Renal Artery Stenting for Renovascular Hypertension
Matthew J. Dougherty
While a renovascular etiology is present in less than 1% of patients with hypertension, because hypertension is extremely common in Western populations, a substantial number of patients have potentially correctable disease. Atherosclerosis and fibromuscular dysplasia (FMD) are the most common etiologies for renal artery stenosis (RAS). Unfortunately, the prevalence of essential hypertension makes it difficult to separate those patients who may have a secondary cause for hypertension from the rest.
The lack of a sensitive and specific diagnostic test for renovascular hypertension (RVH) has led to difficulty in defining the population at risk. Furthermore, variable employment of diagnostic and therapeutic modalities in different practice settings has led to marked heterogeneity in the clinical data available for analysis.
There remains controversy with regard to benefits of endovascular treatment for RAS. When surgical correction was the primary interventional alternative, the cohort undergoing treatment was very well filtered, with correspondingly positive outcome measures, at least in published reports.
The availability of percutaneous treatment opened the floodgates to a population of patients with more advanced systemic atherosclerosis. Angioplasty without stenting was initially popularized in the 1980s with relatively poor patency and clinical results. The availability of stents, which addressed the aortic ostial nature of atherosclerotic RAS, changed the paradigm. The technical efficacy of the procedure improved substantially. However, clinical efficacy has not clearly paralleled these technical improvements, despite a fourfold increase in the number of patients treated with renal artery stenting in the US Medicare population. To date, no prospective randomized trial has demonstrated improved outcomes in patients undergoing percutaneous treatment for RAS compared with medical therapy. Multiple flaws have been criticized in the trials that have been completed. The inclusion of patients with noncritical renal artery lesions has been questioned, as has the exclusion of patients in whom renal intervention was
felt likely to be beneficial by treating physicians. Several studies were severely underpowered to address the clinical question posed, and very high treatment limb crossover rates, with dubious endpoint definitions, made results difficult to interpret and apply to clinical practice.
felt likely to be beneficial by treating physicians. Several studies were severely underpowered to address the clinical question posed, and very high treatment limb crossover rates, with dubious endpoint definitions, made results difficult to interpret and apply to clinical practice.
Despite these limitations, evidence and experience suggest that in the past two decades, many and perhaps most patients undergoing percutaneous renovascular interventions experienced no clinical benefit. Some believe that renal function decline observed in a substantial subset of treated patients may be related to a proclivity for atheroembolism to the end-arteries of the renal parenchyma occurring at the time the intervention. The lack of a predictable measurable salutary effect on hypertension in addition to an unclear effect on preservation of renal function in many treated patients has perhaps resulted in excessive clinical nihilism regarding renovascular disease. There clearly are still many patients for whom endovascular treatment of RAS is indicated.
Patients who should be evaluated for secondary hypertension include patients with early (under age 30) or late (over 60 years) onset hypertension; those with severe and drug-resistant hypertension; and particularly patients with multidrug hypertension who develop “flash pulmonary edema.” Patients who develop a rise in serum creatinine levels in response to ACE inhibitor therapy are both more likely to have renovascular disease, and to have clinical benefit when such lesions are treated. These patients should be considered for intervention.
There are no absolute contraindications to endovascular therapy for RAS, but patients with exophytic aortic atheroma may be at elevated risk for atheroembolism. Patients who require open aortic surgery may also be better served by operative than endovascular repair where indicated. Controversy remains regarding patients with a solitary kidney with critical stenosis as to whether surgical treatment is safer, which probably depends on the nature of the lesion and the comorbidities of the patient.
Patients referred for evaluation of possible RVH first undergo a detailed history and thorough physical examination. For patients with potential atherosclerotic lesions, a positive history for peripheral arterial disease involving other vascular beds is pertinent. Findings of abdominal or other bruits point toward a potential stenotic lesion. Laboratory data that might suggest RVH include hypokalemic alkalosis, a secondary consequence of elevated aldosterone activity. The role of renin level measurements remains poorly defined, and we have not used these assays in recent years.
Color duplex imaging is an excellent and noninvasive screening study for RAS. In a vascular laboratory with capable technologists and suitable equipment, sensitivity and specificity in detecting critical RAS should both exceed 90%. Duplex has the added advantage of detecting parenchymal renal disease which is associated with a high resistivity index, and which may predict for poor clinical results with renal revascularization. CT angiography and MR angiography can both supplement duplex imaging and can be useful; however, if a RAS has been identified on duplex imaging, and endovascular treatment is indicated, we proceed directly to angiography and concomitant intervention. Severity of stenosis is a critical factor, and disappointing clinical results may often reflect the fact that a treated lesion was not transmitting a significant pressure drop to the afferent arterioles of the renal parenchyma. A diameter reduction of 70% is considered hemodynamically significant and will translate to a pressure gradient of more than 20 mm Hg.
Preprocedure Planning
Patients are fasted as appropriate for use of conscious sedation. All patients are treated with aspirin (325 mg daily) or Plavix (75 mg daily) therapy prior to the procedure. If there is preexisting renal insufficiency (serum creatinine >1.5 mg/dL or creatinine clearance less
than 30 cc/min), preprocedural hydration with normal saline solution is utilized: For inpatients 1 cc/kg/hr for 12 hours before and after the procedure; for outpatients 10 cc/kg bolus 1 hour before procedure and 1 cc/kg/hr until discharge. When available, we also prescribe N-acetyl cysteine (Mucomyst) 600 mg orally twice daily starting 24 hours prior to the procedure and continuing 24 hours after for these patients.
than 30 cc/min), preprocedural hydration with normal saline solution is utilized: For inpatients 1 cc/kg/hr for 12 hours before and after the procedure; for outpatients 10 cc/kg bolus 1 hour before procedure and 1 cc/kg/hr until discharge. When available, we also prescribe N-acetyl cysteine (Mucomyst) 600 mg orally twice daily starting 24 hours prior to the procedure and continuing 24 hours after for these patients.
Prophylactic antibiotic (cefazolin 1 g IV) is administered prior to arterial puncture.
Procedure
The patient is positioned supine on the fluoroscopy table, and after intravenous sedation (typically 1 mg midazolam, 50 µg fentanyl) ultrasound-guided micropuncture access to the common femoral artery is performed. We prefer the femoral artery contralateral to the expected treatment side in patients with unilateral RAS, but either side is sufficient. A short 5-Fr introducer sheath is placed, through which a flush catheter is advanced over a 0.035-in hydrophilic guidewire (e.g., Glidewire, Terumo, Ann Arbor, MI) to the L1 level. Using a fixed imaging system, flush aortography is performed using half-strength nonionic contrast, with magnification to an approximately 15-cm field, utilizing a power injector calibrated for a 20 cc/s injection rate for a volume total of 20 cc, with a 1-second injection delay. The patient should be kept alert enough to perform a breath-hold during the aortogram.
For patients with FMD, lesions tend to be more than 1 cm from the renal ostia, are often sequential with intervening aneurysmal dilatation, and may extend to secondary branches. With atherosclerotic disease, RAS is typically ostial and contiguous with aortic plaque (Fig. 35.1). Care must be exercised with wire and catheter manipulations to minimize risk of plaque disruption and the potential for atheroembolism.
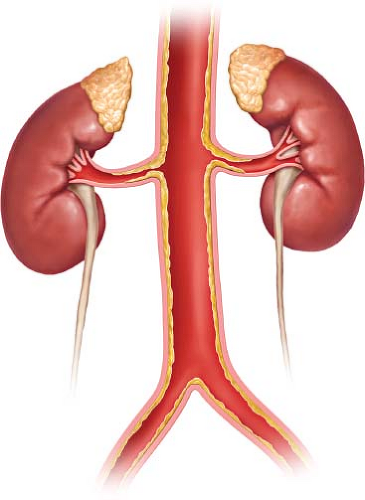 Figure 35.1 Typical atherosclerotic renal artery plaque is ostial and contiguous with aortic plaque. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


