INDICATIONS/CONTRAINDICATIONS
Indications
Sleeve lobectomies were initially conceptualized as a surgical option for those patients whose pulmonary function precluded them from undergoing pneumonectomy. However, as numerous investigators have demonstrated efficacy of sleeve lobectomy, the indications have expanded, recognizing the utility and potential benefit of lung parenchymal preservation even for patients who would clearly tolerate more extensive resections. Sleeve lobectomy should be considered for anatomically appropriate tumors, regardless of pulmonary function. With specific regard to sleeve resection of the right middle lobe (RML), it should be recognized that the benefit in this case is not to avoid pneumonectomy; rather, it is to avoid bilobectomy. In this sense, the utility of sleeve middle lobectomy (as compared to sleeve upper lobectomy) may be most applicable for those patients with truly limited cardiopulmonary reserve, as bilobectomy does not carry the same risk for morbidity or mortality as right pneumonectomy, and the avoidance of bilobectomy is most relevant to those who have the least capacity to tolerate significant resection. For patients with central middle lobe tumors and FEV1 <35% of predicted, sleeve resection should be strongly considered over bilobectomy.
Sleeve lobectomy of the RML is performed infrequently, as shown by a 2013 retrospective analysis of sleeve resection for lung cancer published by Yamamoto et al. In this study, spanning 20 years at a single institution, nearly 2,300 patients underwent operations for primary lung cancer, among whom 201 underwent sleeve resection, with isolated RML sleeve accounting for only three operations (0.1% of total resections, 1.5% of sleeve resections).
Masses anatomically appropriate for sleeve middle lobectomy include centrally located RML tumors, which involve the bronchus intermedius but not the lower lobe bronchus, lower lobe parenchyma, or intervening lymph node stations. Based on these anatomic criteria, the majority of such lesions tend to be low-grade neoplasms such as carcinoid or mucoepidermoid tumors. Sleeve lobectomy of the RML may also be feasible for nonsmall cell lung cancer (NSCLC). However, this tends to be a less frequent indication for sleeve lobectomy for two reasons: (1) centrally located NSCLC with central endobronchial extension tend to be more peripherally invasive and are less likely to be amenable to a parenchymal-sparing procedure; and (2) there is a tendency to take a more aggressive approach for NSCLC, as the importance of margins, completeness of resection, and lymphadenectomy are more significant with higher grade tumors. One particular situation for which RML sleeve resection may be performed for NSCLC occurs among patients who have RML cancer with central endobronchial involvement where concern exists regarding close bronchial margins despite an open approach with a hand-sewn bronchial closure.
In addition to malignancies, other indications exist for sleeve middle lobectomy. These include granulomatous disease, focal strictures, and chronic infection. Lady Windermere’s disease, coined by Reich and Johnson in 1992, refers to mycobacterium avium complex infection isolated to the middle lobe or lingula consequent to habitual voluntary cough suppression. Unlike other cases of mycobacterial infection, which tend to be more diffuse and occur in men with predisposing pulmonary disease or immunosuppressed individuals, these patients tend to be elderly women who chronically restrain themselves from coughing, resulting in poor mucociliary clearance and infection in the least drained areas of the lung (RML and lingula). Such infections may be challenging to treat medically, and patients with RML disease with chronic inflammation extending into the bronchus intermedius may occasionally be appropriate candidates for RML sleeve resection. Clearly, the use of sleeve resection for right middle lobectomy will be a “niche” procedure that will be infrequently used by the typical thoracic surgeon.
