Fig. 11.1
Coronary occluder® (Sumitomo Bakelite Co., Ltd.)
11.2 Coronary Artery Shunt
Temporary coronary occlusion in OPCAB is an easy way to obtain an optimal operative field without any disturbing device. Intraoperative hemodynamic deterioration and/or perioperative myocardial infarction are not encountered in almost all cases in clinical practice. However, transient myocardial ischemia can always affect the hemodynamic condition and cardiac contractile function. Yeatman M and colleagues showed that intraoperative hemodynamic deterioration was transient and recovered soon after the heart was repositioned to its anatomical position when the coronary artery was perfused with a shunt tube, whereas early cardiac functional recovery was impaired by the simple snaring technique [7]. Other group reported that the use of temporary intraluminal shunts resulted in reduced acute ischemia, maintained left ventricular (LV) function, and improved early graft patency compared with the simple coronary occlusion technique in minimally invasive direct coronary artery bypass (MIDCAB) [8].
There are two types of coronary perfusion systems: an intraluminal shunt and an extraluminal shunt. The intraluminal shunt is manufactured by several companies, and each shunt has its own structural features. It contains a shunt tube and a suture that holds the tube. The proximal and distal ends of the shunt tube are expanded slightly to fit the internal lumen of the coronary artery. After the target coronary artery is opened, an intraluminal shunt tube is inserted proximally and distally into the coronary artery. The intraluminal shunt can achieve both hemostasis and coronary perfusion. When the tube is inserted into the proximal side, the bloodstream from the tube should be checked out. The intraluminal shunt can be used in almost all coronary arteries.
Intraluminal shunts are safe, easy to handle, and quite useful (Fig. 11.2). However, if its manipulation is poor, the device can cause some serious problems. When an appropriate intraluminal shunt is used, the intraluminal shunt causes only minor damage of the coronary artery [9]. However, a larger shunt tube can injure the coronary endothelium, causing postoperative coronary stenosis [10], and the tube can tear and even penetrate the target artery. A smaller intraluminal shunt cannot achieve hemostasis. When the shunt is inserted into a meandering coronary artery, the tube can injure the coronary artery, and the shunt might not perfuse the coronary artery because the proximal and/or distal tip of the shunt tube might be closed by the meandering arterial wall. If the coronary artery is opened near a stenotic lesion, an intraluminal shunt cannot be inserted because it cannot pass through the stenotic lesion.
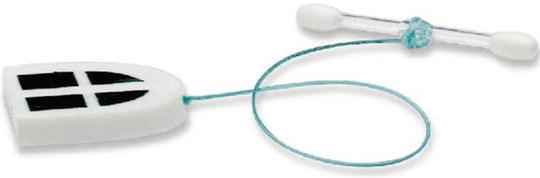
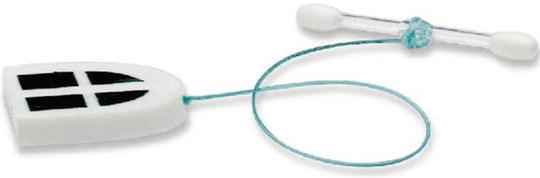
Fig. 11.2
A representative of intraluminal shunt: Anastaflow® (Edwards Lifescience
When we use an intraluminal shunt, we always encircle a target coronary artery just proximal and distal to the anastomotic site with a silicone elastic air cushion suture. The coronary artery should be incised approximately 5 mm in length as it is easier to insert the tube through the larger incision. When the target coronary artery is incised, the proximal elastic suture is slightly pulled upward to obtain temporary hemostasis, and the shunt tube is inserted in an optimal operative field. Then, the distal part is inserted into the distal coronary artery while the shunt tube is clamped with forceps to stop the bleeding. If hemostasis cannot be obtained, the proximal elastic suture is tightened with hemostat clips one by one toward the coronary artery, and the target artery containing the shunt tube is snared gently to stop bleeding. Just before the anastomotic suture is tied, the graft is de-aired, and the shunt is removed. We always select the appropriately sized or a smaller-sized tube as lesser coronary damage occurs with a smaller shunt than with a larger shunt, and a bigger shunt can tear the graft when it is removed.
External shunts are also safe and easy to use. After the proximal side of the target coronary artery is occluded, an external shunt tube is inserted toward the distal site of the coronary artery. The risk of injuring the coronary endothelium is the same as that for an intraluminal shunt, but external shunt has several features that are better than those of intraluminal shunt. The first advantage is that the inflow bloodstream is stronger than that of an intraluminal shunt. External shunt tubes have not been widely commercialized; thus, our group developed an original external shunt tube (Coronary perfusion catheter®, Sumitomo Bakelite, Japan) (Fig. 11.3) [11]. The blood inflow of an external shunt is usually obtained from a healthy femoral artery. We sometimes connect the tube to a saphenous vein graft already anastomosed to the ascending aorta and obtain good blood flow [12]. In the intraluminal shunt technique, the blood inflow originates from the diseased coronary artery, which might result in decreased blood flow. In our clinical experience, ischemic problems can be prevented by using an intraluminal shunt under stable circulatory conditions, but ischemia can occur even with an intraluminal shunt if the stenotic lesion is severe. From this viewpoint, the blood flow from the external shunt is always strong and sufficiently reliable to perfuse the target coronary artery. To obtain more reliable coronary perfusion, a coronary active perfusion system was created. The system injects arterial blood into the coronary artery during the diastolic phase of the cardiac cycle [13, 14].