Right Ventricular Disease and Pulmonary Hypertension
Dimitrios Maragiannis
Sherif F. Nagueh
1. Which of the following is true about hepatic vein Doppler pattern in patients with severe tricuspid regurgitation?
A. In severe tricuspid regurgitation during sinus rhythm, hepatic vein Doppler always shows a prominent systolic flow reversal wave.
B. In severe tricuspid regurgitation during sinus rhythm, systolic flow reversal wave peaks in late systole.
C. In the absence of severe tricuspid regurgitation, systolic flow reversal may occur in the setting of right ventricular dysfunction.
D. None of the above.
E. B and C.
View Answer
1. Answer: E. In severe tricuspid regurgitation during sinus rhythm, hepatic vein Doppler typically shows a prominent, late peaking systolic flow reversal wave. However, systolic flow reversal may also occur in the setting of right ventricular dysfunction. Of note, blunting of the forward flow systolic wave rather than systolic flow reversal may occur in patients with severe TR and a large, compliant right atrium.
2. Which of the following Doppler parameters can be supportive of tricuspid mechanical valve stenosis?
A. A prolonged pressure half time (PHT).
B. An elevated mean gradient and/or velocity.
C. TVIprosthesis/TVILVOT ratio <1.5.
D. A and B.
View Answer
2. Answer: D. A PHT ≥230 ms can identify a stenotic bileaflet tricuspid mechanical valve. However, rounded spectral Doppler contours are not infrequent and PHT cannot be measured in these cases. In the absence of high output states (anemia, hyperthyroidism, sepsis) the elevated mean gradient ≥6 mm Hg and/or an elevated velocity >1.7 m/s are supportive diagnostic parameters of tricuspid prosthetic valve stenosis. No data on TVIprosthesis/TVILVOT ratio are available in current guidelines.
3. A patient is reported to have severe right ventricular diastolic dysfunction with a restrictive filling pattern. Which echocardiographic findings support this diagnosis?
A. A tricuspid E/A ratio <2.1 with a deceleration time >120 ms.
B. A tricuspid E/A ratio >2.1 with a deceleration time <120 ms.
C. No diastolic antegrade flow in the pulmonic artery.
D. None of the above.
E. All of the above.
View Answer
3. Answer: B. Tricuspid E/A ratio >2.1 with a deceleration time <120 ms are consistent with right ventricular restrictive filling in patients with RV disease. Latediastolic antegrade flow in the pulmonary artery also suggests increased right ventricular diastolic pressure.
4. Which patient has the highest right atrial pressure (RAP)?
A. IVC maximum diameter at 1.8 cm and minimum diameter with sniffing at 0.8 cm.
B. IVC maximum diameter at 2.1 cm and minimum diameter with sniffing at 0.9 cm.
C. IVC maximum diameter at 1.9 cm and minimum diameter with sniffing at 1.3 cm.
D. IVC maximum diameter at 2.3 cm and minimum diameter with sniffing at 1.0 cm.
E. IVC maximum diameter at 1.5 cm and minimum diameter with sniffing at 0.7 cm.
View Answer
4. Answer: C. The normal diameter of IVC is ≤2.1 cm and decreases by at least 50% with inspiration during sniffing. Thus patients in choices A and E have the lowest RAP (0-5 mm Hg). When the IVC is dilated but collapses by at least 50%, RAP is estimated at 5-10 mm Hg. In the presence of a normal diameter but with less than 50% collapse (assuming good effort during sniffing), RAP is usually between 10 and 15 mm Hg. When the IVC is both dilated with less than 50% collapse, RAP is estimated at 15-20 mm Hg (Table 28-1).
5. Which of the following is characteristic of RV structure and function in patients with longstanding arrhythmogenic RV dysplasia (ARVD)?
A. RV regional dysfunction in RVOT and apical segments.
B. RV fractional area change of 50%.
C. Tricuspid regurgitation (TR) jet by continuouswave Doppler of 3.6 m/s.
D. Left ventricular (LV) ejection fraction (EF) of 26%.
View Answer
5. Answer: A. In this cardiomyopathy, there are frequent abnormalities in RV regional and global function. The regional dysfunction is commonly noted in the RVOT, apex, and basal RV free wall in the region of the “triangle of dysplasia.” RV dilatation and depressed global systolic function also occur, though not in all patients early on. In one study, dilatation of the RVOT was noted in all patients with ARVD and may occur as an isolated finding. Other abnormalities include abnormally bright moderator band, RV sacculations (or diastolic outpouchings), aneurysm (systolic outpouchings), and trabecular derangements. LV EF is characteristically normal in most patients with ARVD although infrequently a left-sided cardiomyopathy may occur. Given the presence of RV systolic dysfunction, PA pressures are usually normal and not elevated. Therefore, a peak TR velocity of 3.6 m/s is not consistent with ARVD.
Table 28-1. Summary of RAP Estimation Using IVC Collapse Index and Hepatic Venous Flow | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
6. Which of the following tissue Doppler velocities is expected in a 36-year-old patient with primary pulmonary hypertension of 4-year duration?
A. Septal mitral annulus systolic velocity of 16 cm/s.
B. Lateral mitral annulus early-diastolic velocity of 14 cm/s.
C. Septal mitral annulus early-diastolic velocity of 13 cm/s.
D. Tricuspid annulus systolic velocity of 15 cm/s.
E. Tricuspid annulus early-diastolic velocity of 13 cm/s.
View Answer
6. Answer: B. RV systolic and diastolic functions are depressed in patients with pulmonary hypertension. Because of the RV contribution to septal function, both septal systolic and diastolic mitral annulus tissue Doppler velocities are reduced. Likewise, tricuspid annulus velocities at the lateral side of the tricuspid annulus are reduced in these patients. On the other hand, LV function is preserved, and early-diastolic velocities at the lateral side of the mitral annulus are usually normal.
7. Which of these is an abnormal finding?
A. Predominant forward hepatic vein diastolic flow in a 25-year-old man.
B. A hepatic vein atrial reversal velocity of 20 ms duration.
C. A tricuspid E/A ratio of 1.8 in a 34-year-old woman.
D. A hepatic vein systolic velocity to diastolic velocity ratio of 0.3 in a 70-year-old man.
E. Hepatic vein midsystolic reversal velocity of 15 cm/s.
View Answer
7. Answer: D. The flow in the hepatic veins is largely determined by RAP during the cardiac cycle (see Table 28-1). In normal subjects, antegrade flow from the hepatic veins to the RA occurs in systole (S) and diastole (D). With RA contraction, brief retrograde late-diastolic flow (Ar), as well as late systole flow (Vr), occurs into the hepatic veins. It is feasible to record high-quality signals by transthoracic imaging from the subcostal window in most ambulatory patients. Hepatic vein flow velocities can be used to asses RAP. In general, a lower proportion of forward systolic flow is indicative of increased RAP, except in healthy young subjects where this finding is normal. Similar to mitral inflow, young subjects have an E/A ratio that is >1 with a short deceleration time (DT), and reduced RA contribution to RV filling.
8. In which of the following cases may hepatic venous flow predict RA pressure?
A. A 55-year-old man with middiastolic rumble/holosystolic murmur at the lower left sternal border.
B. A 61-year-old woman with postoperative dyspnea and paradoxical pulse.
C. A 65-year-old man with a heart rate of 40 beats/min after bypass surgery and cannon “a” waves in his jugular venous pulse.
D. A 53-year-old man with low-voltage EKG, postural hypotension, and LV posterior wall thickness of 18 mm.
E. A 45-year-old man who received a heart transplant 6 months ago.
View Answer
8. Answer: D. There are limitations to using hepatic venous flow to predict RAP. These include the presence of tricuspid valve stenosis or regurgitation, pericardial compression syndromes, high-grade AV block, and heart transplants. The presence of a restrictive cardiomyopathy is not a limitation. Option A is consistent with tricuspid stenosis/regurgitation. Option B is consistent with a postoperative pericardial compression syndrome. The patient in option C has high-grade heart block, and option E is a heart transplant. The presentation in D is consistent with amyloid where the patient has cardiac disease and peripheral neuropathy.
9. Which of the following is compatible with advanced RV disease in patients with cardiac amyloidosis?
A. RV free wall thickness of 7 mm.
B. Deceleration time of tricuspid E velocity of 260 ms.
C. Tricuspid E/A ratio of 1.
D. A hepatic venous systolic velocity to diastolic velocity ratio of 0.6.
E. Inspiratory hepatic venous atrial flow reversals.
View Answer
9. Answer: E. With advanced RV disease in patients with cardiac amyloidosis, RV free wall thickness is >7 mm, and tricuspid inflow shows a restrictive filling pattern. Hepatic venous flow at this stage is characterized by reduced forward systolic flow, increased forward diastolic flow, and inspiratory diastolic atrial flow reversal.
10. What is the pulmonary artery (PA) systolic pressure in a patient with a peak TR velocity of 3 m/s and a jugular venous pressure of 15 cm?
A. PA systolic pressure = 51 mm Hg.
B. PA systolic pressure = 36 mm Hg.
C. PA systolic pressure = 46 mm Hg.
D. PA systolic pressure = 40 mm Hg.
View Answer
10. Answer: C. PA systolic pressure is given by 4(VTR)2 + RAP. A jugular venous pressure of 15-cm water corresponds to 15 × 0.7 or 10-11 mm Hg, since 1-cm water corresponds to 0.7 mm Hg. Accordingly, PA systolic pressure is given by 4(3)2 + 10, or 46 mm Hg.
11. Which of these patients has the highest pulmonary vascular resistance?
A. TR jet of 3.6 m/s and time velocity integral of RVOT systolic flow of 13 cm.
B. TR jet of 3.3 m/s and time velocity integral of RVOT systolic flow of 13 cm.
C. TR jet of 3.6 m/s and time velocity integral of RVOT systolic flow of 18 cm.
D. TR jet of 3.5 m/s and time velocity integral of RVOT systolic flow of 14 cm.
View Answer
11. Answer: A. Pulmonary vascular resistance (PVR) is derived invasively as: (mean PA pressure – wedge pressure)/cardiac output. It can be estimated noninvasively by using the ratio between peak velocity of TR jet (as a surrogate of PA pressure), and time velocity integral of RVOT systolic flow (as a surrogate of cardiac output). Options A and C have the highest peak velocity, while option A has the least time velocity integral of RVOT systolic flow.
12. What is the mean PA pressure in this patient with TR peak velocity of 3 m/s, pulmonary regurgitation (PR) end-diastolic velocity of 2 m/s, and RA pressure of 10 mm Hg?
A. Mean PA pressure = 26 mm Hg.
B. Mean PA pressure = 21 mm Hg.
C. Mean PA pressure = 33 mm Hg.
D. Mean PA pressure = 40 mm Hg.
View Answer
12. Answer: C. Mean PA pressure is given by PA diastolic pressure + 1/3 pulse pressure or (PA systolic pressure + 2 × PA diastolic pressure)/3. This patient has a PA systolic pressure of 4(3)2 + 10 or 46 mm Hg. PA diastolic pressure = 4(2)2 + 10 or 26 mm Hg. Pulse pressure is given by 46 – 26 or 20 mm Hg. Accordingly, mean PA pressure = 26 + (20/3), or 33 mm Hg. Mean PA pressure can also be estimated using the regression equation: 80 – 0.5 (acceleration time) of the RVOT pulsed Doppler velocity.
13. What is the PA systolic pressure of this patient with pulmonary stenosis, where peak TR velocity is 4 m/s, peak velocity across pulmonic valve is 3 m/s, and RA pressure is 10 mm Hg?
A. PA systolic pressure = 46 mm Hg.
B. PA systolic pressure = 74 mm Hg.
C. PA systolic pressure = 38 mm Hg.
D. PA systolic pressure = 50 mm Hg.
View Answer
13. Answer: C. RV systolic pressure is given by 4(VTR)2 + RAP, where VTR is the peak velocity of the TR jet. Therefore, RV systolic pressure = 64 + 10, or 74 mm Hg. The gradient between RV systolic pressure and PA systolic pressure is given by RV systolic pressure – PV systolic pressure = 4(VPV)2, where VPV is the peak velocity across the pulmonary valve. Therefore, PA systolic pressure = 74 – 36, or 38 mm Hg.
14. Which of these supports the diagnosis of increased RV systolic pressure?
A. Acceleration time of 120 ms in systolic flow recorded at RVOT.
B. Pulmonary regurgitation (PR) peak velocity of 1.5 m/s, and RA pressure of 5 mm Hg.
C. TR peak velocity of 3.5 m/s.
D. Flat interventricular septum during diastole only.
View Answer
14. Answer: C. Mean PA pressure can be estimated using the regression equation: 80 – 0.5 (acceleration time). Therefore, the patient in option A is predicted to have a mean PA pressure of 20 mm Hg, which is normal. Mean PA pressure can also be estimated using the peak velocity of PR to which an estimate of right ventricular end-diastolic pressure (RVEDP), or RAP, is added. Therefore, the mean PA pressure in option B can be predicted to be: 4(1.5)2 + 5 or 14 mm Hg, which is normal. In option C, the peak systolic pressure is at least: 4(3.5)2, or 49 mm Hg, which is consistent with pulmonary hypertension. With increased RV systolic pressure, a D-shaped septum is present in both systole and diastole, and not only during diastole.
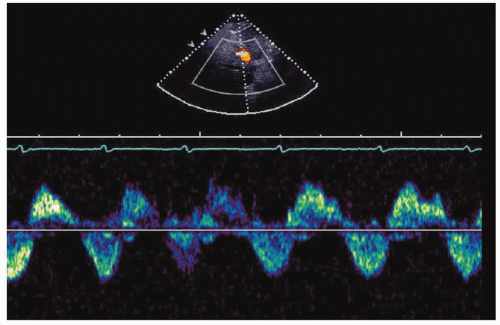
15. Which of the following is most compatible with the hepatic venous flow in Figure 28-1?
A. A 56-year-old man with systemic hypertension under control with medical therapy.
B. A 39-year-old woman with hypotension in the setting of acute inferior wall MI.
C. A 25-year-old man with recurrent septic pulmonary embolism.
View Answer
15. Answer: C. The hepatic venous flow shows holosystolic reversal compatible with severe TR, as in the setting of infective endocarditis of the tricuspid valve. A patient with controlled blood pressure has normal RA pressure and predominant forward systolic flow, not systolic reversal. In the setting of RV infarction and acute inferior wall MI, RV filling pressures are increased and there is predominant forward diastolic flow in the hepatic veins. Systolic flow is reduced, but not reversed in atrial fibrillation.
16. Which of the following is compatible with the hepatic venous flow in Figure 28-2?
A. A 49-year old man with dilated cardiomyopathy and systemic and pulmonary congestion.
B. A 29-year-old woman with pulmonary hypertension and systemic congestion.
C. A 55-year-old man with cardiac amyloidosis and lower extremity swelling.
View Answer
16. Answer: D. The hepatic venous flow shows a large Ar signal compatible with normal RA systolic function in the presence of increased RVEDP. In early stages of RV diastolic dysfunction, RVEDP is increased, whereas mean RAP is normal. This hemodynamic finding is compatible with option D. Systemic congestion occurs with increased RA mean pressure and predominant forward diastolic flow in all other choices.
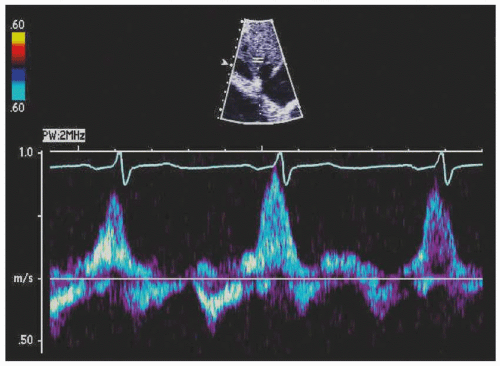
17. Continuous-wave Doppler at the pulmonic valve in a 42-year-old woman with right ventricular dilatation (Fig. 28-3). Which of the following findings by itself can establish the definitive diagnosis?
A. Color Doppler.
B. Right ventricular outflow tract stroke volume.
C. Right ventricular function.
D. None of the above.
View Answer
17. Answer: A. The patient has a wide regurgitant jet of pulmonic regurgitation (PR) by color Doppler and normal right ventricular systolic function with normal cardiac output. Spectral Doppler with a short deceleration time of PR may also occur due to an abnormally elevated right ventricular end-diastolic pressure. A wide color Doppler jet can differentiate severe pulmonic regurgitation from a nonsignificant regurgitant lesion. Normal RV systolic function with normal cardiac output in the presence of a short PR deceleration time supports the diagnosis of severe PR as opposed to a noncompliant RV. A noncompliant RV typically occurs in patients with an enlarged RV with reduced systolic function.
18. Tricuspid annular plane systolic excursion (TAPSE) was measured at 6 mm in a 47-year-old patient with cardiac amyloidosis (Fig. 28-4). Which of the following is true?
A. The lower normal limit for preserved right ventricular function is 16 mm.
B. TAPSE represents the longitudinal function of the right ventricle.
C. TAPSE is an accurate assessment of global RV function.
D. All of the above.
View Answer
18. Answer: E. TAPSE assumes that the tricuspid annulus displacement represents RV global systolic function. In reality, TAPSE reflects best longitudinal as opposed to global RV systolic function. The lower range for normal TAPSE is 16 mm.
A. Ebstein anomaly.
B. Carcinoid heart disease.
C. Rheumatic valvular disease.
D. None of the above.
View Answer
19. Answer: B. The 4-chamber view demonstrates the presence of prominent thickening and retraction of septal and anterior tricuspid leaflets with annular dilatation, characteristic findings of carcinoid heart disease. Ebstein anomaly is characterized by apical displacement of the septal leaflet and an elongated anterior leaflet in that view. Rheumatic tricuspid valve disease is usually accompanied by mitral valve rheumatic disease in patients with a history of rheumatic fever. The pathologic characteristic is commissural fusion of the leaflets with diffuse thickening and resultant stenosis and regurgitation.
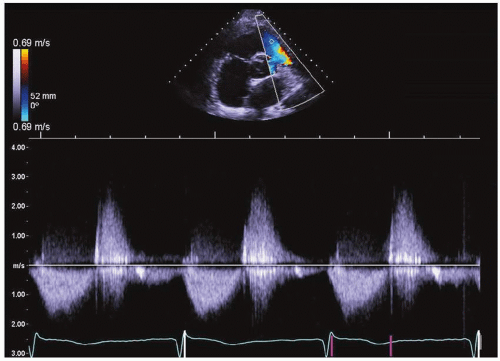
20. Which is true about this patient with pulmonary regurgitation (PR) (Fig. 28-5)?
A. Right ventricular end-diastolic pressure (RVEDP) is normal.
B. RV stiffness is increased.
C. Systolic reversal in the hepatic veins is present.
View Answer




20. Answer: B. The PR signal is steep indicating rapid equilibration of pressure between the PA and the RV. When RV stiffness is increased, RV diastolic pressure rises rapidly leading to a PR signal that is similar to that seen in this case. This patient has increased RVEDP and RAP. Tricuspid inflow is characterized by predominant early filling with an E/A ratio >1, and a steep deceleration time of tricuspid E velocity. Hepatic venous flow shows predominant forward flow in diastole (not systolic reversal).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree