Chapter 14
Secondary Prevention and Antiplatelet Therapy in Peripheral Arterial Disease
Richard Donnelly
Division of Medical Sciences & GEM, School of Medicine, University of Nottingham, UK
Introduction
Patients with peripheral arterial disease (PAD), especially those with symptoms, have a 3- to 4-fold increased risk of cardiovascular (CV) mortality as a result of atherosclerosis in other vascular territories, particularly the coronary and cerebral circulations. Furthermore, in population studies, the severity of PAD as measured by the ankle-brachial pressure index (ABPI) correlates with reduced survival (Figure 14.1). Thus, symptomatic PAD is indicative of systemic vascular disease—it is as important a prognostic marker as stable angina or recent myocardial infarction (MI)—and therefore patients should be treated with lifestyle and drug interventions as part of secondary prevention to improve lower limb and CV outcomes.
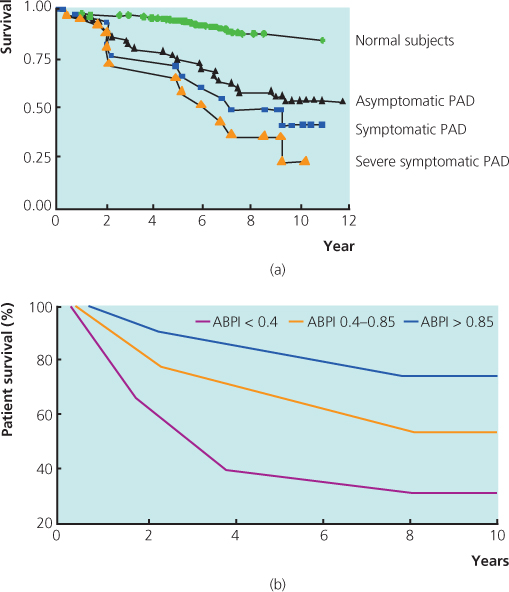
Figure 14.1 (a) Survival curves for patients with symptomatic and asymptomatic PAD, and those with severe symptoms (e.g. critical limb ischaemia), in a population cohort (data from Criqui et al., 1992) and (b) survival among patients with PAD according to ankle-brachial pressure index (ABPI). ABPI is an independent predictor of mortality. Source: McKenna et al. (1991). Reproduced by permission of Elsevier.
Most trials of secondary prevention have included patients with known, symptomatic PAD (e.g. those with intermittent claudication or previous revascularisation), but whether treatment recommendations for secondary prevention would apply to asymptomatic patients with PAD, e.g. those identified by population screening of ABPI, is unclear. In observational studies, however, treatment with two or more preventative therapies [including aspirin, statin and/or ACE (angiotensin-converting enzyme) inhibitor] was associated with a 65% reduced risk of all-cause mortality in individuals with PAD who had not previously had any symptoms of CV disease.
In surveys of routine clinical practice, a large proportion of patients with PAD fail to receive optimum secondary prevention (Box 14.1), in part because clinicians have misjudged the prognostic significance of lower limb symptoms. In the United States, it is estimated that 5m adults with PAD are not taking a statin and 4.4m are not receiving antiplatelet therapy.
Lifestyle advice
Education and lifestyle changes should focus on smoking cessation, diet, weight management, moderation of alcohol consumption and regular physical activity (Box 14.2).
Smoking is strongly associated with PAD. Observational studies have shown that mortality and amputation rates are considerably higher, and revascularisation patency rates are much lower, among PAD patients who continue to smoke. In those who are motivated and supported, smoking cessation interventions, e.g. nicotine replacement therapy (NRT), alleviate short-term nicotine withdrawal symptoms and increase long-term quit rates by 2- to 3-fold. Bupropion and varenicline, a nicotine receptor partial agonist, are alternatives to NRT for managing the symptoms associated with abrupt smoking cessation. Varenicline achieves higher quit rates than NRT in randomised trials but is associated with a higher incidence of behavioural or mood changes such as agitation, depression and suicidal thoughts.
The CV benefits of smoking cessation accrue fairly quickly—e.g. up to 50% risk reduction within 1–2 years—whereas the excess cancer risks associated with smoking persist for much longer. Thus, smoking cessation services are very cost-effective for CV risk reduction.
Regular exercise (e.g. brisk 30-min walks three or four times per week) may improve walking distances in patients with PAD but exercise has other metabolic, haemodynamic and CV benefits. The best evidence of the benefits of exercise originates from randomised trials in the context of cardiac rehabilitation.
Lipid-lowering therapy
The Heart Protection study (HPS) demonstrated the benefits of statin therapy (simvastatin 40 mg) in patients with symptomatic PAD and a total-cholesterol level >3.5 mmol/L (Figure 14.2). American Heart Association guidelines (2013) have emphasised the wider CV benefits of cholesterol reduction (e.g. stroke prevention), the superiority and safety of statins over other lipid-lowering drugs, and highlighted the evidence that more intensive statin treatment is better than less intensive treatment to maximise CV risk reduction.
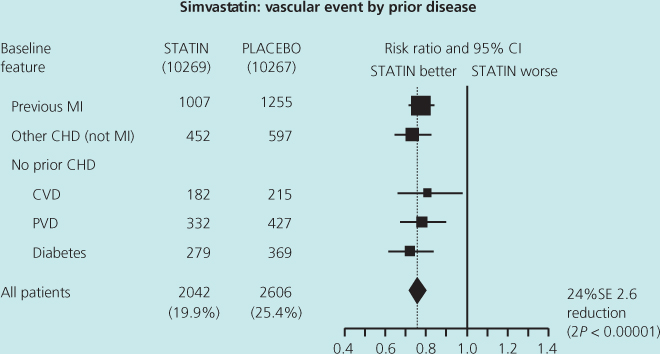
Figure 14.2 The Heart Protection study was a large placebo-controlled trial of simvastatin 40 mg daily in a population of patients treated for primary and secondary prevention with average or low levels of cholesterol (>3.5 mmol/L). The subgroup with known peripheral vascular disease (PVD) at baseline achieved as much benefit from statin therapy as those with prior myocardial infarction. Source: Heart Protection Study Collaborative Group (2002). Reproduced by permission of Elsevier.
Although there is debate about whether statins have non-lipid-mediated (e.g. anti-inflammatory) effects that contribute to their mode of action, in a combined analysis of major statin trials, improvements in CV outcomes were in proportion to the reduction in LDL (low-density lipoprotein)-cholesterol. A subgroup analysis of the 4S study also showed that in patients with PAD statin therapy reduces the incidence of new or worsening claudication.
Target levels of total- and LDL-cholesterol of <4 and <2 mmol/L, respectively, should be used to titrate statin treatment in secondary prevention (Figure 14.3). Monitoring lipid levels is important because fewer than half of the patients will achieve these targets using simvastatin 40 mg daily. Substitution of a more potent statin (e.g. atorvastatin or rosuvastatin), up-titration to simvastatin 80 mg daily or use of additional lipid-lowering treatments, e.g. ezetimibe, may be required in order to achieve optimum LDL-cholesterol reduction. Musculoskeletal aches and pains, and changes in liver function, are the commonest side effects of statin treatment.
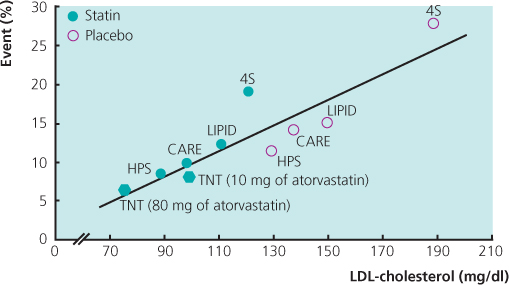
Figure 14.3 This analysis plots the achieved cholesterol level in both the placebo-treated and statin-treated groups in each of the major statin trials against the observed CV event rates, for example, in the 4S, CARE and Heart Protection studies (HPS). It reinforces the notion that lower is better. Data from La Rosa et al. (2005).
Although LDL-cholesterol is the primary measurement used for initiating and titrating lipid-lowering therapy, there is emerging evidence that LDL-cholesterol may not be the best lipid marker to predict CV risk or the anti-atherosclerotic effect of statin therapy. Alternative measurements, in particular, apolipoprotein B (apo-B, which is not routinely measured in most clinical laboratories) and non-HDL (high-density lipoprotein)-cholesterol, have been shown in population studies to be superior to LDL-cholesterol in assessing CV risk (Figure 14.4). Non-HDL-cholesterol is easily calculated by the clinician: total-cholesterol level minus the HDL-cholesterol level. It reflects the sum of serum cholesterol carried by all the atherogenic lipoproteins [i.e. LDL, VLDL (very low-density lipoprotein) and IDL (intermediate-density lipoprotein)] and is valid even in a non-fasting blood sample. The prognostic utility of non-HDL-cholesterol may be particularly good in patients with diabetes.
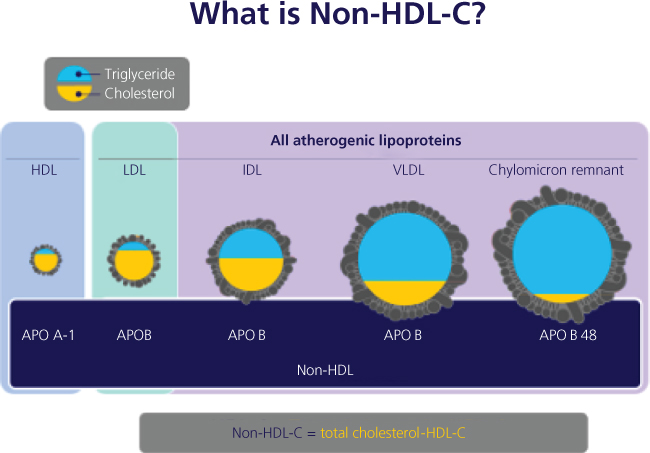
Figure 14.4 Non-HDL-cholesterol is emerging as an important secondary lipid target for use in assessing CV risk and for titration of lipid-lowering therapy. It may correlate more closely with future CV risk.
In a large meta-analysis of statin-treated patients, non-HDL-cholesterol was more strongly associated with risk of future CV events than LDL-cholesterol or apo-B. Thus, non-HDL-cholesterol is likely to emerge as an important secondary target in assessing CV risk and for use in titrating lipid-lowering therapy.
Blood pressure control
Several population studies have reinforced the importance of BP (blood pressure) as an independent risk factor for coronary heart disease, stroke, renal failure and death. In the Framingham Heart study, the risk of intermittent claudication was 2.5- to 4-fold higher among hypertensive patients compared with controls. Furthermore, small differences in BP, maintained over several years, translate into large differences in CV outcomes. Therefore, detecting and treating high BP remains one of the most cost-effective public health interventions to reduce the population incidence of CV disease. Placebo-adjusted treatment effects of around 10/5 mmHg result in 30–40% relative risk reductions in stroke and 15–20% reductions in major coronary disease events.
Several studies have shown that CV end-organ damage associated with hypertension is more strongly correlated with 24-h ambulatory blood pressure (ABP) than with clinic or casual BP measurements (Box 14.3). ABP monitoring requires specialised, validated machines and careful quality control measures. Interpretation of the ABP profile typically includes measurements of mean daytime, night-time (asleep) and 24-h BP. Normal BP values for adults are <135/85 mmHg for daytime, <120/75 mmHg for night-time and <130/80 mmHg for 24-h BP.

Full access? Get Clinical Tree


