FIGURE 13-1 Early X-ray of bilateral cardiac catheterization using left ulnar arterial access and forearm central venous access from the right arm. (From Zimmerman HA, Scott RW, Becker NO. Catheterization of the left side of the heart in man. Circulation. 1950;1:357–359.)
Modern Era
During the 1990s, transradial arterial access techniques expanded as catheterization equipment improved with both a reduction in size and an improvement in performance. Lost in this enthusiasm for transradial cardiac catheterization was the stagnation in central venous techniques. Patients could undergo eloquent transradial procedures only to have their femoral vein also punctured so a right heart catheterization could be accomplished. The presumed inability to provide a central venous access to match the newer arterial technique was often used by doubters of the transradial approach to stick to their historic methods. Even among transradial converts, the need for right heart catheterization was used as an indication to revert to legacy techniques in the femoral artery and vein along with its concomitant risks and comorbidities.
Central access from forearm veins was redeveloped in the mid-1970s with the evolution of flexible polymer catheters that avoided many of the sequelae of long-term venous access.7 These peripherally inserted central catheters (PICC or PIC lines) became, and continue to be, popular in oncology, nutritional support, and other specialties, but the potential for use by the cardiology community was not generally recognized. As a medical resident in 1984, I passed an 8F-balloon-tipped, thermodilution catheter up the forearm of a young, highly anticoagulated patient with a prosthetic valve dehiscence in the middle of the night to help manage the hemodynamics prior to an emergency surgery planned for the following morning. The catheter passed without problems and entered the pulmonary artery and wedge position without X-ray support. My supervising cardiology fellow was less sanguine about this procedure and demanded the removal of the catheter before the attending’s arrival in the morning. According to her, it just did not seem right.
Extending the pilot experience as a resident almost 20 years before, Gilchrist et al.,8 in 2002, published a report reintroducing the utility of forearm venous access in the setting of radial artery access. This early work attempted to use veins that were very distal in the arm using special-order 125-cm-length 6F catheters provided by Arrow, Inc. (Teleflex USA, Reading, PA). Access was obtained at the time of catheterization by the physician with a tourniquet. This technique was limited by an inability to find veins at times on the distal forearm and occasional failure at blind cannulation of the deep veins that tend to course close to the radial artery. Otherwise, once venous access was obtained, the placement of vascular sheaths and 6F diagnostic balloon-tipped catheters was relatively unremarkable.
Subsequently, a slightly different approach was adapted with the access obtained anywhere along the forearm. In addition, initial intravenous puncture was done outside of the catheterization laboratory by the precatheterization technical staff who would establish a heparin-well venous access. This access site was then exchanged for a vascular sheath in the catheterization laboratory large enough to accept the right heart catheter or other indicated transvenous device. This markedly improved the efficiency of the procedure and demonstrated almost universal success.9
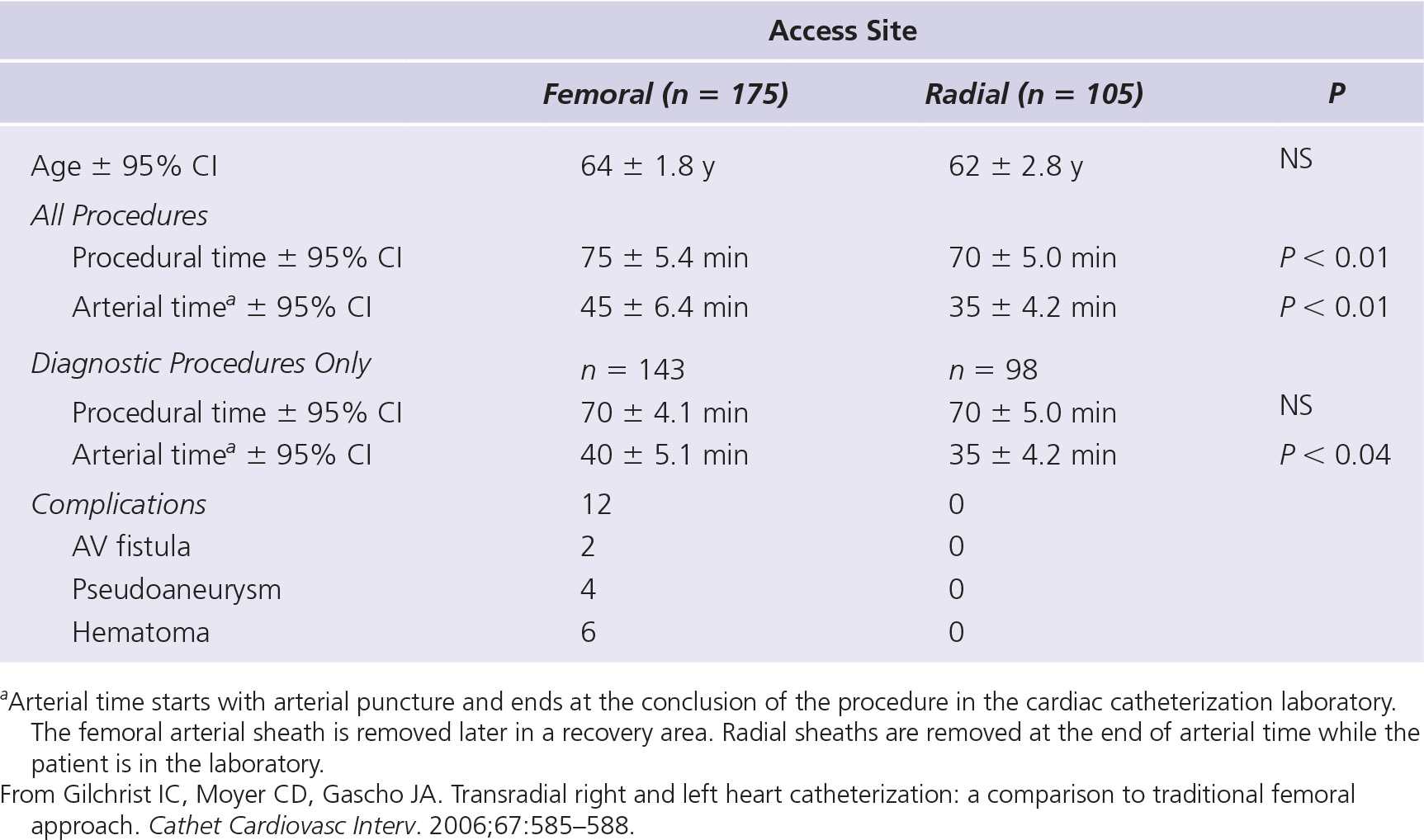
Table 13-2 lists the comparison of the procedural times and arterial times and X-ray exposure between bilateral heart catheterizations done via the forearm/transradial versus the traditional transfemoral route.9 While observational and single site, the data support that the shift to a forearm approach can be associated with procedural efficiency similar to that of the traditional techniques. A similar result was seen in a study done at a high-volume British center.10 While the outcomes were analogous to those listed in Table 13-2, the procedure times were slightly longer in the transradial groups (radial: 48 ±15 minutes, vs femoral: 32 ± 9 minutes, P < 0.05). This difference in results can probably be accounted for by differences in practices. Lo et al. obtained venous access in the catheterization laboratory versus the practice of using precatheterization venous access sites as done by Gilchrist et al. Since this publication, the institution is now utilizing prelaboratory venous access (J. Nolan, personal communication, September 2012). Several groups have now reported analogous reports of transvenous forearm access, confirming the successful application of this approach to central venous access.11,12
TABLE 13-2 Characteristics of Patients, Procedural Times, and Complications in Those Undergoing Either Femoral or Radial Right and Left Heart Catheterization
Practical Aspects of Venous Catheterization
Vein Physiology
Veins are distinctly different from arteries due to their different physiologic roles. The vessels of the arterial system are muscular and capable of controlling the high-pressure arterial system and redirect blood flow away from the heart to the end organs. The venous system is a low-pressure collecting system that delivers blood back to the heart. It serves a capacitance role. Veins are eight times more distensible than similar-sized arteries. Arterial vessels are composed of significantly more smooth muscle constitutions, resulting in far less compliance and distensibility than are seen in veins. In addition, the veins tend to respond to mechanical contact by catheter surfaces with far less tendency toward spasm than is commonly seen in the arterial system.
Vasoreactivity
While a growing body of literature concerning arterial vasoreactivity and prescriptions for cocktails to prevent arterial spasm exists, publications concerning the venous system are almost nonexistent. The venous system has less of a tendency for vasospasm, although there are older case reports from the era of large-sized, stiff catheters being passed up peripheral veins that confirm the potential for vigorous venospasm under some circumstances. From a pharmacologic viewpoint, veins are not responsive to calcium channel blockers13 but are readily responsive to nitrates. Since veins are often relatively superficial, nitrates can be applied topically in addition to being given in the usual intravenous, intra-arterial, or sublingual form to treat spasm. Application of warmth is another technique to release venous spasm. Raising the local extremity temperature to 42°C results in maximal vasodilatation.14
Venous Anatomy of Arm
Veins of the forearm and hand coalesce toward the antecubital fossa on the palmar side of the forearm into the basilic vein, which passes up the medial aspect of the upper arm or the cephalic vein of the lateral upper arm. In general, while individual variability is the rule with potential arrays of collaterals and alternative channels at all levels of the arm, forearm veins on the ulnar side drain up the basilic vein, while the veins from the radial side of the forearm show equal tendency toward cephalic or basilic drainage.15
The basilic vein offers the most direct passage to the central system as it forms the axillary vein at the junction with the cephalic vein, and then the subclavian vein as it passes into the chest cavity under the clavicle. The cephalic vein takes a more circuitous route up the lateral aspect of the upper arm, finally joining the axillary vein. This junction often forms a right angle and is described as a T-junction where the smaller cephalic enters the main venous channel. In older cardiology literature, this region was known for difficulties in permitting large, stiff catheters from completing successful passage. With modern soft and flexible catheters, this is not a barrier to catheter passage, but its presence must be considered as specific techniques and precautions may be needed to transit this region.
Localizing Veins
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


