Right Ventricular Function and Pulmonary Hemodynamics
Suzanne V. Arnold
High-Yield Findings
Right ventricular size should be ≪ left ventricular (LV) size
RV dysfunction—decreased tricuspid valve (TV) annular motion, RV outflow duration ≪ TR duration
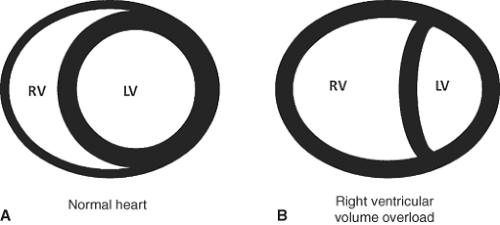
RV pressure overload—systolic interventricular septal flattening, high-velocity tricuspid regurgitant (TR) jet, short right ventricular outflow tract (RVOT) acceleration time, RVOT outflow notching
RV volume overload—diastolic interventricular septal flattening, severe pulmonic regurgitation (PR)
Right atrial (RA) pressure increase—dilated inferior vena cava (IVC), interatrial septal bowing to left
Key Views
Parasternal long axis and RV inflow—initial screening of RA/RV size and TR jet
Parasternal short axis—assessment of interventricular septal flattening, TR jet, RVOT outflow pattern, PR jet
Apical four chamber—best view for RA/RV size, qualitative RV function, tricuspid valve (TV), annular motion, TR jet, interatrial septum
Subcostal—assessment of RVH and IVC
Anatomy and Physiology of the Right Ventricle
The RV is fundamentally different from the LV in both structure and function such that methods typically used to assess the LV do not work for the RV.
The RV is a thin-walled pyramidal structure that “wraps around” the LV. The RV is divided into two sections: Inflow (TV, papillary muscles, chordae tendinae, myocardium) and outflow (conus or infundibulum and pulmonic valve [PV]). Additional structures unique to the RV: Crista supraventricularis, prominent trabeculations, moderator band.
In contrast to the LV, the RV is highly compliant and energetically-efficient; designed to pump blood into the low-resistance, high-capacitance pulmonary circulation. The RV is less capable of maintaining stroke volume in the setting of acute increases in afterload.
The RV contracts by three separate mechanisms: Inward movement of the free wall to the interventricular septum (i.e., “bellows” motion: This allows for a large volume shift with little transverse motion), contraction of longitudinal fibers, and traction on the free wall due to LV contraction. This method of contraction is fundamentally different than that of the LV. The main driving force of the LV comes from a layer of circumferential constrictor fibers that act to reduce ventricular diameter. The RV lacks these fibers and thus must rely more heavily on longitudinal shortening than does the LV. In addition, although the RV does undergo torsion, this does not contribute substantially to RV contraction.
The RV and LV are interdependent, with common encircling muscle fibers, a shared interventricular septum, and the pericardium. It is estimated that ∼65% of RV pressure and volume outflow are generated by the LV.
RV Size and Function
2D Assessment
Important to assess in patients with pulmonary embolism, pulmonary hypertension, RV infarction, LV assist devices, congenital heart disease.
The RV is a complex 3D shape and unlike the LV is difficult to model with a single 2D echocardiographic view. Therefore multiple views should be assessed before determining that RV enlargement is present.
Qualitative: A standard apical four-chamber (A4C) view is best to assess RV size as compared to LV.
Mildly enlarged: RV is enlarged but <LV
Moderately enlarged: RV ≈ LV
Severely enlarged: RV > LV. Apex of heart comprised of RV
Quantitative:
PLAX RVOT proximal diameter >3.3 cm
PSAX RVOT distal diameter >2.7 cm
Apical four-chamber RV basal diameter in diastole >4.2 cm
As RV enlarges, it assumes more of a spherical shape and can impair LV output (Fig. 5-1).
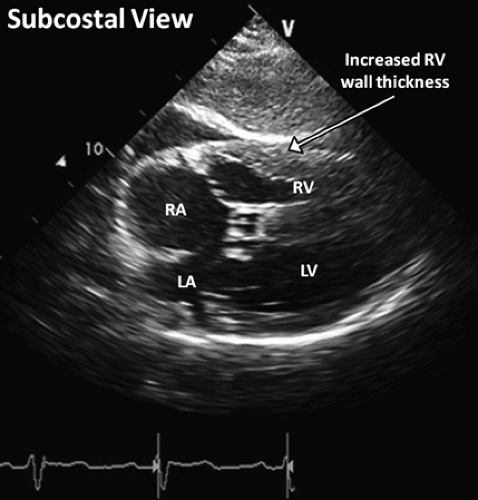 Figure 5-2. A subcostal image showing clear delineation of the borders of the hypertrophied RV wall. For accurate measurement, a zoomed 2D view or M-mode should be acquired. |
Key Point:
It is critical that qualitative assessment of RV size be made in standard transducer locations. If the transducer is placed too medially in the apical four-chamber view, the RV will always appear larger.
M-mode Assessment
RV wall thickness measured at peak of R wave on electrocardiogram at level of TV chordae in subcostal view (normal ≤5 mm) (Fig. 5-2).
As RV systolic function primarily relies on longitudinal myocardial shortening, measurement of tricuspid annular plane systolic excursion (TAPSE) can be used. In the apical four-chamber view, an M-mode cursor is oriented to the junction of the TV plane with the RV free wall. TAPSE is the difference in the displacement of the RV base during diastole and systole. Abnormal excursion <1.7 cm (low sensitivity but high specificity) (Fig. 5-3).
Doppler Assessment
RV function can be assessed by the myocardial performance index (MPI) or Tei index, which is the ratio of isovolumic time to ventricular ejection time. It is a measure of both systolic and diastolic function. For this measurement the TR jet duration (CW Doppler) and RVOT jet duration (PW Doppler) are
recorded. Since TR occurs from a high to low pressure chamber (i.e., RV → RA), flow is holosystolic—including isovolumic contraction and relaxation times. Thus, to determine isovolumic time, subtract ejection time from TR duration (Fig. 5-4).
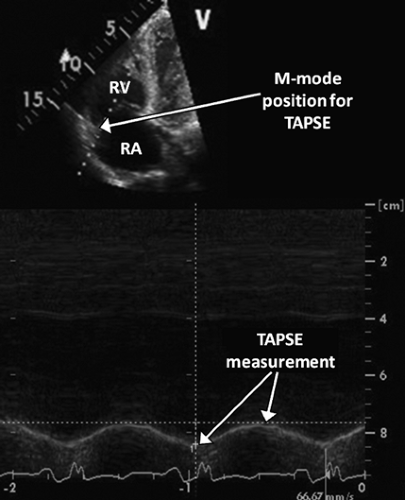
Figure 5-3. Using M-mode positioned from the RV apex through the RV free wall and tricuspid annulus intersection to measure TAPSE.
MPI = (isovolumic contraction time [IVCT] + isovolumic relaxation time [IVRT])/ejection time; IVCT + IVRT = TR time – RVOT ejection time.
MPI = (TR time – RVOT ejection time)/RVOT ejection time
Normal <0.4. Value increases with systolic and diastolic RV dysfunction.
Tissue Doppler imaging can also be used for quantitative assessment of RV systolic function. Systolic tissue Doppler signal of the lateral TV annulus (Sa) <10 cm/s suggests RV dysfunction (Fig. 5-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree