Risk Factors for Heart Failure
Javed Butler
“If you wish to speak to me, you should first define your terms.”
—Master Pangloss to Candide in Voltaire’s Candide
Risk Factor Determination: A Risky Business
Beyond a few high-impact and obvious conditions such as myocardial infarction or hypertension, which clearly are associated with the development of heart failure, determination of risk factors for any disease entity is a difficult task. The literature is filled with claims of risk association between various exposures and disease states that are difficult to prove conclusively. Moreover, these associations are often used for unintended purposes (e.g., medical/legal reasons, publicity, and media attention). A perfect example would be the proposed link between silicone breast implants and the risk for connective tissue diseases in women, a debate that has now been active for over a decade without resolution (1,2).
What strength of association is needed between an exposure and a disease for that exposure to be labeled as a risk factor? How much data do we need to be certain? How many times does it have to be reproduced? These questions are difficult to answer. If the risk factor claim is made hastily, without completely understanding the subtleties and nuances, scientific progress can be delayed for a long time. After all, for several decades beta-blockers were considered to be contraindicated in patients with heart failure! On the other hand, waiting too long for the ultimate confirmation of risky exposures can lead to continuing potentially hazardous exposure and ongoing public health concerns. The cardiovascular risk associated with the use of cyclo-oxygenase II inhibitors, commonly used for arthritis, is an example of such a case. Though the increased risk of cardiovascular disease with their use was first described several years ago, these drugs were not taken off the market until 2005 (3).
Risk factor determination is always a progressive and evolving field as understanding of the disease process broadens and the treatment options evolve. Today’s risk factors may be obsolete tomorrow as either the treatment or patient profiles change over time, or better colinear associations are discovered, rendering any given established risk factor relatively insignificant. In this respect, heart failure presents an even bigger challenge as this condition is a clinical syndrome and not a narrowly defined disease process. Thus, different risk factors may predict the risk for varying aspects of this syndrome, adding to the complexity of risk factor determination.
Difficulties in Assessing Risk Factors for Heart Failure
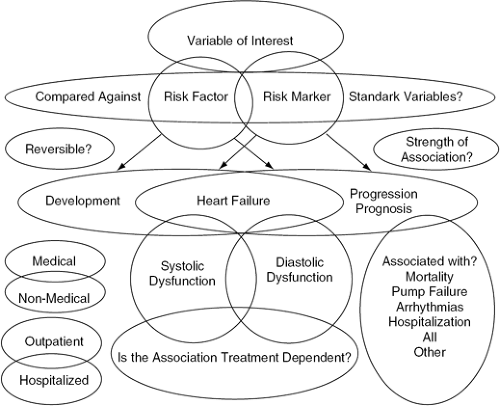
Figure 16-1 gives a general conceptual overview of the difficulties in determining risk factors for heart failure.
Risk Factor or Risk Marker
A correlation between a variable and a disease process may represent a so-called true-true but unrelated epiphenomenon, a marker of disease progression, or a directly contributing pathological relationship to the progression of disease. For example, activation of the renin-angiotensin-aldosterone system (RAAS) is seen with advancing heart failure, and elevated angiotensin II
or aldosterone levels are associated with worse outcomes. Mechanistically, this pathogenic link is plausible considering the role that these neurohormones play in apoptosis, fibrosis, remodeling, and the risk for arrhythmias and pump failure (4,5,6). On the other hand, with advancing heart failure, activation of the natriuretic peptide system is also seen and the levels of B-type natriuretic peptide (BNP), similar to angiotensin II and aldosterone levels, correlate with severity of disease. However, natriuretic peptides are not considered risk factors for heart failure but are markers of severity (7,8). In fact, recombinant natriuretic peptides are used to treat acutely decompensated heart failure. Although this example may be rather clear, the ability to differentiate is not always the case. For example, whether or not C-reactive protein (CRP) is a risk marker or risk factor for progression of coronary artery disease has been debated for many years. We are still awaiting the results of a clinical trial targeting CRP as a therapeutic target to conclude this debate (9,10).
or aldosterone levels are associated with worse outcomes. Mechanistically, this pathogenic link is plausible considering the role that these neurohormones play in apoptosis, fibrosis, remodeling, and the risk for arrhythmias and pump failure (4,5,6). On the other hand, with advancing heart failure, activation of the natriuretic peptide system is also seen and the levels of B-type natriuretic peptide (BNP), similar to angiotensin II and aldosterone levels, correlate with severity of disease. However, natriuretic peptides are not considered risk factors for heart failure but are markers of severity (7,8). In fact, recombinant natriuretic peptides are used to treat acutely decompensated heart failure. Although this example may be rather clear, the ability to differentiate is not always the case. For example, whether or not C-reactive protein (CRP) is a risk marker or risk factor for progression of coronary artery disease has been debated for many years. We are still awaiting the results of a clinical trial targeting CRP as a therapeutic target to conclude this debate (9,10).
