The aim of the present study was to investigate whether reperfusion by primary percutaneous coronary intervention (PCI) improves 12-month survival in late presenters with ST-segment elevation myocardial infarction (STEMI). We analyzed 2,036 patients with STEMI presenting 12 to 24 hours from onset of symptoms, without cardiogenic shock or pulmonary edema and not reperfused by thrombolysis, of 23,517 patients with STEMI enrolled in the Polish Registry of Acute Coronary Syndromes from June 2005 to August 2006. An invasive approach was chosen in 910 (44.7%) of late presenters and 92% of them underwent reperfusion by PCI. Patients with an invasive approach had lower mortality after 12 months than patients with a conservative approach (9.3% vs 17.9%, p <0.0001). The benefit of an invasive approach was also observed after multivariate adjustment with a relative risk 0.73 for 12-month mortality (95% confidence interval 0.56 to 0.96) and in a subpopulation of patients selected by a propensity-score matching procedure with an adjusted relative risk 0.73 for 12-month mortality (0.58 to 0.99). In conclusion, almost 1/2 of late presenters with STEMI were considered eligible for reperfusion by primary PCI. These patients had a lower 12-month mortality rate than they would have had if they had been treated conservatively, which supports the idea of late reperfusion in STEMI. However, whether all late presenters with STEMI should be treated invasively remains unanswered. Nevertheless, until a randomized trial is undertaken, late presenters with STEMI could be considered for reperfusion by primary PCI.
Optimal management for patients with ST-segment elevation myocardial infarction (STEMI) who arrive at a hospital late remains uncertain. A few recently published studies have suggested that reperfusion by percutaneous coronary intervention (PCI) could be beneficial to patients if performed just after 12 hours from onset of symptoms. In addition, the most recent European guidelines on STEMI recommend PCI for late presenters with ongoing ischemia. The aim of our analysis was to assess the current use of invasive treatment and mechanical reperfusion by primary PCI applied 12 to 24 hours from onset of symptoms in patients with STEMI arriving at a hospital 12 to 24 hours from onset of symptoms and to determine the influence of this invasive approach on 12-month mortality in clinical practice.
Methods
We used data from the Polish Registry of Acute Coronary Syndromes (PL-ACS), for which the method and results of the first 100,193 patients have been described. In brief, the PL-ACS is an ongoing, nationwide, multicenter, prospective, observational study of consecutively hospitalized patients with the entire spectrum of ACSs in Poland. The pilot phase of the registry commenced in October 2003 in the Silesia region. In subsequent months, further regions were opened and, since June 2005, all Polish regions collect data for the PL-ACS.
Hospitals were invited to enter the registry if they had a coronary care unit, a cardiology unit, a cardiac surgical unit, an internal medicine unit, or an intensive care unit or if they hospitalized ≥10 patients with ACS per year.
A detailed protocol with inclusion and exclusion criteria, methods and logistics, and definitions of all fields in the registry dataset was prepared before the registry was started. However, it has since been revised 2 times. In May 2004, the protocol was adapted to be compatible with the Cardiology Audit and Registration Data Standards (CARDS). Nevertheless, the PL-ACS case-report form (CRF) covers only part of the CARDS dataset. A second revision (May 2005) added new fields to the CRF, which included exact dates and times of onset of symptoms, coronary angiography, and PCI procedures.
According to the protocol, all admitted patients with suspected ACS were screened for eligibility to enter the registry but were not enrolled until the ACS was confirmed. Patients were then classified as having unstable angina, non-STEMI, or STEMI. STEMI was defined as the presence of (1) ST-segment elevation consistent with infarction of ≥2 mm in contiguous chest leads and/or ST-segment elevation of ≥1 mm in ≥2 standard leads or new left bundle branch block and (2) positive cardiac necrosis markers. If a patient was hospitalized during the same ACS in >1 hospital (transferred patient), all hospitals were required to complete the registry data. These hospitalizations were linked together during data management and were analyzed as 1 ACS.
Data were collected by skilled physicians who were in charge of each patient and entered directly into an electronic CRF or temporarily printed onto a CRF before being transferred to an electronic CRF. Internal checks for missing or conflicting data and values markedly out of the expected range were implemented by the software. In the Silesian Center for Heart Diseases (Zabrze, Poland) data management and analysis center, further edit checks were applied if necessary.
All-cause mortality data with exact dates of deaths were obtained from official mortality records from the National Health Fund. Vital status at 12 months after STEMI was available for all patients enrolled up to August 2006.
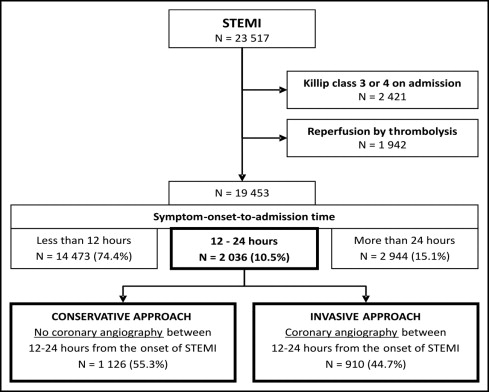
For the present analysis, we selected patients with STEMI who were enrolled during a consecutive 15-month period, from the time of the second protocol revision (June 2005) to August 2006. In addition, we excluded patients with severe hemodynamic disturbances on admission such as pulmonary edema (Killip class III) and cardiogenic shock (Killip class IV) for whom the recommended window for invasive treatment exceeded 12 hours. Furthermore, patients initially treated with thrombolysis were excluded.
Symptom-onset-to-admission time was calculated for every patient as an absolute difference in minutes between dates and times of hospital admission and onset of symptoms. Only patients with symptom-onset-to-admission times 12 to 24 hours comprised the study population. Two groups of patients were then identified based on whether coronary angiography had been performed and time of the invasive procedure.
Patients were included in the invasive-approach group if they had coronary angiography performed 12 to 24 hours from onset of symptoms. All other patients (treated noninvasively or with coronary angiography performed >24 hours from symptom onset) were included in the conservative-approach group.
The main outcome measurement was 12-month all-cause mortality. In-hospital outcomes were death from any reason, recurrent MI (defined as an ischemic event that met European Society of Cardiology/American College of Cardiology criteria for reinfarction and was evidently clinically distinct from the index event at time of admission), and stroke (defined as an acute neurologic deficit that lasted >24 hours and affected the ability to perform daily activities or resulted in death).
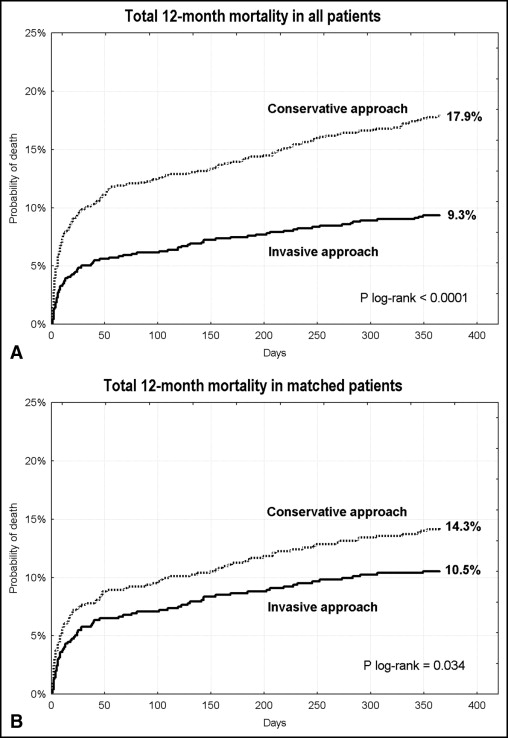
Continuous variables are reported as mean ± SD or median and interquartile range as appropriate. Categorical variables are expressed as percentages. Student’s t test and, when the assumption of normality was violated, Mann-Whitney U test were used for comparison of continuous variables. Normality of distribution was checked with the Shapiro-Wilk test. To compare categorized variables, chi-square test was used. Follow-up mortality was analyzed using the Kaplan-Meier method, and differences between groups were compared with log-rank test. Multivariate Cox proportional hazard model regression was performed to adjust the influence of the invasive approach on 12-month mortality, including all parameters listed in Table 1 , except for place of hospitalization. Hazard ratios and 95% confidence intervals were calculated.
| Variable | Conservative Approach | Invasive Approach | p Value |
|---|---|---|---|
| (n = 1,126) | (n = 910) | ||
| Age (years), mean ± SD | 67.2 ± 13.2 | 63.3 ± 11.8 | <0.0001 |
| Women | 44.0% | 32.4% | <0.0001 |
| Smokers | 29.1% | 42.5% | <0.0001 |
| Hypertension | 63.1% | 63.3% | 0.94 |
| Diabetes mellitus | 23.9% | 23.4% | 0.80 |
| Obesity (body mass index ≥30 kg/m 2 ) | 17.9% | 18.2% | 0.82 |
| Previous myocardial infarction | 16.6% | 11.2% | 0.0005 |
| Previous coronary bypass | 5.3% | 2.9% | 0.0058 |
| Previous percutaneous coronary interventions | 1.2% | 1.0% | 0.59 |
| Cardiac arrest before admission | 1.0% | 1.7% | 0.18 |
| Anterior wall infarct location | 41.3% | 45.2% | 0.080 |
| Heart rate on admission (beats/min), mean ± SD | 81 ± 21 | 78 ± 17 | 0.0001 |
| Other than sinus rhythm | 10.0% | 4.8% | <0.0001 |
| Systolic blood pressure (mm Hg), mean ± SD | 139 ± 28 | 136 ± 27 | 0.032 |
| Killip class II on admission | 24.0% | 11.8% | <0.0001 |
| Symptom-onset-to-admission time (hours), median (interquartile range) | 16 (14–21) | 15 (12–18) | <0.0001 |
| Hospitalization in hospital with percutaneous coronary intervention capability | 26.1% | 100% | <0.0001 |
Due to differences in baseline characteristics between groups, a propensity-score method was used to identify comparable patients treated with invasive and conservative approaches. Multivariate logistic regression analysis, including all baseline characteristic parameters listed in Table 1 except for place of hospitalization, was performed to calculate the predicted probability of receiving an invasive approach (propensity score) for every patient. Patients from the conservative group were then matched to patients from the invasive group. Because of substantial differences in baseline parameters, only 68% of patients remained after the matching procedure. The original multivariate Cox proportional hazard model regression was recalculated in the matched groups to further adjust the influence of an invasive approach on 12-month mortality. Subgroup analysis to identify patients who would potentially benefit from an invasive approach was performed with univariate Cox proportional hazard model regression in the matched population.
A 2-sided p value ≤0.05 was considered statistically significant. For all calculations, STATISTICA 7.1 (StatSoft, Inc., Tulsa, Oklahoma) was used.
Results
In total 23,517 patients with STEMI were hospitalized in 385 hospitals from June 2005 to August 2006. After excluding patients with pulmonary edema and cardiogenic shock on admission and, subsequently, those whose reperfusion was primarily by thrombolysis, there were 19,453 patients, and symptom-onset-to-admission time was calculated. A prehospital delay from 12 to 24 hours was observed in 2,036 patients (10.5%). Criteria for an invasive approach were fulfilled by 44.7% of them. The remaining patients were assigned to the conservative-approach group ( Figure 1 ).
Differences in clinical characteristics between groups presented in Table 1 show that an invasive approach was chosen more frequently in patients with a more favorable baseline risk profile. These patients were on average 4 years younger, more often men, less frequently had a history of MI and previous bypass surgery, and were less often in Killip class II on admission. About 1/4 of patients from the conservative group were treated in hospitals with PCI capability.
Most from the invasive group had coronary angiography done within 90 minutes of time of admission ( Table 2 ). Coronary angiography was also performed in 15% of patients assigned to the conservative approach. In almost all these patients, door-to-angiography time exceeded 2 hours, and symptom-onset-to-angiography time was >24 hours. Consequently, PCI was performed in 12% of patients in conservative group, whereas 92% of patients in the invasive group received primary PCI. Significant differences were also observed in pharmacotherapy during hospitalization with the invasive group having greater use of thienopyridines, glycoprotein IIb/IIIa inhibitors, β blockers, statins, and angiotensin-converting enzyme-inhibitors and less frequent use of nitrates and diuretics.
| Variable | Conservative Approach | Invasive Approach | p Value |
|---|---|---|---|
| (n = 1,126) | (n = 910) | ||
| Coronary angiography | 15.0% | 100% | <0.0001 |
| Door-to-angiography time (minutes) | |||
| ≤90 | 0.6% | 86.2% | |
| 91–120 | 1.2% | 4.6% | <0.0001 |
| >120 | 98.2% | 9.2% | |
| Primary percutaneous coronary intervention | 12.1% | 91.8% | <0.0001 |
| Initial Thrombolysis In Myocardial Infarction grade 2 or 3 flow | 22.6% | 21.8% | 0.85 |
| Final Thrombolysis In Myocardial Infarction grade 2 flow | 6.7% | 7.2% | 0.84 |
| Final Thrombolysis In Myocardial Infarction grade 3 flow | 90.3% | 87.3% | 0.33 |
| Stent implantation | 93.4% | 90.2% | 0.23 |
| Coronary bypass | 0.3% | 1.2% | 0.011 |
| Aspirin | 95.7% | 97.0% | 0.10 |
| Thienopyridines | 42.0% | 87.8% | <0.0001 |
| Glycoprotein IIb/IIIa receptor inhibitor | 3.6% | 22.0% | <0.0001 |
| Heparin | 76.9% | 69.8% | 0.0003 |
| β Blocker | 74.7% | 79.0% | 0.022 |
| Calcium antagonist | 5.0% | 3.7% | 0.18 |
| Statin | 74.9% | 86.6% | <0.0001 |
| Angiotensin-converting enzyme inhibitor | 71.1% | 80.8% | <0.0001 |
| Nitrate | 53.0% | 27.6% | <0.0001 |
| Diuretic | 31.4% | 19.2% | <0.0001 |
In-hospital and 12-month outcomes are presented in Table 3 . Patients in whom an invasive approach was chosen had approximately 1/2 the mortality of the conservative group after 30 days and 12 months. A similar trend was observed for in-hospital reinfarctions. After multivariate adjustment ( Figure 2 ), an invasive approach remained significantly associated with lower relative risk of 12-month mortality (hazard ratio 0.73, 95% confidence interval 0.56 to 0.96).
| Variable | Conservative Approach | Invasive Approach | p Value |
|---|---|---|---|
| (n = 1,126) | (n = 910) | ||
| Stroke in hospital | 0.6% | 0.7% | 0.92 |
| Recurrent myocardial infarction in hospital | 5.2% | 2.6% | 0.0041 |
| Death in hospital | 6.8% | 2.6% | <0.0001 |
| Combined in-hospital outcome | 12.2% | 5.7% | <0.0001 |
| 30-day mortality | 10.0% | 5.1% | <0.0001 |
| 6-month mortality | 14.2% | 7.5% | <0.0001 |
| 12-month mortality | 17.9% | 9.3% | <0.0001 |
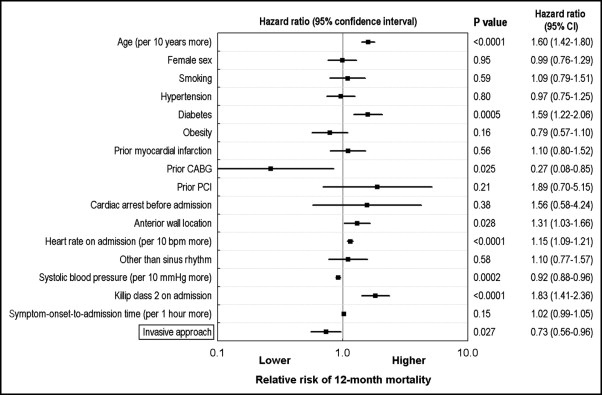
The lower 12-month mortality of an invasive approach was also observed in the subpopulation of patients selected by the propensity-score matching procedure ( Figure 3 , Table 4 ). Of note, however, the guidelines’ recommended pharmacologic treatment was more widely used in patients who received an invasive approach. In addition, we did not find any specific subgroup of patients for whom an invasive approach could be potentially harmful ( Figure 4 ).