INTRODUCTION AND CONCEPTUAL OVERVIEW OF OXYGEN TRANSPORT
Learning Objectives
The student will be able to describe the general process of oxygen transport and identify steps in this cascade that depend upon the lung to be achieved.
The student will be able to translate key words and phrases of pulmonary medicine into their internationally recognized abbreviations and acronyms.
The student will be able to calculate the partial pressures of constituent gases in normal dry air using Dalton’s law and explain the effects of altitude upon them.
The student will be able to use Boyle’s law and Charles’s law to convert gas volumes between standard conditions [Standard Temperature and Pressure, Dry (STPD)] and ambient conditions [Body Temperature and Pressure, Saturated (BTPS)].
The student will be able to compute the content of gases equilibrated with aqueous media using Henry’s law and their established solubility coefficients.
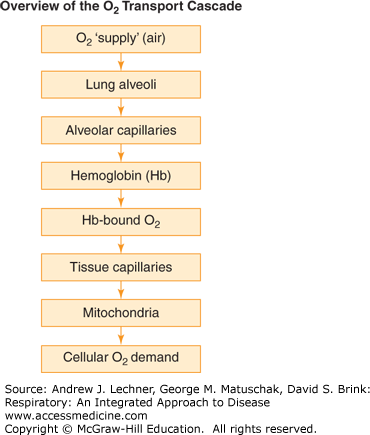
There is little argument that the urge to breathe is the most compelling drive that humans face, one they must satisfy every minute of life. Our dependence on aerobic metabolism to perform life’s complex functions requires coordinated interaction among multiple organ systems to deliver sufficient O2 for those demands (Fig. 1.1). Although only the upper elements of this O2 transport cascade are the formal purview of this book, physicians need to appreciate each aspect since failure at any step can become an O2 transport bottleneck with catastrophic consequences for their patients.
From this perspective, respiration really consists of two sequential processes within the lung, ventilation and diffusion. Each will require several chapters to describe their constituent parts and boundary conditions. As an obvious example, ventilation is the algebraic product of respiratory frequency, f, multiplied by the amount of air moved per breath, termed the tidal volume (VT). Less obvious is the fact that only a portion of each VT enters the alveolar volume (VA) where diffusion can occur, while the remaining portion of VT is confined to anatomical regions unsuitable for diffusion, collectively called the dead space volume (VD). Thus, one goal of this text is to provide the intellectual tools both to determine the fraction of VA in each VT, and to identify possible treatments for patients whose VA/VT is not optimal. As will be seen, the work of breathing and the calories required are substantial to inhale the 8,000-12,000 L of air per day just to support basal oxygen consumption. Clinicians must be able to distinguish if a patient’s work of breathing is excessive, and if so, whether due to altered recoil properties of the lungs and chest wall, or to reduced airway diameters which increase dynamic resistance. Such functional distinctions, and the structural changes that underlie them, form the central framework for sorting lung disorders into the so-called restrictive lung diseases and obstructive airway diseases. Later subsections of this book are devoted to providing a detailed introduction to both disease categories.
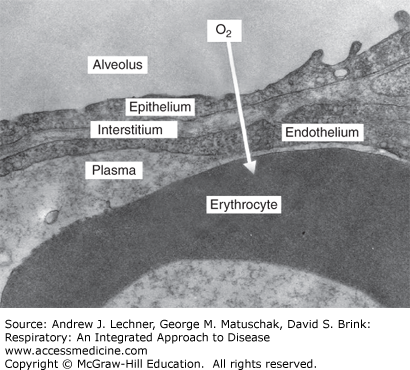
Even when the physical forces that regulate ventilation are ideal, the inhaled O2 must still diffuse through the delicate membrane sandwich that separates alveolar airspace from blood within the underlying pulmonary capillaries (Fig. 1.2). The resistance that the septal barrier poses to diffusion is related to its thickness and total surface area, which are modified in diseases like interstitial fibrosis and emphysema, respectively. Alveolar diffusion may be enhanced by interventions like increasing the fraction of inspired O2 in the ambient air, thereby increasing the pressure gradient for oxygen between the airspace and blood that is the driving force for diffusion. Much importance will be placed in the following chapters on training the clinician to determine when such supplemental O2 will probably improve tissue oxygenation versus when that tactic alone will fail.
RESPIRATORY SYSTEM NOMENCLATURE
Numerous terms and phrases pertaining to respiratory biology and pulmonary medicine will be introduced in this book. Among the most fundamental are abbreviations and acronyms that succinctly describe the origin and contents of a gas or fluid sample. With such shorthand, the phrase carbon dioxide partial pressure of alveolar gas usefully compresses to just PAco2, with its most common units of mm Hg implied. Likewise, the phrase fractional concentration of oxygen in the inspired gas mixture reduces to FIo2. The proper labeling of respiratory gases begins with the notation of F (fractional concentration, as a decimal from 0.0-1.0), or P (for pressure in mm Hg, torr, kilopascals, etc). The second letter (often subscripted) states the source or location of the gas, if known, including: A = alveolar; AW = airway; a = arterial; B = ambient barometric; c = capillary; ć = end-capillary; E = expired or expiratory; Ē = mean expiratory; É = end-expiratory (sometimes called end-tidal); I = inspired; IP = intrapleural; IT = intratracheal; v = venous; and v̄ = mixed or mean venous. Note that conventional usage may specify upper versus lower case lettering to distinguish locations. The final designation is to the gas species: O2, N2, CO2, H2O, etc. Thus, the phrases FĒco2 = 0.08 and Pćo2 = 105 mm Hg indicate respectively that the average fractional CO2 concentration in a sample of expired air is 8%, and that the partial pressure of O2 in blood exiting an alveolar capillary to enter a pulmonary venule is 105 mm Hg.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree