Renopulmonary Syndromes
Jud W. Gurney, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
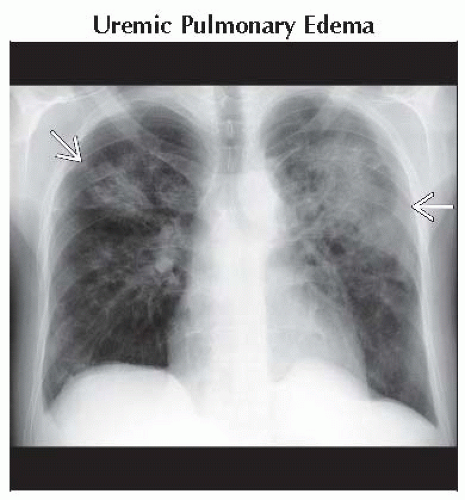
Uremic Pulmonary Edema
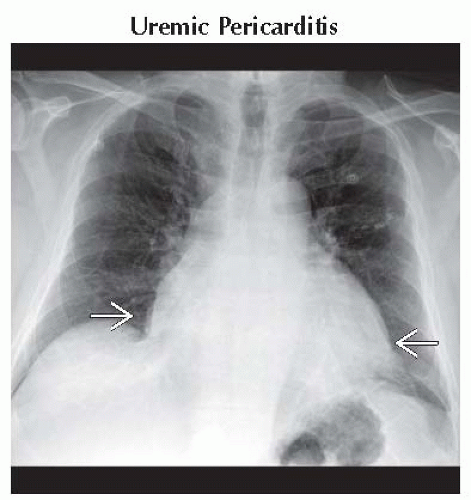
Uremic Pericarditis
Diffuse Alveolar Hemorrhage (DAH)
Wegener Granulomatosis
Goodpasture Syndrome
Systemic Lupus Erythematosus
Microscopic Polyangiitis
Renal Cell Carcinoma
Less Common
Lymphangiomyomatosis
Metastatic Pulmonary Calcification
Sarcoidosis
Rare but Important
Sickle Cell Disease
Birt-Hogg-Dubé Syndrome
Erdheim Chester Disease
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Recognition of renal osteodystrophy in chronic renal failure (CRF)
Bone resorption
Erosion of distal clavicles
Osteopenia (50%)
Compression fractures (5-25%)
Rib fractures (5-25%)
Osteosclerosis of axial skeleton (10-30%)
Vertebral bodies: Band-like areas of sclerosis of superior and inferior endplates (“rugger jersey” spine)
Brown tumors (1%): Lytic expansile lesions, cortical, usually solitary
Soft tissue calcification
Periarticular and symmetric
Pleural effusions common in CRF
From overhydration, left ventricular (LV) failure, nephrotic syndrome, autoimmune disease, peritoneal dialysis
Cardiomegaly common in CRF
From overhydration, LV failure, high output failure, pericardial disease, underlying disease causing renal failure
Helpful Clues for Common Diagnoses
Uremic Pulmonary Edema
Batwing central pulmonary opacities classic but not specific
From LV failure, overhydration, anemia, hypoproteinemia, high output AV fistula, diffuse alveolar damage (uremic lung)
Uremic Pericarditis
Includes acute pericarditis, pericardial effusions, cardiac tamponade, constrictive pericarditis
Injury from toxic metabolites from renal failure, underlying disease, drug toxicity
Cardiomegaly in 95%
Diffuse Alveolar Hemorrhage (DAH)
From small-vessel vasculitis affecting lung and kidney
Acute onset batwing consolidation in anemic patient
Hemoptysis (66%), may be mild
Radiology-pathology correlation
Hemorrhage into alveolar spaces (ground-glass opacities to consolidation)
Blood removed from alveoli by macrophages (2-3 days)
Macrophages migrate into interstitium (septal thickening)
Macrophages removed by lymphatics (7-14 days) (lungs return to normal)
Wegener Granulomatosis
Hemorrhagic presentation in 8%
May occur in absence of cavitary nodules
Goodpasture Syndrome
May follow influenza-type illness
Males (M:F = 9:1), often smokers
Systemic Lupus Erythematosus
Autoimmune disorder characterized by antinuclear antibodies, females (M:F = 1:10)
Hemorrhage in 2%, may be fatal
Renal involvement in 60-90%
Unexplained small bilateral pleural effusions and cardiomegaly
Microscopic Polyangiitis
Variant of polyarteritis nodosa
Pulmonary hemorrhage (10-30%)
Glomerulonephritis (80-100%)
Renal Cell Carcinoma
Propensity for metastasizing to uncommon locations (e.g., mediastinal nodes, endobronchial, intravascular) in addition to typical locations (lung, pleura, bone)
Helpful Clues for Less Common Diagnoses
Lymphangiomyomatosis
Nonneoplastic hamartomatous proliferation of atypical muscle cells
Women of child-bearing age
Radiographic manifestations
Thin-walled cysts: Diffuse, bilateral, and uniform in size; cysts increase in number and size as disease progresses, results in hyperinflation
Spontaneous pneumothorax (40%)
Small chylous pleural effusions
Renal angiomyolipomas (20-50%): Small (< 1 cm), multiple, bilateral
Metastatic Pulmonary Calcification
Calcium deposition in normal tissue
Tropism for tissues with relative alkaline pH: Upper lung zones, gastric wall, kidney medulla
Due to hypercalcemic condition, most commonly chronic renal failure
HRCT: Mulberry-shaped nodules of amorphous calcification 3-10 mm in diameter in centrilobular location
Sarcoidosis
3.5% develop nephrolithiasis, may be presenting feature
Hypercalciuria (50%), hypercalcemia (20%)
Pulmonary macrophages produce calcitriol
Stones more common in sunny months
Helpful Clues for Rare Diagnoses
Sickle Cell Disease
Due to abnormal hemoglobin, which deforms when deoxygenated
Nephropathies: Papillary necrosis, renal infarcts, pyelonephritis, renal medullary carcinoma
Radiographic manifestations
Lungs: Variable-sized opacities due to pneumonia, atelectasis, or infarcts; interstitial thickening from edema
Cardiac: Cardiomegaly
Skeletal: Osteonecrosis of humeral heads, H-shaped vertebra (10%), enlarged ribs (marrow expansion), bone sclerosis (bone infarcts)
Abdomen: Small or absent spleen
Birt-Hogg-Dubé Syndrome
Facial papules (fibrofolliculomas)
Renal tumors: Range from oncocytomas to renal cell carcinoma
May be bilateral and multifocal
Lungs: Thin-walled cysts, predominantly lower lobes, few in number
Lung cysts closely associated with interlobular septa or visceral pleura
Erdheim Chester Disease
Non-Langerhans cell histiocytosis
Skeletal: Bilateral symmetric osteosclerosis of metaphyses and diaphyses, especially long leg bones (sparing epiphyses)
Renal: Perirenal fat effaced by soft tissue, bilateral and symmetric
Lungs and pleura: Smooth thickening of visceral pleura and fissures, usually bilateral and symmetric
Cardiac: Cardiac enlargement from pericardial or cardiac involvement
Image Gallery
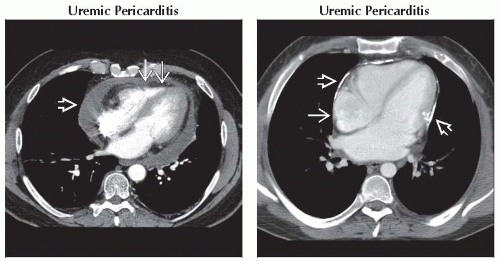 (Left) Axial CECT shows moderate pericardial effusion
 . Tubular shape of the right ventricle . Tubular shape of the right ventricle  suggests mild constriction or tamponade. Pericardial disease may be secondary to uremic toxins, underlying disease (like SLE), or drugs used to treat underlying disease. (Right) Axial CECT shows multiple foci of pericardial calcification suggests mild constriction or tamponade. Pericardial disease may be secondary to uremic toxins, underlying disease (like SLE), or drugs used to treat underlying disease. (Right) Axial CECT shows multiple foci of pericardial calcification  . Right atrium is enlarged . Right atrium is enlarged  . The patient had symptoms of constrictive pericardial disease. . The patient had symptoms of constrictive pericardial disease.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|