventricular fibrillation (VF) is a lethal arrhythmia that requires immediate cardioversion and is rarely self-terminating. Spontaneous termination is typically associated with more organized activation than sustained VF terminated by shock, but the precise mechanism is unclear. In the present case, we describe a patient with recurrent syncope and documented self-terminating VF, who ultimately underwent implantable cardioverter defibrillator insertion. Assessment of the rhythm strip revealed organization of a chaotic rhythm into monomorphic ventricular tachycardia before termination, in supportive of previous reports. In conclusion, self-terminating VF is a very rare condition that can cause syncope.
The cardiac causes of syncope, primarily bradyarrhythmias and tachyarrhythmias, account for 10% to 20% of syncopal episodes. Of the tachyarrhythmias, ventricular tachycardia (VT) and, less commonly, supraventricular tachycardia can cause syncope. In contrast, ventricular fibrillation (VF) is an extremely rare cause of syncope. VF is a life-threatening arrhythmia that requires immediate cardioversion and is rarely self-terminating. In the present case, we describe a patient with recurrent syncope and self-terminating VF detected by implantable loop recorder (ILR). An implantable cardioverter defibrillator was inserted.
Case Report
A 68-year-old man was admitted to our hospital with recurrent syncope. Previously, he had had syncope after sitting up in bed. At that time, he had a prodrome of nausea, flushing, and dizziness. The cardiac evaluation included an electrocardiogram with normal findings, an echocardiogram that revealed normal biventricular function and no wall motion abnormality, and an imaging stress test that demonstrated a fixed infero-posterolateral defect. Angiography revealed 100% occlusion of the right coronary artery and a 50% narrowing of the obtuse marginal artery.
One year later, he lost consciousness at rest, without any preceding symptoms. Cardiopulmonary resuscitation was initiated immediately. On medical team arrival, he was awake and free of symptoms. His vital signs were normal. The electrocardiogram revealed sinus rhythm without evidence of previous infarction, acute ischemia, or Brugada, long QT, or short QT syndromes. The electrolytes and cardiac biomarker levels were normal. The echocardiogram displayed normal biventricular function with no wall motion abnormality. An electrophysiologic study was performed, revealing a normal voltage map, without evidence of an endocardial scar. Ventricular arrhythmia was not induced, with extra stimuli delivered from the right ventricular apex and the right ventricular outflow tract, with and without isoproterenol. Sinus node function and atrioventricular conduction were normal. Given recurrent unexplained syncope, an ILR was placed.
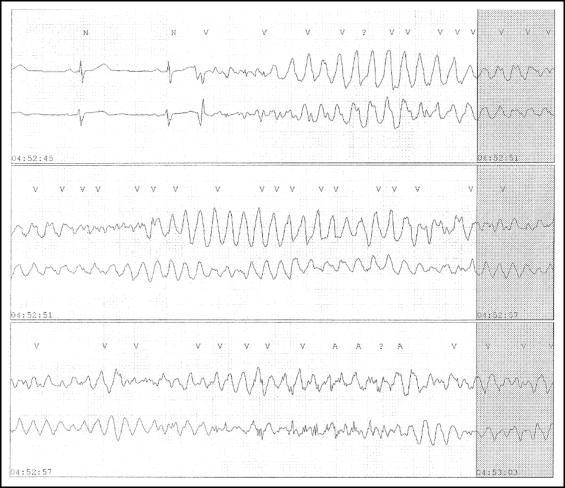
Two weeks later, a third syncopal episode occurred. The ILR tracing demonstrated VF, which organized into monomorphic VT and spontaneously terminated ( Figure 1 ). During hospitalization, another syncopal episode occurred, with no preceding symptoms. VF was documented ( Figure 2 ), and brief cardiopulmonary resuscitation was initiated with spontaneous VF termination. Cardioversion or medications were not required. Assessment of the initiating ventricular premature complex (VPC) revealed a Q wave in lead II, suggestive of a VPC originating from an inferior scar. An implantable cardioverter defibrillator was inserted.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


