Cardiovascular disease is the leading cause of death among those with renal insufficiency, those requiring dialysis, and in recipients of kidney transplants reflecting the greatly increased cardiovascular burden that these patients carry. The best method by which to assess cardiovascular risk in such patients is not well established. In the present study, 1,225 patients seeking a kidney transplant, over a 30-month period, underwent cardiovascular evaluation. Two hundred twenty-five patients, who met selected criteria, underwent coronary angiography that revealed significant coronary artery disease (CAD) in 47%. Those found to have significant disease underwent revascularization. Among the patients found to have significant CAD, 74% had undergone a nuclear stress test before angiography and 65% of these stress tests were negative for ischemia. The positive predictive value of a nuclear stress test in this patient population was 0.43 and the negative predictive value was 0.47. During a 30-month period, 28 patients who underwent coronary angiography received an allograft. None of these patients died, experienced a myocardial infarction, or lost their allograft. The annual mortality rate of those who remained on the waiting list was well below the national average. In conclusion, our results indicate that, in renal failure patients, noninvasive testing fails to detect the majority of significant CAD, that selected criteria may identify patients with a high likelihood of CAD, and that revascularization reduces mortality both for those on the waiting list and for those who receive an allograft.
That chronic kidney disease adversely influences cardiac health and function is well established. In 1998, data from the National Center for Health Statistics and from the United States Renal Data System demonstrated that the annual cardiovascular mortality of a dialysis-dependent 25- to 34-year old exceeded that of a 75- to 84-year old in the general population. Cardiovascular disease (CVD) in renal failure patients, however, appears to differ from CVD in the general population. Patients with renal failure are less likely to be symptomatic when experiencing coronary ischemia. Noninvasive testing in this population appears to have poor sensitivity and specificity for the detection of significant coronary artery disease (CAD) and may fail to predict major adverse cardiovascular events (MACEs). Although several studies, in the general population, have failed to demonstrate a survival advantage to revascularization of CAD compared with medical management, the same may not be true in patients with renal failure. Revascularization of coronary artery lesions in patients with end-stage renal disease (ESRD) may significantly improve long-term survival. The purpose of this study was to evaluate the predictive value of noninvasive testing, to determine whether selected criteria would more reliably identify patients with significant CAD, and whether revascularization would reduce mortality while on the waiting list and following transplantation.
Methods
In January 2013, the Kidney/Pancreas Transplant Program at Robert Wood Johnson University Hospital established 6 criteria (listed in Table 1 ) thought to identify patients who were at high risk for underlying CAD. The 559 patients on the transplant waiting list in January 2013 were evaluated. Any patient who met one of the high-risk criteria was referred for coronary angiography. Over the next 30 months, an additional 666 patients seeking a kidney or kidney/pancreas transplant were evaluated. Those who met our criteria were asked to undergo coronary angiography. Of the 1,225 patients evaluated, 225 (18%) met criteria that prompted coronary angiography.
|
Any patient found to have >70% coronary artery occlusion(s) was required to undergo either angioplasty or coronary artery bypass grafting (CABG). When measured, a fractional flow reserve of <0.8 was thought to represent significant coronary artery stenosis.
At the end of the 30-month period, after an Institutional Review Board exemption was obtained, a de-identified retrospective chart review of patients who had undergone a cardiac catheterization, which had been prompted by the established criteria, was performed. The patients with identified significant CAD were compared with those without significant CAD with regard to (1) age, (2) self-identified race, (3) gender, (4) body mass index, (5) the presence and duration of diabetes mellitus, (6) the presence and duration of hypertension, (7) the presence of dyslipidemia, (8) smoking history, (9) the presence of peripheral vascular disease, (10) the presence of carotid artery disease, (11) previous CVA or TIA, (12) previous CAD (CABG and previous myocardial infarction [MI] or percutaneous coronary intervention [PCI]), (13) months on dialysis, and (14) the results of previous stress testing.
Quantifiable data are expressed as mean ± SD throughout the article. Differences between means were compared using Student’s 2-tailed t test. Differences between groups of binomial data were compared by chi-square. A p value <0.05 was considered significant.
Results
Significant CAD was identified in 47% (106 of 225) of patients who underwent a cardiac catheterization. Table 2 compares the characteristics of those with and without significant CAD. Patients with significant CAD were older with a larger percentage being >60 years old. Those with significant CAD were also more likely to be white and male.
| Coronary Artery Disease | |||
|---|---|---|---|
| Variable | Yes (n=106) | No (n=119) | P Value |
| Mean Age ± SD | 59.2 ± 8.5 | 55.2 ± 10.2 | 0.002 |
| Age > 60 Years | 58 (55%) | 45 (38%) | 0.001 |
| White | 50 (47%) | 32 (27%) | 0.002 |
| Black | 31 (29%) | 53 (45%) | 0.02 |
| Hispanic | 8 ( 7%) | 20 (17%) | 0.04 |
| Asian | 12 (11%) | 11 ( 9%) | 0.6 |
| Other | 5 ( 5%) | 2 ( 2%) | 0.2 |
| Male | 87 (82%) | 85 (71%) | 0.02 |
| Female | 19 (18%) | 34 (29%) | |
| BMI (kg/m 2 ) | 30.2 ± 4.5 | 29.3 ± 5.3 | 0.2 |
| Diabetes Mellitus | 89 (84%) | 82 (69%) | 0.01 |
| Years | 19.5 ± 10.1 | 19.2 ± 7.7 | NSS |
| Hypertension | 99 (93%) | 116 (98%) | 0.1 |
| Years | 17.7 ± 11.7 | 14.7 ± 10.5 | 0.06 |
| Dyslipidemia | 74 (70%) | 61 (51%) | 0.005 |
| Smoker | 55 (52%) | 43 (36%) | 0.02 |
| >35 pack years | 15 (14%) | 3 ( 3%) | 0.003 |
| Peripheral Vascular Disease | 13 (12%) | 6 ( 5%) | 0.06 |
| Carotid Disease | 1 ( 1%) | 0 | 0.3 |
| S/P CVA/TIA | 13 (12%) | 13 (11%) | 0.8 |
| Prior Coronary Artery Disease | 49 (46%) | 14 (12%) | 0.00001 |
| Months on Dialysis | 27.9 ± 27.8 | 26.4 ± 31.1 | 0.7 |
Those with significant CAD were more likely to be diabetic, although the duration of diabetes did not differ between the 2 groups. Those with significant CAD were more likely to exhibit dyslipidemia and to have a history of tobacco use, particularly long-standing tobacco use.
There was a trend toward more long-standing hypertension in those with CAD that failed to reach statistical significance (p = 0.06). Our data do not reflect how well controlled the hypertension or diabetes had been. The most significant risk factor for significant CAD was a history of having experienced an MI or of having undergone a PCI or CABG.
Nuclear stress testing results are listed in Table 3 . Patients who met our criteria were asked to undergo cardiac catheterization without undergoing noninvasive testing. Of the 161 patients who underwent a nuclear stress test, 124 were performed before being evaluated at our center. Thirty-seven patients, who did not meet criteria for a cardiac catheterization, underwent a nuclear stress test that was positive for ischemia. Subsequent cardiac catheterization revealed significant CAD in 9 of these patients. Among the 161 patients who had undergone nuclear stress testing, the positive predictive value was 0.42 and the negative predictive value was 0.47.
| Patients with significant coronary artery disease on angiography (n=106) |
| Number undergoing stress test = 78 |
| Number with stress test with reversible ischemia = 27 |
| Number with stress test without reversible ischemia = 51 |
| Positive Predictive Value = 0.42 |
| Patients without significant coronary artery disease on angiography (n= 119) |
| Number undergoing stress test = 83 |
| Number with stress test without reversible ischemia = 45 |
| Number with stress test with reversible ischemia = 38 |
| Negative Predictive Value = 0.47 |
∗ A total of 161 patients underwent a nuclear stress test prior to angiography.
Most patients with significant CAD were revascularized including 18 patients who underwent CABG. Ten patients were either removed from the list or not listed due to severe disease that could not be revascularized. Twenty others were removed from the list when their overall condition worsened. Eleven patients underwent a second cardiac catheterization during this 30-month period. Seven of these repeat angiograms demonstrated significant progression of disease that prompted revascularization.
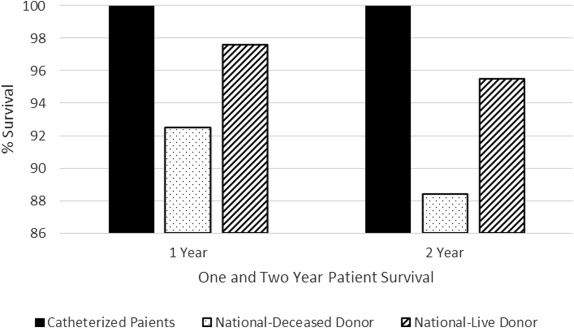
Twenty-eight patients underwent a cardiac catheterization and subsequently received an allograft during this 30-month period. Five patients were transplanted at other centers. As shown in Figure 1 , of the 28 catheterized patients who subsequently received an allograft, none died (or lost an allograft) during this 30-month period. Five of these 28 transplants were from live donors. None experienced an MI.
Of the 55 nondiabetic patients who underwent coronary angiography, none died on the waiting list during these 30 months. Of the 170 diabetic patients who underwent coronary angiography, 9 died while on the waiting list. Six of these patients had ≥1 coronary arteries that were ≥70% occluded. Three of these patients had been revascularized. Of the 3 who were not revascularized, 1 had a fractional flow reserve >0.8 and the other 2 had lesions in vessels that were thought to perfuse a small portion of the myocardium.
Of the 9 deaths while on the waiting list, the cause of death was unknown in 3. One died of sepsis, 1 in a fall, and 1 withdrew from dialysis. Three died of an MI. One had undergone coronary angiography 4 months earlier that revealed mild diffuse disease. One had undergone coronary angiography 23 months earlier and had been found to have an 80% occlusion of a small Ramus vessel. The third patient had undergone coronary angiography 21 months earlier at which time a stent was inserted in the right coronary artery, and there was a 60% to 70% occlusion of the left anterior descending artery that was not revascularized.
In the first year of this study, the mortality on the waiting list of those who had undergone coronary angiography was 1%. Among diabetic patients, mortality was 1.3%. In the second year of this study, the mortality on the waiting list of those who had undergone coronary angiography was 2.4%. Among diabetic patients, mortality was 3.3%. Only 1 death was a cardiovascular death in a patient who had undergone coronary angiography 4 months earlier that revealed mild diffuse disease. As shown in Figure 2 , the mortality rate of the patients on the waiting list in this study was lower than the national average.





