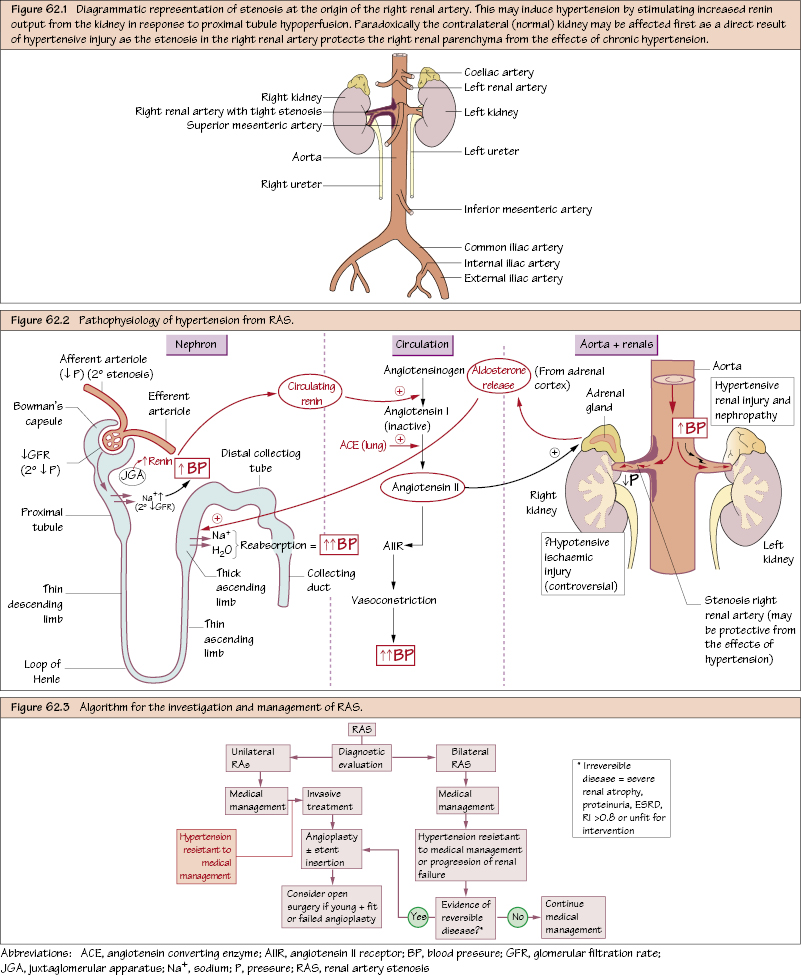
Renal Vascular Disease Renal artery stenosis (RAS) is a stenotic lesion affecting one or both renal arteries. It affects 1–5% of the general population and may be unilateral or bilateral. Although there is no absolute consensus as to what constitutes significant RAS, a stenosis >70% (PSV > 200 cm/s or ratio ≥ 3.5) or a cross-lesion pressure gradient drop of 15–20 mmHg is a useful objective guide. Hypoperfusion of the nephron stimulates sodium re-absorption in the proximal tubule with renin release from the juxta-glomerular apparatus (JGA). Circulating renin cleaves angiotensinogen to form angiotensin I (inactive), which in turn is converted to angiotensin II (AII) by ACE in the lung. AII acts on the AII receptor directly causing vasoconstriction (↑ BP) and stimulates aldosterone-release (adrenal cortex) which leads to Na+ and H2O re-absorption in the distal tubule (↑ BP). Ironically, the RAS-affected kidney may be protected from the hypertension by the stenosis, while the RAS-free contralateral kidney is exposed (leading to atrophy, scarring and eventually renal failure). The contribution of chronic post-RAS renal hypoperfusion towards ipsilateral renal insufficiency is unclear and controversial.
Aetiology
Clinical Presentation
Pathophysiology
Complications of RAS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


