Retrotracheal Space Mass
Jud W. Gurney, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Vascular Anomalies
Aberrant Right Subclavian
Aberrant Left Subclavian
Double Aortic Arch
Substernal Goiter
Esophageal Disorders
Zenker Diverticulum
Achalasia
Foreign Body
Less Common
Tracheal or Esophageal Masses
Esophageal Carcinoma
Esophageal Leiomyoma
Tracheal Neoplasms
Nerve Sheath Tumors
Rare but Important
Mediastinal Cysts
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Retrotracheal space
Lateral examination: Triangular area of lucency bounded
Posteriorly by spine (1st 4 thoracic vertebra)
Inferiorly by top of aortic arch
Anteriorly by posterior wall of trachea
Superiorly by thoracic inlet
Trachea is straight; convex bowing anteriorly is considered abnormal
Also known as Raider triangle after radiologist Louis Raider who originally described radiographic significance
Lesions in retrotracheal space may not be evident on frontal radiographs
Lesions may widen or disrupt posterior junction line
Lesions of retrotracheal space arise from normal contents
Esophagus, trachea, lymph nodes, lung, nerves (left recurrent laryngeal nerve, vagus nerve), thoracic duct
Posterior tracheal band (or tracheoesophageal stripe)
Vertically oriented linear opacity < 4.5 mm in thickness (usually < 3 mm thickness)
Visible on lateral radiograph in 50%
Extends from thoracic inlet to carina
Components: Posterior tracheal wall, anterior esophageal wall, and mediastinal soft tissue
Tracheoesophageal stripe (TES) vs. posterior tracheal band (PTB); TES if
Stripe contains vertical fat radiolucency
Stripe passes below azygos arch
Helpful Clues for Common Diagnoses
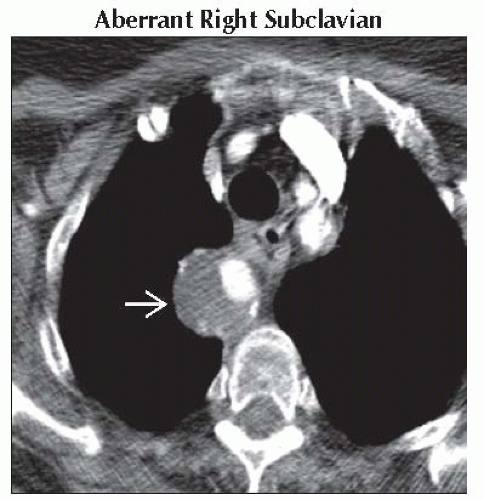
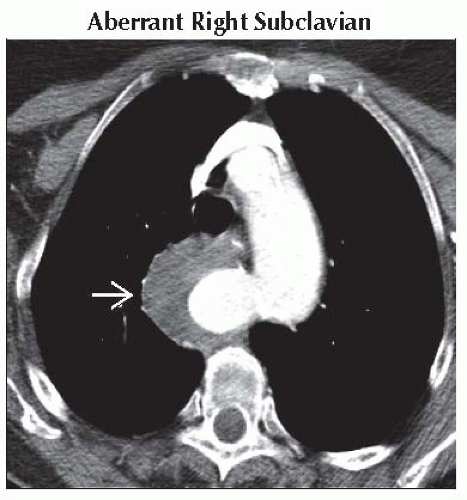
Aberrant Right Subclavian
Most common major aortic anomaly (0.5% of population)
Arises as last branch from left aortic arch
Origin often widened and known as diverticulum of Kommerell
Represents remnant of primitive distal right aortic arch
Seen in 60%
Aneurysmal when > 4 cm in diameter
Associated abnormalities
Congenital heart disease (CHD): Conotruncal anomalies, ventricular septal defects
Down syndrome with CHD; 37% have aberrant right subclavian
Surgical implications
Anomalous recurrent laryngeal nerve (nonrecurrent laryngeal nerve)
Thoracic duct may terminate on right
Most patients asymptomatic
Most common problem: Dysphagia (lusoria) from esophageal compression
Aberrant Left Subclavian
Arises as last branch from right aortic arch
Most common type of right aortic arch (0.05% of population)
Associated abnormalities
Tetralogy of Fallot (70%)
Atrial septal defect or ventricular septal defect (20%)
Coarctation of aorta (7%)
Double Aortic Arch
Most common vascular ring
Rarely associated with congenital heart disease
Results in tracheal &/or esophageal compression
Right arch is larger and positioned higher than left
Substernal Goiter
Represents up to 7% of mediastinal tumors
Usually has tracheal deviation on frontal radiograph
Posterior to trachea (25%), predominant on right side
Calcification in 25%
High attenuation at CT due to natural iodine
Zenker Diverticulum
Pulsion diverticulum at pharyngoesophageal junction
Descends into retrotracheal space posterior to trachea and esophagus
Size variable (0.5-8 cm)
May contain air or air-fluid level
May have findings of chronic aspiration
Achalasia
Primary motility disorder of smooth muscle or secondary (e.g., Chagas disease)
Esophageal dilatation, usually marked, with air-fluid level in upper esophagus
CT: Smooth narrowing of distal esophagus
Smooth symmetric wall thickening (< 10 mm); any asymmetric thickening or frank mass consider carcinoma (pseudoachalasia)
Foreign Body
Most common site of chronic esophageal foreign body is upper esophagus at level of thoracic inlet
Coins: Seen en face frontal and in profile on lateral views
CT useful for complications (perforation or abscess), may also be useful for nonradiopaque foreign body
Helpful Clues for Less Common Diagnoses
Esophageal Carcinoma and Leiomyoma
Most common tumors of esophagus
Widening of tracheoesophageal stripe and presence of air-fluid level most common findings
Tracheal Neoplasms
Rare, 2/3 either squamous cell carcinoma or adenoid cystic carcinoma
Adenoid cystic carcinoma more common in proximal 1/2 of trachea
May have either focal mass of tracheal wall or diffuse thickening of PTB
Nerve Sheath Tumors
Neurofibroma or schwannoma
May occur along any peripheral nerve
In retrotracheal space: Recurrent laryngeal nerve, vagus nerve, phrenic nerve
Helpful Clues for Rare Diagnoses
Mediastinal Cysts
Includes bronchogenic cysts, esophageal duplication cysts, thymic cysts, and thoracic duct cysts
None primarily located in region of retrotracheal space
Thoracic duct cyst
Rare, expands with fatty meals
Thin-walled, low-attenuation fluid characteristic
Image Gallery
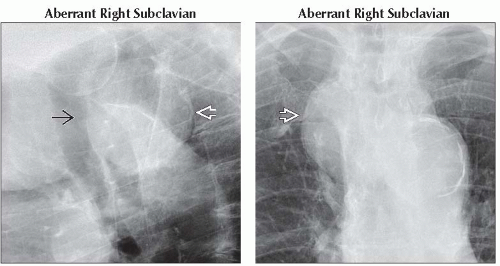 (Left) Lateral radiograph shows a large mass in Raider triangle
 . Note that the trachea is bowed anteriorly . Note that the trachea is bowed anteriorly  . The most common cause of mass in retrotracheal triangle is aberrant right subclavian artery. (Right) Frontal radiograph shows a right paratracheal mass . The most common cause of mass in retrotracheal triangle is aberrant right subclavian artery. (Right) Frontal radiograph shows a right paratracheal mass  . There is no posterior junction line. . There is no posterior junction line.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|