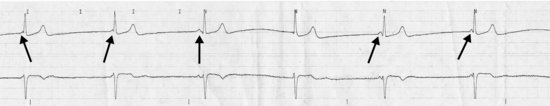
Junctional rhythm with AV dissociation
DESCRIPTION
A junctional, or “nodal” rhythm (more confusing, redundant terminology) arises in the atrioventricular (AV) junction (or node, as you guessed) instead of in the normal sinoatrial node, and thence travels to and excites the ventricle. The key is that in a junctional rhythm there are usually no P waves preceding the QRS complex. If you are really good, you might see upside-down (retrograde) P waves just before or just after the QRS (see arrow), which represent the atria being activated backwards (from bottom to top) from the AV node. Remember, the impulse which arises in the AV node usually will spread in both directions: down into the ventricle, and backwards up into the atrium. If you are able to point out these retrograde P waves, even if they’re not really there, it impresses everyone.
Sometimes a junctional rhythm seems to be competing with the sinus node. Here you may see sinus P waves slow down and wander in and out around the QRS complexes (see arrows) which are actually triggered by impulses arising in the AV node and have nothing to do with the P waves: the PR intervals are so short the P waves are clearly not responsible for the QRS complexes. The P waves and QRS complexes are dissociated: one is not related to the other. But this is not heart block because the P waves cannot be conducted to the ventricle, since the AV node just fired. Your friendly neighborhood electrophysiologist can explain this to you with a big blackboard and about 20 minutes.
HABITAT
This rhythm may be found in various habitats, and similar to poisonous snakes or rhinoceri, its significance is affected by the setting. In young ’uns or athletes, a junctional rhythm, especially at night, may be quite normal, representing increased parasympathetic tone. In an older person, however, we would worry about too much “slower-downer” medicine, such as digoxin, β-blockers, verapamil, or diltiazem, alone or in ridiculous combinations. We might also find junctional rhythms lurking in the jungles of an acute (especially inferior) myocardial infarction.
CALL
“I don’t see any P waves!”
RESEMBLANCE TO OTHER ARRHYTHMIAS
If it’s regular without preceding P waves, it is usually junctional, especially if the rate is under 60; junctional rhythms are usually slower than a sinus rhythm. If P waves are small and hard to see, you might be tempted to call a rhythm junctional; check all the leads carefully to avoid looking dumb. If the PR is particularly long (first degree AV block), P waves may be hidden in preceding T waves; again, look closely in all leads. If there is a regular rhythm with wide complexes and no P waves I would be tempted to call it a ventricular rhythm; take the strip (walk, don’t run) and show it to someone who knows.
CARE AND FEEDING
Restraint is the name of the game here; unless the junctional rhythm is particularly slow and is causing symptoms (blood pressure low, patient dizzy) we would usually leave it alone and look for causes. If you rushed in and shook awake a 24-year-old track star because you noticed a junctional rate of 35 on his monitor, you’d probably leave the room with a black eye and no autograph, because this is a normal rhythm for a young athlete. If an older patient had the same rhythm and an elevated digoxin level, we might administer anti-digitalis antibodies, because the rhythm was likely a digoxin toxic rhythm. Junctional rhythms in patients receiving agents that slow the sinus node (or block the AV node) usually just go away if you withhold the offending agent(s). In cases where a patient has a symptomatic junctional rhythm that can’t wait a day or two to go away and doesn’t respond to anti-digitalis antibodies (if the patient was receiving digoxin!) or other maneuvers to increase the heart rate, a pacemaker might be in order.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