Risk for What?
Like most chronic disease, heart failure can present at various stages with a wide spectrum of manifestations. With respect to risk factors and heart failure, the most important aspects of this spectrum are whether a risk factor is related to the development or progression (and, in turn, prognosis) of heart failure. Some risk factors are associated with both (e.g., diabetes), whereas others may be more specific for either development (e.g., certain chemotherapy agents) or progression (e.g., conduction abnormalities) of heart failure. Similarly, risk factors may vary in their importance with respect to different outcomes (e.g., pump failure versus sudden cardiac death).
Type of Heart Failure
Since heart failure is a syndrome and not a specific, single disease entity, another level of complexity is what type of heart failure the risk is associated with. Is the risk factor pertinent to systolic or diastolic dysfunction? Although diastolic dysfunction is less well-studied, there appears to be considerable overlap between risk factors. For example, hypertension is recognized as being a cause of both systolic and diastolic dysfunction. In contrast, excessive alcohol consumption is associated with a higher risk for systolic dysfunction but no such link is currently known for diastolic dysfunction. Similarly, many other forms of heart failure may have unique risk factors (e.g., thiamine deficiencies and risk for high-output heart failure or idiopathic pulmonary fibrosis and risk for isolated right heart failure).
Is the Risk Factor Modifiable?
Another important consideration is whether or not the risk factor is reversible. Many risk factors are of interest from the epidemiological perspective but have no therapeutic value (e.g., age and gender), whereas others are treatable (e.g., dyslipidemia). Similarly, risk factors can be medical (e.g., hypertension) or nonmedical (related to patients’ demographics or lifestyle choices, such as obesity). Usually, the former are more easily treatable.
Is the Risk Factor Treatment-Dependent?
Medical therapy is fast-changing, as is the relationship between risk factors and outcomes. Certain risk factors, such as advancing age, are immune to therapy while others, such as exercise capacity, are not. Several recent reports have suggested
that as prognoses for patients with heart failure have improved with newer therapies and devices, the outcomes for patients with similar peak exercise oxygen consumption level have also improved over time (11,12,13). This is primarily because several of these therapies that improve outcomes do not impact peak exercise oxygen consumption (e.g., betablockers and defibrillators) (14). Thus, the importance of risk factors needs continuous re-evaluation as medical therapy advances.
that as prognoses for patients with heart failure have improved with newer therapies and devices, the outcomes for patients with similar peak exercise oxygen consumption level have also improved over time (11,12,13). This is primarily because several of these therapies that improve outcomes do not impact peak exercise oxygen consumption (e.g., betablockers and defibrillators) (14). Thus, the importance of risk factors needs continuous re-evaluation as medical therapy advances.
Statistical Considerations
Before one can be certain of the association between an exposure and the risk of a disease, there are many statistical considerations that have to be satisfied. For example, the independent prognostic power of any risk factor depends largely on what it is compared against. A very simplistic example would be a statistically higher risk of lung cancer among people who carry matches or lighters with them and, hence, we can conclude that these are risk factors for lung cancer. Obviously this will only be the case if one ignores cigarette smoking in the equation. This is the Achilles’ heel of the literature on risk factor determination. Because different investigators control for a varying array of variables, ranging from none to extensive, in different patient populations the generalizability of such reports is difficult to ascertain. If such results were to be replicated in other studies with different patient populations (e.g., elderly versus middle-aged) or in association with other copredictors, even if such risk factors remain positive, it is almost certain their strength of association would be different. Since the risk factor analysis is important not only from a qualitative perspective but also to quantify outcomes, these statistical considerations cannot be ignored. Similarly, whether the data are validated, what proportion of outcomes are explained by the risk factors, how well the risk factor predicts outcomes across the spectrum of risks, and so forth are all important considerations when determining risk factors.
Practicality and Feasibility
The most important characteristic of a risk factor is whether or not it is clinically useful. For example, cardiac norepinephrine spillover is a strong but clinically irrelevant risk factor. Measurement of plasma norepinephrine, a potent risk factor which can be measured only by an expensive and difficult-to-obtain test, is another example. Simple measurement of heart rate, however, can give significant clues as to the degree of sympathetic activity. Similarly, a detailed history can generally give a reasonable sense whether the peak exercise oxygen consumption is severely or modestly depressed. For decisions such as transplant listing, this may not be enough, but for routine clinical management in the community this may be an adequate way of risk-stratifying patients, especially when used in conjunction with New York Heart Association class symptoms.
In short, there is no single risk factor that is totally accurate or perfect. In order to assess a patient’s risk for development of heart failure or to determine prognosis in patients who already manifest the condition, a careful history and physical examination and measurement of left ventricular function remains the cornerstone. Information obtained from the history and physical should then be used in conjunction with other tests tailored to the patient and the purpose of investigation. This chapter will focus on risk factors for development and progression of heart failure associated with primarily systolic dysfunction as they are seen in the outpatient setting.
Risk Factors for Development of Heart Failure
Table 16-1 gives an overview of risk factors for heart failure development.
Demographics
A higher risk of development of heart failure with increasing age and among males has been consistently shown in the literature (15,16,17,18,19,20,21,22). The higher risk in men may be at least partially related to the greater prevalence of coronary heart disease. Low socioeconomic status has also been associated with an increased heart failure risk (23). Though not clear, the association between low socioeconomic status and the risk for heart failure may be related to poor access to health care, compliance issues, or a higher prevalence of other heart failure risk factors (24,25).
Lifestyle-Related
Alcohol Consumption
Relationship between alcohol abuse and development of heart failure is well-known (26,27). This may be related to both the direct myocardial toxicity of alcohol and the higher risk of hypertension development with excessive alcohol use (28,29,30). However, some data suggest that moderate alcohol consumption may lower the risk of heart failure development (31). This may be related to the lower risk of diabetes, myocardial infarction, and favorable changes in the lipid profile, platelet function, and blood clotting associated with moderate alcohol intake (32,33,34,35,36).
Tobacco and Coffee Consumption
Data regarding the risk for heart failure development with smoking (after controlling for other risk factors) are conflicting (23,37,38). Theoretically, such a relationship is conceivable as smoking is associated with abnormalities that, in turn, increase heart failure risk (e.g., insulin resistance, endothelial dysfunction, oxidative stress, and possible direct myocardial toxicity) (39,40,41,42). Similarly, excessive coffee intake has been associated with an increased risk of heart failure (38).
Dietary Sodium Intake
An association between excessive dietary salt intake and risk for heart failure has been reported (43). This may be related to ventricular function abnormalities, hypertension,
development of left ventricular hypertrophy, or water retention associated with excessive salt intake (43,44,45,46,47).
development of left ventricular hypertrophy, or water retention associated with excessive salt intake (43,44,45,46,47).
Table 16-1 Risk Factors for Development of Heart Failure | |||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Recreational Drug Use
Cocaine abuse has been associated with development of heart failure. This has been shown in both acute and chronic settings. It may be related to either development of premature coronary disease, vasospasm, or cocaine’s effect on cardiac contractility (48,49,50). Other agents, particularly methamphetamines, have also been associated with increased heart failure risk.
Biochemical Markers
Albuminuria
In the Heart Outcomes Prevention Evaluation study, presence of microalbuminuria was associated with a threefold increase in the risk of heart failure hospitalization (51). Microalbuminuria is associated with other cardiovascular risks such as hypertension, ventricular hypertrophy, and serum acute phase reactants, which may be important in heart failure development (52,53,54).
Homocysteine
The Framingham Heart Study has shown that elevated plasma homocysteine levels are associated with almost a 75% increase in risk for heart failure development (55). This may be related to the link between high homocysteine serum levels and oxidative stress and cardiac fibrosis, endothelial dysfunction, and coronary atherosclerosis—all factors important in development of heart failure (56,57,58,59).
Tumor Necrosis Factor-α
In recent analyses, after adjustment for other risk factors, every tertile increment in tumor necrosis factor-α (TNF-α) levels was associated with a 60% increase in risk of heart failure (60). TNF-α is a proinflammatory cytokine produced by myocardial macrophages and is associated with myocardial dysfunction and cell death (61). TNF-α has several negative pleiotropic effects and also negative inotropic properties that may be responsible for excessive heart failure risk (62,63); it is also associated with progression of heart failure (64).
Interleukin-6
Similar to TNF-α, interleukin-6 (IL-6) is also a proinflammatory cytokine associated with an excessive risk of development of heart failure (60). Both of these cytokines are associated with ventricular remodeling, fetal gene expression, and myocyte hypertrophy and apoptosis (65). In transgenic mice models, overexpression of IL-6 and its receptor has been associated with left ventricular dilatation (66).
C-Reactive Protein
Data from the Framingham Heart Study also suggest that an increase in CRP level by 5 mg/dL is associated with a greater than twofold increased risk of heart failure, and subjects who simultaneously also had elevated serum IL-6 and TNF-α values had a fourfold increase in risk (60). Whether this increased risk is due to high CRP levels and atherosclerosis risk or through activation of other proinflammatory cytokines is not known.
Insulin-Like Growth Factor-I
Insulin-like growth factor-I (IGF-I) is expressed in various tissues and has been shown to have a positive inotropic effect; it also decreases the rate of apoptosis (67,68). IGF-I
may also cause vasodilation, decreasing impedance to cardiac emptying (69). Data from the Framingham Heart Study have linked a serum IGF-1 level below 140 mg/L with a doubling of the risk of heart failure development (70).
may also cause vasodilation, decreasing impedance to cardiac emptying (69). Data from the Framingham Heart Study have linked a serum IGF-1 level below 140 mg/L with a doubling of the risk of heart failure development (70).
Natriuretic Peptides
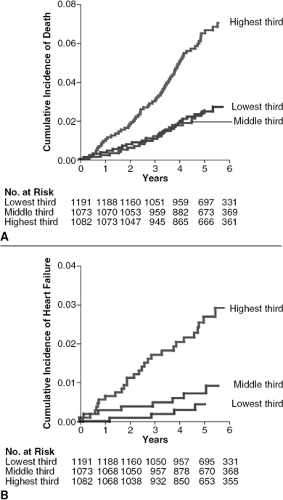
In the Framingham Heart Study, increased levels of plasma BNP and N-terminal atrial natriuretic peptide (N-ANP) were associated with an increased risk of heart failure. As shown in Figure 16-2, BNP levels above the 80th percentile (20 pg/mL for men and 23.3 pg/mL for women) were associated with a threefold increase in heart failure risk (71). BNP and N-ANP are secreted by the cardiac myocytes in response to stretch and have several beneficial physiological effects (72,73). The increased risk for heart failure related to elevated natriuretic peptides is not readily explained. However, this association may be due to the presence of subclinical heart failure, which results in elevation of these hormones.
Echocardiographic Parameters
Asymptomatic dilatation of the left ventricle, along with increases in left end-diastolic or end-systolic diameter, has been linked to a higher risk of developing heart failure (74). Similar to elevated natriuretic peptides, whether or not this represents the initial stages of left ventricular dysfunction is unknown. One may also include in this category asymptomatic left ventricular dysfunction as a risk factor for developing the syndrome of heart failure (75). Increased left ventricular mass, which is a correlate of left ventricular hypertrophy as assessed by electrocardiogram, is also related to a higher risk for heart failure development (76). Finally, multiple left ventricular diastolic filling abnormalities, such as alterations in the E/A wave ratio, have been associated with a higher heart failure risk (76). These different echocardiographic parameters may act in concert to predict the risk and may be related to the activation of the neurohormonal axis in patients with cardiac structural changes, even in the absence of symptoms (77).
Comorbidities
Hypertension
There is perhaps no better-documented risk factor for predicting the future risk for heart failure development than hypertension, which confers a two- to threefold higher risk (16,17,18,19,20,21,78). All three components of hypertension (systolic, diastolic, and pulse pressure) have been associated with this higher risk (79,80). Interestingly, the risk of developing heart failure related to a wide pulse pressure is not completely explained by either systolic hypertension or diastolic pressure lowering by medications, suggesting that a combination of elevated systolic and reduced diastolic pressures may confer additional risk related to increased pulse pressure (79). The mechanism by which hypertension confers the risk for development of heart failure is well-described in the literature and is related to myocyte hypertrophy, increased fibrosis, reduced contractile proteins, eventual neurohormonal activation, and, ultimately, remodeling of the ventricle (81,82,83). It is therefore not surprising that treatment of hypertension substantially reduces the risk of heart failure development, although different drugs may have varying effect, including higher risk with the use of doxazosin (84,85).
Myocardial Infarction
Similar to hypertension, myocardial infarction is a well-known risk factor for heart failure in terms of its overall association, but it confers a much higher magnitude of risk (on the order of 15-fold or more) (16,17,18,19,20,21). Therefore, myocardial infarction can be considered the most potent risk factor for heart failure. Also, similar to hypertension, the mechanisms of development of heart failure after an infarction are complex and include cellular slippage, dilatation of the infracted area, subsequent hypertrophy of the unaffected myocytes, excess collagen deposition and fibrosis, apoptosis, and, ultimately, systemic neurohormonal activation and its subsequent consequences (86).
Left Ventricular Hypertrophy
Left ventricular hypertrophy on electrocardiogram, independent of hypertension, is associated with a higher risk of heart failure (87). On a relative scale, this risk appears to be higher in younger subjects than older. The increased risk is likely mediated through multifactorial mechanisms, including a direct effect on myocardium in terms of increased oxygen demand and reduced coronary reserve, higher risk of apoptosis, and also (indirectly) by increasing the risk of coronary artery disease and myocardial infarction (88,89,90). Regression of left ventricular hypertrophy with medication is associated with an overall reduction of risk for cardiovascular outcomes, and it probably also leads to a reduction in the risk for heart failure (91).
Valvular Heart Disease
Various cardiac valvular abnormalities are associated with an increased risk of heart failure development (92). Whether this presents in the form of pressure overload (e.g., aortic stenosis) or volume overload (e.g., mitral regurgitation), the initial compensatory mechanisms, such as hypertrophy or ventricular dilatation, eventually affect contractility and development of heart failure (93). Timely surgical intervention can substantially improve cardiac function and reduce the risk for heart failure (94).
Diabetes Mellitus
Diabetes mellitus, especially in women and in patients with asymptomatic left ventricular dysfunction, has been associated with a three-to fivefold increased risk of developing heart failure (17,18,19,20,95,96). This excess risk may be related to accelerated atherosclerosis, endothelial dysfunction, microvascular diseases, and autonomic dysfunction associated with diabetes (97). Even a modest increase of 1% in glycosylated hemoglobin (HgbAlc) leads to a >10% risk of heart failure hospitalization or death (98).
Overweight
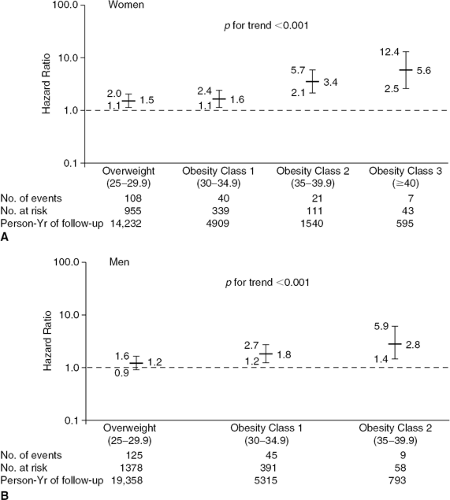
Although debated for some time, being overweight or obese is now a well-established risk factor for heart failure (99). As shown in Figure 16-3, for both men and women there is a worsening gradient for adverse outcomes with increasing body mass index (BMI). This relationship was seen even after adjusting the data for differences in groups with respect to age, lipid levels, smoking and alcohol consumption, and history of hypertension, diabetes, and myocardial infarction. Similar to diabetes, elevated BMI tends to be associated with other high-risk vascular disease traits, but obesity is also associated with potential changes in cardiac structure and function, neurohormonal changes, preload and afterload, and other comorbidities such as renal diseases. Whether this risk is reversible or not has not been elucidated.
Lipid Abnormalities
Hypertriglyceridemia and an increased total cholesterol to high-density lipoprotein (HDL) level are associated with a higher risk of heart failure (100). This may be related to increased atherosclerotic cardiovascular diseases, left ventricular hypertrophy, or cardiac function abnormalities seen in patients with dyslipidemias (101,102). Interestingly, in at least one controlled clinical trial in patients with coronary artery disease, lipid lowering was associated with a 21% reduction in the risk of developing heart failure (103).