Contraindications
Patients with advanced lung cancer tend to be inappropriate candidates for sleeve lobectomy, and involvement of adjacent mediastinal structures are contraindications. General contraindications to pulmonary resection apply to sleeve lobectomy, and standard guidelines should be followed. In the situation of the RML, the structure closest to the confluence of the bronchus intermedius, the RML orifice and the right lower lobe orifice would be the pulmonary artery and the lobar branches to the middle and lower lobe (Fig. 35.1). Peripheral extension of the pathology to involve the pulmonary artery would typically lead to a recommendation for a bilobectomy to achieve a complete resection.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
If a sleeve resection is being considered for an indeterminate mass or known malignancy, diagnosis and staging should be completed as with any other pulmonary tumor. Such elements of the workup are discussed in detail elsewhere. Briefly, these should include:
 Tissue diagnosis, if obtainable preoperatively
Tissue diagnosis, if obtainable preoperatively
 Cross-sectional imaging of the chest
Cross-sectional imaging of the chest
 Lymph node staging, as appropriate for the lesion in question, possibly including:
Lymph node staging, as appropriate for the lesion in question, possibly including:
 Positron emission tomography
Positron emission tomography
 Endobronchial ultrasound with fine-needle aspiration
Endobronchial ultrasound with fine-needle aspiration
 Mediastinoscopy
Mediastinoscopy
 Evaluation for metastatic disease relevant to the specific disease process
Evaluation for metastatic disease relevant to the specific disease process
Suitability for operative intervention in general should be assessed, and pulmonary function tests with spirometry, in particular, are quite relevant for planning this operation. Usually, the RML will contribute 5% of the total pulmonary function. If the tumor has a central, endobronchial extension, the chances are that the RML does not contribute at all to the patient’s lung function. It is important, however, to determine if the patient could tolerate a bilobectomy should the attempts at sleeve resection fail. The usual techniques combining spirometry and perfusion scans to estimate predicted postoperative lung function will pertain.
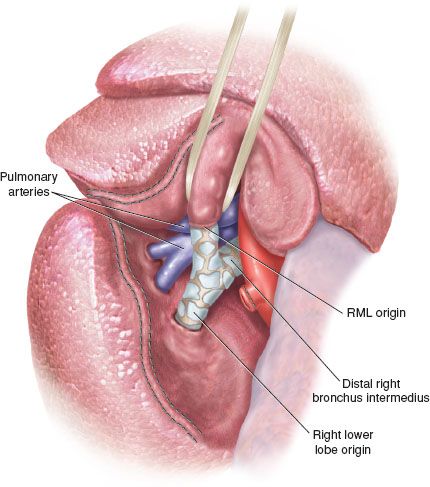
Figure 35.1 The anterior half of the major fissure has been divided with a stapler to show the origin of the RML bronchus and its confluence with the distal bronchus intermedius and the right lower lobe origin. Note the close proximity of the pulmonary artery to the central middle lobe bronchus, and thus the likelihood of pulmonary artery involvement with any transmural central right middle bronchus tumor.
Bronchoscopy is a key component of preoperative planning for RML sleeve resections, as with all bronchoplastic procedures. Bronchoscopic evaluation will allow for identification of endobronchial tumor at the middle lobe orifice or within the bronchus intermedius, while allowing the surgeon to verify that the lower lobe bronchus remains suitably clean to allow a postresection anastomosis. As is the case with all sleeve resections, it is important to determine preoperatively the extent to which the lower lobe has been obstructed by the mass. If the ongoing bronchus has been significantly obstructed, there may be impairment of secretion clearance from the lower lobe and there is potential for postobstructive bacterial pneumonia. In such situations, it may be prudent to debulk the endobronchial component in advance of the planned sleeve resection, so that the remaining lung parenchyma following pulmonary resection is best able to compensate following lobectomy. During such debulking procedures, the lower lobe should be suctioned and cleared of all secretions, with cultures obtained from any purulent secretions. After debulking and suctioning, prudent surgeons will treat with appropriate antibiotics and wait a few weeks prior to subsequent sleeve resection.
 SURGERY
SURGERY
Preparation
Anesthetic considerations include placement of a thoracic epidural catheter for intra- and postoperative analgesia. Patients should receive deep venous thrombosis prophylaxis with placement of lower extremity compression boots and subcutaneous heparin (safely administered 2 hours after placement of an epidural catheter). Antibiotics to prevent wound infection should be given prior to making incision.
Positioning and Airway Management
Patients are initially placed supine and intubated with a single-lumen endotracheal tube for the purpose of fiberoptic bronchoscopy. This is necessary at the time of the operation to verify extent of bronchial involvement and patient’s candidacy for sleeve resection. This will also help to define the limits of resection. Further, it allows for suctioning of the right lower lobe, which may contain retained secretions secondary to partial obstruction of the bronchus intermedius. After bronchoscopy, the endotracheal tube is changed to a standard left-sided double-lumen tube, as single lung ventilation is mandatory for the operative resection. The patient is turned into a standard left lateral decubitus position, with care taken to protect all bony prominences. Maintenance of appropriate endotracheal tube positioning is verified following the turn.
Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


