Fig. 1
CT scan showing a large mediastinal mass, which is invading the aortic arch, compressing the right lung parenchyma, and constricting the trachea and the esophagus

Fig. 2
CT scan showing an enlarged right upper paratracheal lymph node (station 2R)
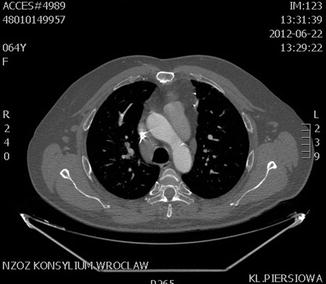
Fig. 3
CT scan showing an enlarged right lower paratracheal lymph node (station 4R)

Fig. 4
CT scan showing a large tumor in the anterior mediastinum, which is invading the posterior wall of the sternum and aortic arch, compressing the right and left lung parenchyma, and constricting the trachea
Negative histological results of mediastinoscopy were obtained in 22 cases (40.8 %). Ten patients did not develop any serious disease, which was confirmed by a positron emission tomography (PET) scans, CT scans, or by further observation (true negative values). Three of these 10 patients underwent a thoracotomy with lymphadenectomy, which proved to be negative. However, 12 patients were discovered to have disseminated cancer, which was confirmed by other diagnostic procedures (false negative values). In our series, the sensitivity of the procedure was 72 %, and the specificity was 100 %.
There were no major complications such as hemorrhaging from major blood vessels. The only minor complication was recurrent laryngeal nerve injury, manifested as prolonged hoarseness of voice, which occurred in three cases (5.5 %). There were no perioperative deaths.
4 Discussion
The role of mediastinoscopy in the evaluation of thoracic disease still remains a debatable subject. Radiological images often do not provide information about the nature of these lesions and consequently fail to enable therapeutic decisions. Surgical exploration of the mediastinum provides a definitive diagnosis as it allows biopsies of lymph nodes or tumors affecting the mediastinum.
The most important question is whether patients with NSCLC will benefit from surgery (Leschber et al. 2008). Mediastinal lymph node involvement (N2 disease), confirming systemic disease, is considered a contraindication for surgery in NSCLC. Mediastinoscopy can obviate an unnecessary thoracotomy. Thoracic CT and PET-CT scans have been widely used for noninvasive tumor staging. Studies have suggested that PET could reduce the need for mediastinoscopy (Hammoud et al. 1999; Vansteenkiste et al. 1998). Invasive mediastinal staging is still necessary as it is based on tissue confirmation. The sensitivity of mediastinoscopy varies between 79 and 93 % (McManus et al. 2008; Fibla et al. 2006). In our series the sensitivity was 72 %. Recently, transbronchial lymph node biopsy by endobronchial ultrasound has been introduced with an approximately 85 % level of sensitivity. The addition of endoscopic ultrasound with fine needle aspiration (EUS-FNA) to mediastinoscopy can increase the sensitivity of detection of mediastinal disease to 93 % (Annema et al. 2010; Annema and Rabe 2006). However, international guidelines regard the surgical staging as the gold standard. It is suggested that endosonography should be followed by mediastinoscopy if no metastases are found (Annema et al. 2010).
The procedure is safe with minimal morbidity. We noticed only three cases of recurrent laryngeal palsy in our series. However, hemorrhage, vocal cord dysfunction, tracheal injury, pneumothorax, and vascular injury are other major complications that have been described in literature (Chauchan et al. 2012; Minowa et al. 2011; Iskender et al. 2011).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