Renal Insufficiency
Elevated serum creatinine (1.5 mg/dL in men and 1.3 mg/dL in women) or reduced creatinine clearance (less than 60 mL/minute) is related to a higher risk for newonset heart failure, even after adjusting for traditional risk factors for heart failure; this risks tends to increase with worsening renal function (104). However, even milder degrees of renal insufficiency are also associated with a progression of asymptomatic systolic dysfunction to symptomatic heart failure (105). Many pathophysiological changes that occur in patients with renal insufficiency can contribute to this excess risk, including hypervolemia, oxidative stress, neurohormonal and cytokine activation, anemia, hypertension, and abnormalities in coagulation cascade (106,107,108,109).
Sleep-Disordered Breathing
In both humans and animals, sleep-disordered breathing is associated with a risk for heart failure (110,111,112). In an epidemiological study consisting of a survey of over 6,400 individuals, the presence of an apnea-hypopnea index (AHI) was associated with a greater than twofold increased risk of heart failure (113). The physiological basis for this increased risk is complicated. Apnea can lead to negative swings in intrathoracic pressure, in turn leading to increase in afterload. A reduced oxygen level and an elevated carbon dioxide level can increase sympathetic activation (114). Hypoxiainduced pulmonary vasoconstriction and increased right ventricular pressure may compromise left ventricular filling. Obstructive sleep apnea also elevates sympathetic activity and hypertension, leading to a higher heart failure risk (115,116). Treatment of sleep apnea in smaller studies has
been associated with improved outcomes in terms of reduction in blood pressure and sympathetic activity and improved left ventricular function (117,118).
been associated with improved outcomes in terms of reduction in blood pressure and sympathetic activity and improved left ventricular function (117,118).
Tachycardia
Tachycardia-induced cardiomyopathy is a well-known entity. In the Framingham Heart Study, a 10-beats-per-minute increase in heart rate was associated with a >10% higher risk for heart failure development (92). Whether this represents existing left ventricular dysfunction and tachycardia in compensation to reduced stroke volume or inappropriate activation of the neurohormonal system is not known.
Pulmonary Function Abnormalities
Data regarding pulmonary function abnormalities and development of heart failure are conflicting. Forced vital capacity and forced expiratory volume in the first second have been associated with an increased risk in some but not other studies (16,119). The most difficult aspect of ascertaining the relationship between heart failure risk and abnormal pulmonary function is the potential for misclassification based on symptoms. However, pulmonary abnormalities are associated with other high-risk cardiovascular diseases and structural cardiac abnormalities, and a direct link is possible (120,121).
Depression and Stress
Social and emotional factors are known to precipitate hospitalization among heart failure patients (122). Depressed elderly patients have been shown to have a twofold higher risk of developing heart failure (123). Gender differences, with a higher risk in women as compared to men, have been described in the literature (124). Although a greater part of this excess risk may be attributable to compliance, an association between stress and depression with sympathetic activation, arrhythmias, and immune system modulation has been described (125,126,127,128). Whether treatment of depression prevents the development of heart failure is not known.
Pharmacological Risk Factors
Chemotherapeutic agents such as doxorubicin and cyclophosphamide can cause myocardial damage, which results in left ventricular dysfunction and heart failure (129,130). This risk exists not only in the acute treatment phase but also may occur several months after the exposure to these agents; there generally tends to be a higher risk with increasing cumulative dose (131,132). The heart failure risk associated with the antihypertensive agent doxazosin has been described earlier. Although the link between new-onset heart failure with nonsteroidal antiinflammatory drugs (NSAIDs) is now clear, in patients on diuretic therapy the use of these agents has clearly been shown to worsen the risk of heart failure hospitalization. This may be related to alterations in renal function or inhibition of prostaglandin synthesis and resulting sodium and water retention (133,134). Finally, the association between use of thiazolidinediones and decompensation of heart failure requiring hospitalization has been challenged based on the potential benefit of insulin sensitization in the heart failure patient. There is currently an ongoing trial assessing the careful use of these agents in patients with heart failure, and additional data are needed to clarify the role of these drugs (135).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree