Fig. 33.1
Proposed treatment algorithm for patients presenting with SIVAD
In patients who are suitable candidates for medical management, the role of anticoagulation and antiplatelet therapy is unclear. The rationale for these therapies is the prevention of thrombosis and distal microemboli. While this strategy has traditionally been advocated in the medical management of SIVAD [3, 7], recent studies have failed to demonstrate significant benefit. In the largest case series of patients with SISMAD treated medically to date, Park et al. [8] analyzed 46 patients treated with medical management. Twelve patients received some combination of anticoagulation or antiplatelet therapy in their cohort, while 38 received neither. There was no difference observed in the clinical course of these two groups over a median follow-up period of 28 months, suggesting that anticoagulation and antiplatelet agents may not be necessary in the medical management of SIVAD. Furthermore, Takayama et al. [9] describe a cohort of 18 patients with dissections in the celiac, SM, common hepatic, and splenic arteries who were managed with medical management alone without anticoagulation or antiplatelet therapy, and all showed good outcomes over a mean follow-up time of 20.9 months. Moreover, a literature review of 291 cases of SISMAD performed by Luan et al. [2] evaluated 209 patients treated with medical management and failed to show any significant difference in outcomes between those treated with and without anticoagulation. In the absence of level I evidence, it can be said that patients have been successfully treated both with and without anticoagulation and antiplatelet therapy.
Results of conservative management in the treatment of SIVAD have been favorable. The majority of asymptomatic patients, as well as a significant number of symptomatic patients without evidence of vessel rupture or bowel necrosis, have been treated exclusively with medical management without the need for further intervention. A review of the literature in patients with SISMAD has shown that out of 291 reported cases, 209 (72 %) were treated with medical management alone [2]. Of these 209 patients, 156 (75 %) were managed successfully and 53 (25 %) required further treatment. In those patients that were managed unsuccessfully with medical treatment, 13 (6 %) died and were diagnosed at autopsy after no formal targeted visceral vessel management, 6 (3 %) required further hospitalization and medical management, 21 required endovascular intervention (10 %), 10 required open surgical intervention (5 %), 2 required bowel resection (1 %), and 1 patient received a hybrid repair with transmesenteric stenting of the SMA (Table 33.1). Compared to patients receiving endovascular or surgical intervention in SISMAD, patients receiving medical management have been shown to be younger on average and have less compression of their true lumen on initial imaging. Additionally, patients treated with medical management alone required shorter hospital stay [14]. Medical therapy is the most common approach to SICAD as well as having been used in 45–63 % of cases [3].
Table 33.1
Reported cases of medical, endovascular, and open surgical treatment of SIVAD
Vessel | # of cases | Medical | Endovascular | Open surgery | Secondary interventions | Complications |
|---|---|---|---|---|---|---|
Celiac | 72 | 47 | 6 | 19 | None | None |
SMA | 291 | 209 | 40 | 42 | Open surgery – 10 | 1 patient thrombosed open surgical repair on follow-up but remained asymptomatic |
Bowel resection – 2 | 1 patient thrombosed stent on follow-up but was asymptomatic | |||||
Endovascular – 22 | 1 patient had progressive aneurysmal dilatation after stenting and received a second stent | |||||
Hybrid – 1 | ||||||
IMA | 1 | 0 | 0 | 1 | 0 | None |
Follow-up data shows that SIVAD may often be a self-limiting event with very few long-term complications. Patients who present during the acute stage of their dissection with symptoms of abdominal pain, nausea, vomiting, and diarrhea are often symptomatic from the arterial dissection itself rather than from complications of the dissection (Fig. 33.2). With medical management, most patients see gradual resolution of their symptoms and follow-up imaging shows radiographic resolution with stable or improved dissection, partial or complete false lumen thrombosis, and an increase in true lumen diameter [3, 5–9].
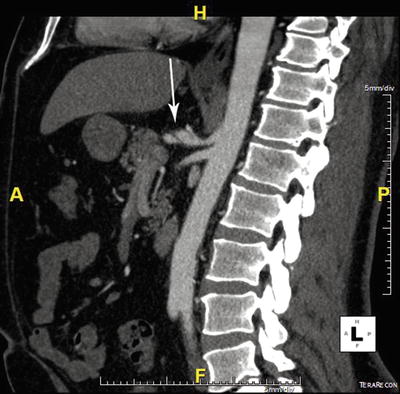
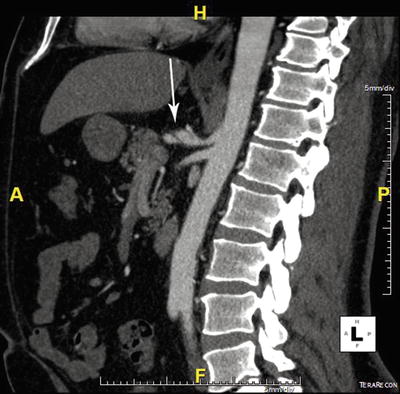
Fig. 33.2
Spontaneous dissection of the celiac artery treated successfully with conservative medical management
Results of Open Surgical Repair
Open surgical repair of SIVAD was first described in a report of isolated SMA dissection by Sisteron and Vieville in 1975 [10]. Since that time, open surgical repair has been described in 19 cases of SICAD and 43 cases of SISMAD. While these open surgical approaches were originally considered the mainstay of treatment for any SIVAD, more recently, endovascular approaches and conservative medical management have become more common. Currently, the suggested indications for open surgical repair in SIVAD include suspected end-organ necrosis requiring exploratory laparotomy, vessel rupture, and thrombosis or significant narrowing of the true lumen. Additionally, surgery can be considered in patients managed expectantly with persistent or recurring abdominal pain, progressive aneurysmal dilatation of the affected vessel segment, and false lumen expansion causing progressive narrowing of the true lumen.
Of the 19 cases of open surgery in SICAD reported, approaches have included bypass to the hepatic artery with prosthetic or autogenous vein graft in 14 patients, resection of the celiac artery with direct anastomosis of the hepatic artery to the celiac ostium in 3 patients, and ligation of the celiac artery without revascularization in 2 patients [3]. Eighteen of these procedures were performed during the initial phase of diagnosis, and only one after failure of conservative medical management, defined as worsening pain and propagation of the dissection [11]. No perioperative deaths have been reported in this patient population. Additionally, limited short-term follow-up ranging from 6 to 36 months shows these reconstructions to be durable, with all patients being asymptomatic on follow-up and evidence of stable repairs on imaging.
Out of 43 cases of open surgery in SISMAD, approaches have included aorto-mesenteric bypass in 9 patients, resection of SMA dissection with interposition graft in 6 patients, SMA to right gastroepiploic artery bypass in 3 patients, SMA to right common iliac artery bypass in 2 patients, transposition of the SMA to the aorta in 2 patients, SMA ligation in 1 patient, and a combination of intimectomy, thrombectomy, and endoaneurysmorrhaphy with or without patch angioplasty in 13 patients. The operative details for the remaining seven patients were not described [2]. Thirty-three cases were done at primary presentation, while the remaining ten cases were secondary interventions after failed conservative medical management. Two of the cases required bowel resection at the time of reconstruction due to bowel ischemia and necrosis. There have been no reported cases of patients needing surgical re-intervention after open surgery or endovascular treatment. Surgery has been generally performed on an emergent, acute, or subacute basis after the diagnosis of SISMAD, though in some cases patients required intervention up to 2 years after the first presentation of symptoms [12]. After successful surgical treatment, patients have all done well with relief of their symptoms and evidence of patent repairs at up to 5 years. Patients who have been treated with open surgical repair have been shown to be older and require a longer stay in hospital than those receiving endovascular interventions or medical treatment alone [13]. Only one case of failure after surgical intervention has been described. The patient in question received a saphenous vein graft bypass between the SMA and right common iliac artery as a primary intervention. During follow-up, the bypass thrombosed due to competitive flow in the native SMA but the patient continued to be asymptomatic at 5 years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


