12 OBJECTIVES
Respiratory Abnormalities with Sleep Disorders
 Identify sleep stages and their physiology in the normal subject.
Identify sleep stages and their physiology in the normal subject.
 Describe the pathophysiology of obstructive and central sleep apneas.
Describe the pathophysiology of obstructive and central sleep apneas.
 Understand the diagnostic, clinical, and management principles relating to sleep-related breathing disorders.
Understand the diagnostic, clinical, and management principles relating to sleep-related breathing disorders.
GENERAL CONSIDERATIONS
It is well recognized that sleep disorders and respiratory functions are closely related. Sleep has a demonstrable effect on breathing patterns in individuals, producing a variety of specific clinical disorders such as obstructive sleep apnea (OSA) syndrome, or aggravating preexisting cardiopulmonary conditions such as chronic obstructive pulmonary disease (COPD) or congestive heart failure. This chapter will focus on this pathophysiologic relationship.
NORMAL SLEEP PHYSIOLOGY & DEFINITIONS
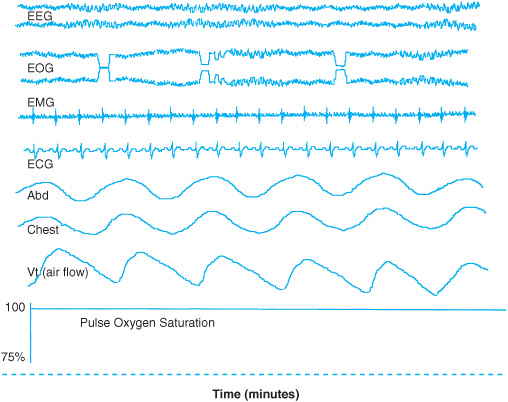
Sleep is divided into stages based on brain activity (as detected by the electroencephalograph [EEG]), eye movements (as detected by the electrooculogram [EOG]), and muscle activity (as detected by the electromyogram [EMG]). Additional parameters, including respiratory flow, oxygen saturation, and heart rate and rhythm, are simultaneously recorded during a polysomnogram (PSG) in order to diagnose sleep disorders (Figure 12–1).
Acknowledgment: The authors acknowledge the use of some clinical material and images from Omidvari K. Sleep disorders. In: Ali J, Summer WR, Levitzky MG, eds. Pulmonary Pathophysiology. New York: McGraw-Hill; 1999 and Barton C. Sleep disorders. In: Ali J, Summer WR, Levitzky MG, eds. Pulmonary Pathophysiology. New York: McGraw-Hill; 2005.
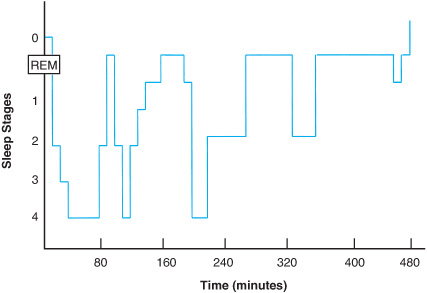
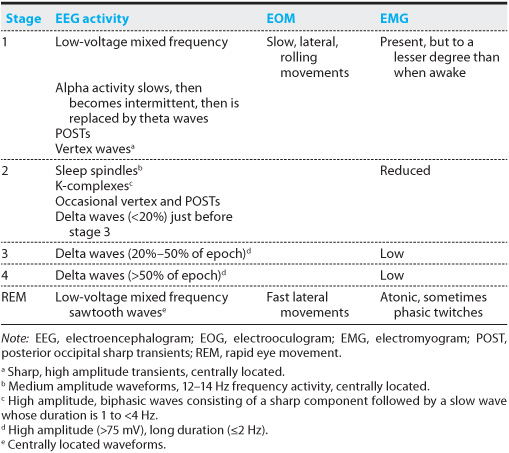
Sleep is categorized in various ways. Based on eye movements, sleep is characterized as being without rapideye movements (REM; non-REM sleep) or with rapid eye movements (REM sleep). Non-REM (NREM) and REM sleep alternate throughout the night in roughly 90-minute cycles. During the night, the relative amounts of NREM and REM sleep vary, with more REM sleep occurring toward the end of the sleep period (Figure 12–2). Stage 1 marks the transition from wakefulness to sleep and includes the state of drowsiness. During this stage, the EEG is characterized by mixed frequency low-voltage activity in addition to slow rolling eye movements. Stage 2 is defined by the presence of two distinct waveform complexes on EEG: sleep spindles and K-complexes. During this stage, breathing can be irregular due to fluctuations in respiratory drive. Stages 1 and 2 are categorized as light sleep. Stages 3 and 4 are called slow wave or delta sleep because they are defined by the amount of slow waves they contain, and are categorized as deep sleep. The EEG in REM sleep is composed of low-voltage mixed frequency activity with sawtooth waves. In normal subjects, almost all tonic muscle activity is suppressed, although phasic muscle twitches can occur. This is termed muscle atonia. Only extraocular and diaphragmatic muscle activity is preserved. Rapid eye movements are the hallmark of REM sleep. During this stage, intrinsic metabolic activity occurs that is not unlike that observed in the waking stage. Breathing is irregular. REM sleep generally occurs within 90–120 minutes of sleep onset and lasts 10–20 minutes. Episodes of REM sleep are of longer duration and occur more frequently toward the end of the sleep period (Table 12–1).
Figure 12–1. Normal polysomnogram
Figure 12–2. Depiction of “sleep architecture” in a typical 8-hour sleep period.
Table 12–1. Characteristics of sleep stages, normal sleep
CLASSIFICATION OF SLEEP DISORDERS
The International Classification of Sleep Disorders categorizes sleep disorders into four groups (Table 12–2). Dyssomnias include disorders of initiating and maintaining sleep that produce excessive sleepiness, the patient’s major complaint. Parasomnias include elements of undesirable phenomena or behavior such as rhythmic body movements or rocking that occur exclusively during sleep and are manifestations of nervous system activity. Excessive sleepiness is generally not the primary presenting complaint. Medicopsychiatric sleep disorders have features of disturbed sleep and wakefulness, although these are not generally the patient’s primary complaint. This category includes psychiatric, neurologic, and other medical conditions such as infections, nocturnal cardiac ischemia, sleep-related asthma, gastroesophageal reflux disease (GERD), peptic ulcer disease, and fibromyalgia. The fourth category contains proposed sleep disorders for which there is insufficient evidence available to clearly define them, but include pregnancy-associated disorders and terrifying hypnagogic hallucinations.
Dyssomnia is further subdivided into three major groups: intrinsic, extrinsic, and circadian sleep disorders based on pathophysiologic mechanisms. Intrinsic sleep disorders arise from causes in the brain or body and include sleep-related breathing disorders (SRBDs), restless leg syndrome, and narcolepsy. Extrinsic sleep disorders are predominantly caused by disturbances of the environment. Some of these disorders depend on internal factors that initially cause a sleep disturbance, but continued sleep disturbance ultimately depends on external factors. When the external factors are removed, the sleep disorder disappears. This group includes stimulant-dependent sleep disorder and altitude insomnia. Circadian sleep disorders, although due to internal central nervous system (CNS) factors, are grouped separately because of their common chronobiologic basis. The patient’s sleep pattern, which is internally generated, is out of synchrony with external societal demands, so the patient sleeps and wakes at times that are inappropriate and complains of insomnia or excessive sleepiness. Jet lag syndrome and shift-work sleep disorder are examples of these derangements.
Table 12–2. The American Sleep Disorders Association International Classification of Sleep Disorders
Dyssomnias (disorders of initiating and maintaining sleep) |
Intrinsic sleep disorders |
Extrinsic sleep disorders |
Circadian sleep disorders |
Parasomnias |
Disorders of arousal |
Sleep–wake transition disorders |
Parasomnias associated with REM sleep |
Other parasomnias |
Medicopsychiatric sleep disorders |
Associated with affective disorders |
Associated with neurologic disorders |
Associated with other medical disorders |
Proposed sleep disorders |
Not clearly defined |
Note: REM, rapid eye movement.
RESPIRATORY PHYSIOLOGY DURING NORMAL SLEEP
In normal adults, tidal volume decreases by 15%–25% during sleep, with shallowest breathing occurring during REM sleep. Respiratory frequency can increase slightly during NREM sleep, but is irregular during REM and stages 1 and 2 of NREM sleep. Minute ventilation decreases by 0.5–1.5 L/min as a consequence of decreased tidal volume. Arterial carbon dioxide pressure (Paco2) increases by 2–3 mm Hg while arterial oxygen pressure (Pao2) decreases by 3–10 mm Hg such that the net result is a 0%–2% decrease in arterial oxygen saturation (Sao2). Breathing during REM sleep becomes irregular due to changes in cortical activity associated with dreaming. Cyclical fluctuations in tidal volume, referred to as periodic breathing, are commonly observed during the transition from wakefulness to NREM sleep. This oscillatory breathing pattern results from fluctuations in respiratory center output in the brain. Alveolar ventilation is adjusted between the higher set point associated with wakefulness and the lower set point associated with sleep. At sea level, the fluctuations in alveolar O2 tension are insufficient to produce noticeable changes in Sao2. However, sleep at high altitudes potentiates periodic breathing and results in alterations in Sao2. As sleep proceeds through slow wave sleep, ventilation becomes monotonously regular. Pauses in respiratory flow are frequently observed in normal patients. In normal subjects, they are generally short (<20 seconds in duration) and infrequent (<5 per hour of sleep). They can cause small decreases in Sao2 and occur most commonly in REM and stage 1 and 2 sleep (NREM).
Age, male gender, use of alcohol or sedatives, obesity, and a history of hypertension, snoring, and upper airway muscle dysfunction are some of the risk factors for the occurrence of pathologic respiratory flow pauses called apneas and hypopneas, which are defined below.
Apneas and hypopneas can cause hypoxemia and hypercapnia. The amount of Sao2 decrease is determined by the length of the pause, initial lung volume, ventilation-perfusion match, venous O2 saturation, cardiac output, and factors affecting the oxyhemoglobin dissociation curve. Ventilatory responses to hypercapnia and hypoxia are blunted during sleep, most prominently in REM sleep. The decreased ventilatory response is due to increased airway resistance and decreased central ventilatory drive, among other factors. However, arousal from sleep occurs when the Paco2 increases by 6–15 mm Hg. The arousal response to hypoxia is weaker than that to hypercapnia. Both of these may result in sleep stage transition and lighten sleep. However, most arousals are linked to airway obstruction and a secondary increase in the work of breathing.
HEMODYNAMIC CHANGES THAT OCCUR DURING NORMAL SLEEP
Changes in metabolic rate as well as parasympathetic and sympathetic tone in the nervous system cause a general decrease in systemic blood pressure and heart rate.
Systemic blood pressure reaches a nadir within several hours after sleep onset, followed by a gradual tendency to increase throughout the remainder of sleep. Mean arterial blood pressures decrease an average of 5%–9% during stages 1 and 2 and an average of 4%–8% during stages 3 and 4. During REM, blood pressure fluctuates widely, but is usually increased above NREM values. In contrast to significant changes in systemic blood pressure that can occur in sleep, pulmonary artery pressures remain in the physiologic range in normal individuals.
Heart rate decreases by 5%–8% during NREM sleep and increases to waking levels during REM sleep. Benign sinus arrhythmias with pauses up to 2 seconds in duration can be observed with type I second-degree atrioventricular block, which occurs in up to 6% of young adultmales, but less often in young women and the elderly. In sleep, although there is a general reduction in ventricular ectopy, it can still be detected in 48%–73% of normal subjects, with the highest incidence of ectopy occurring during REM sleep. Ectopic rhythms can be complex (multifocal, repetitive, or both) in 15% of cases. Ventricular tachycardia is rare.
Sudden nocturnal death can occur in apparently healthy individuals, with the highest death rates occurring between 4 and 6 am, when REM sleep is most abundant. Prolonged sinus arrest and ventricular arrhythmias during REM sleep have both been proposed as possible mechanisms for sudden death. In those patients with known cardiac disease, cardiac monitoring demonstrates that the transition from ventricular tachycardia to ventricular fibrillation is the most common cause of sudden death. Lower heart rate as well as reduced stroke volume contributes to a decrease in cardiac output of about 10% during NREM sleep. Decreases in cardiac output parallel reductions of systemic blood pressure, resulting in little change in total peripheral resistance. Cardiac output is variable during REM sleep but can fall by as much as 26%.
PATHOPHYSIOLOGY OF SRBDs
SRBDs represent a spectrum of disorders that include OSA syndromes, central sleep apnea (CSA) syndromes, and hypoventilation syndromes. OSA is characterized by repetitive episodes of obstructive apneas and hypopneas that cause arousals and desaturations and result in a complaint of excessive daytime sleepiness. CSA is characterized by repetitive central apneas and hypopneas that also cause arousals and desaturations and result in complaints of insomnia, the inability to remain asleep with or without excessive daytime sleepiness.
Definition of Apnea
An apnea that occurs during sleep is defined by a significant decrease or complete absence of airflow for 10 seconds or longer. A hypopnea is defined as an incomplete absence of airflow resulting in an arousal from sleep or a decline in oxygen levels by 3% or 4% desaturation. Depending on the cause, apneas and hypopneas during sleep are divided into three types: central, obstructive, or mixed. Central apnea is defined as an apneic event characterized by cessation in oronasal air flow which coincides with the lack of effort detected in muscles of inspiration. It is due to the absence of CNS respiratory drive and is detected by chest wall monitors that remain silent during inspiration. Obstructive apnea occurs when respiratory flow is absent or significantly reduced despite the fact that activity in muscles of inspiration is detected by chest wall monitors. This signifies that although respiratory drive is normal, obstruction in the upper airway prevents respiratory inflow. Mixed apnea
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree