Collaterals to occluded coronary arteries have been observed early after the onset of acute myocardial infarction (AMI). The pressure distal to the occluded segment of the culprit coronary artery (P d ) is generated by collateral flow from the feeding coronary artery supplied by the systemic circulation. The aim of the study was to assess the relation between systemic blood pressure (BP) and P d . Systemic BP and P d were measured simultaneously during intervention of totally occluded coronary arteries in 152 patients admitted for AMI. Patients were divided into groups by time from symptom onset to P d measurement. There was a significant positive correlation between P d and the systolic, diastolic, and mean BPs measured during the first 3 hours from symptom onset (n = 60; p <0.05, p <0.006, and p <0.005, respectively), from 3 to 12 hours (n = 56; p <0.02 for all), and >12 hours after symptom onset (n = 36; p <0.003 for all). The collateral flow, represented by calculated collateral flow index (mean 0.37 ± 0.14, median 0.36), was correlated with mean BP (p = 0.05) but not with diastolic or systolic BP (p = NS) in the overall study population. A direct relation was established during AMI between systemic BP and P d at all time intervals from symptom onset. Collateral flow index correlated with mean BP and was strongly associated with P d at all time intervals. In conclusion, the relation between P d and systemic BP suggests caution when administering therapy that may lower systemic BP during AMI before restoring flow in the occluded culprit artery, as it may compromise collateral pressure and exacerbate myocardial ischemia.
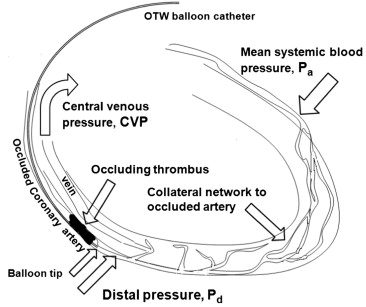
Collaterals, shown to be present already during the first few hours after the onset of acute myocardial infarction (AMI), may confer some protection against ischemic myocardial injury. The systemic blood pressure (BP) determines the flow in the feeding coronary artery that supplies the collateral arteriolar network and generates the distal pressure (P d ) within the occluded segment of the culprit coronary artery. These collaterals perfuse via native arterioles the myocardium and ultimately drain into the coronary veins ( Figure 1 ). The collateral-dependent postocclusive P d provides anterograde flow that partly nourishes the ischemic myocardium subtended by the occluded culprit artery. Occluded coronary arteries treated by percutaneous coronary intervention (PCI) during AMI may be crossed with an over-the-wire balloon, which may allow the measurement of P d . We hypothesized that P d is dependent on the systemic BP that determines flow in the contralateral or homolateral coronary artery giving rise to evolving collaterals. If this is the case, then any excessive decrease in systemic BP before the restoration of anterograde flow might deleteriously affect collateral flow and reduce P d . This, in turn, may diminish perfusion of the ischemic myocardium, with potentially harmful implications. In this study, we investigated in patients sustaining an AMI the relation between the systemic BP and the P d or the collateral flow index (CFI), which reflects the collateral blood supply to the ischemic territory.
Methods
The study population comprised consecutive patients admitted to our coronary care unit for AMI. Study patients were recruited prospectively and had totally occluded culprit coronary arteries with Thrombolysis In Myocardial Infarction (TIMI) flow grade of 0 as observed on angiography and were treated by 1 operator (S.R.M.) on presentation as the primary procedure or as early as possible during admission. Demographic details, laboratory data, and time interval from symptom onset to intervention were recorded, as well as clinical data during admission and at discharge. The local institutional review board approved the study. No extramural funding was used to support this work.
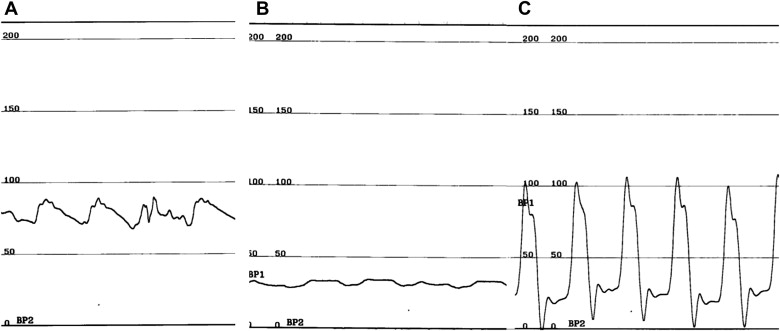
The study procedure and method have been described and validated previously. In brief, an occluded culprit artery was identified on coronary angiography. The collateral grade before intervention was determined at this stage according to Rentrop et al. Crossing the occlusion was accomplished with a guidewire supported by an over-the-wire angioplasty balloon that was advanced to the lumen beyond the estimated distal edge of the occlusion. Contrast injected through the guiding catheter ensured persistence of the obstruction despite lesion crossing, because pressure measurements were eligible for analysis by protocol only if TIMI flow grade was 0. After aspiration of blood and careful flushing of the balloon catheter with saline, mean BP was measured at the guiding catheter tip, and P d was measured at the balloon tip beyond the coronary obstruction ( Figure 2 ). Dilute contrast was injected through the balloon catheter to confirm appropriate position within the main vessel lumen. The guidewire was then reintroduced and intervention completed. The CFI was calculated according to Pijls et al and Seiler et al as (P d − central venous pressure)/(mean BP − central venous pressure) (all pressures in millimeters of mercury). Central venous pressure was substituted by 5 mm Hg or by 10 mm Hg in patients with overt signs of increased systemic venous pressure. To evaluate the kinetics of the P d and collateral flow evolution after acute occlusion, patients were divided into 3 groups according to time interval from symptom onset to measurement: 1 to 3, 3 to 12, and >12 hours.
Data are expressed as mean ± SD (median). The correlations between various measured BP values or their ratios were evaluated using Pearson’s test for continuous variables or Spearman correlation for categorical variables, as appropriate. The Kruskal-Wallis test was applied for the evaluation of the significance of the association between collateral grade and P d or CFI. Analysis of variance was used for evaluation of the trend of P d by time interval. A p value <0.05 was considered statistically significant. SPSS version 15 (SPSS, Inc., Chicago, Illinois) was used for statistical analysis.
Results
One-hundred and sixty-two consecutive patients admitted for AMI with a total obstruction of the culprit coronary artery were eligible for the study. Of these, 10 patients were excluded: 7 patients whose occluded coronary arteries partially recanalized upon passage of the guidewire during angioplasty, 2 patients in whom attempts to cross the lesion were unsuccessful, and 1 patient whose admission chart could not be found. The remaining 152 patients constituted the study cohort (mean age 57 ± 12 years, median 56), of whom 125 were men (82%). Most patients presented with ST-segment elevation myocardial infarctions (84%; Table 1 ), and 74 patients (49%) underwent primary PCI. Table 1 lists the prevalence in the study cohort of atherosclerosis risk factors, co-morbid conditions, infarct territory, culprit artery, collateral grade, and extent of coronary disease according to time from symptom onset to pressure measurement. No difference in the incidence of diabetes mellitus, smoking, hypertension, or hypercholesterolemia was noted among study groups.
| Variable | Time from Onset (h) | Overall (n = 152) | p Value | ||
|---|---|---|---|---|---|
| <3 (n = 60) | 3–12 (n = 56) | >12 (n = 36) | |||
| Age (yrs), mean ± SD | 58 ± 11 | 55 ± 13 | 59 ± 14.3 | 57 ± 12.5 | 0.30 |
| Men | 50 (83%) | 48 (86%) | 26 (74%) | 125 (82%) | 0.36 |
| Smokers | 34 (57%) | 31 (55%) | 16 (46%) | 81 (53%) | 0.56 |
| Past smokers | 8 (13%) | 5 (9%) | 2 (6%) | 15 (10%) | 0.46 |
| Diabetes mellitus | 16 (27%) | 20 (36%) | 15 (43%) | 51 (34%) | 0.25 |
| Hyperlipidemia | 40 (67%) | 37 (66%) | 24 (69%) | 101 (66%) | 0.96 |
| Hypertension | 24 (40%) | 24 (43%) | 10 (29%) | 58 (38%) | 0.37 |
| Chronic renal failure | 5 (8%) | 4 (7%) | 3 (9%) | 12 (8%) | 0.96 |
| First presentation of coronary artery disease | 52 (87%) | 44 (79%) | 25 (71%) | 121 (80%) | 0.19 |
| Primary PCI | 38 (63%) | 31 (55%) | 4 (11%) | 74 (49%) | <0.0001 ∗,† |
| Preadmission angina | 7 (12%) | 2 (4%) | 1 (3%) | 10 (7%) | 0.13 |
| ST-segment elevation myocardial infarction | 56 (93%) | 50 (89%) | 22 (61%) | 128 (84%) | 0.002, ∗ <0.0001 † |
| Infarct territory | |||||
| Inferior | 17 (28%) | 33 (59%) | 11 (31%) | 61 (40%) | 0.017, ∗ 0.001 ‡ |
| Anterior | 33 (55%) | 14 (25%) | 13 (37%) | 60 (40%) | 0.001 ‡ |
| Culprit coronary artery | |||||
| Left anterior descending | 34 (57%) | 13 (23%) | 14 (39%) | 61 (40%) | <0.0001 ‡ |
| Right | 23 (38%) | 31 (55%) | 12 (33%) | 66 (43%) | 0.054 ∗ |
| Left circumflex | 11 (18%) | 14 (25%) | 8 (22%) | 33 (22%) | 0.68 |
| Rentrop collateral grade = 0 | 27 (47%) | 19 (34%) | 2 (6%) | 48 (32%) | <0.0001, † 0.002 ∗ |
| Number of narrowed coronary arteries | |||||
| 1 | 41 (68%) | 36 (64%) | 19 (54%) | 97 (64%) | 0.38 |
| 2 | 16 (27%) | 10 (19%) | 12 (34%) | 38 (25%) | 0.20 |
| 3 | 3 (5%) | 10 (19%) | 4 (11%) | 17 (11%) | 0.04 ‡ |
Systolic, diastolic, and mean BP and CFI showed normal Gaussian distributions, with values unchanged over time from the onset of AMI to measurement during PCI ( Table 2 ). P d , in contrast, increased as time from onset to measurement elapsed ( Table 2 ). In the entire study population, P d correlated significantly with systolic BP, diastolic BP, and mean BP (p <0.0001; Figure 3 ). P d , measured <3 hours after symptom onset, correlated with simultaneous systolic BP (R = 0.26, p <0.05), diastolic BP (R = 0.35, p <0.006) and mean BP (R = 0.37, p <0.004). Similarly, P d measured during PCI performed 3 to 12 hours after symptom onset correlated with simultaneous systolic BP (R = 0.35), diastolic BP (R = 0.35), and mean BP (R = 0.36) (p <0.008 for all), as was P d measured >12 hours after symptom onset (R = 0.49 [p <0.003], R = 0.45 [p <0.006], and R = 0.5 [p <0.002] for systolic, diastolic, and mean BP, respectively). In addition, a statistically significant correlation between CFI and P d , was observed (p <0.0001; Figure 4 ), as well as a correlation between CFI and mean BP (R = −0.16, p = 0.05). However, no relation between CFI and systolic BP (R = −0.13, p = 0.11) or diastolic BP (R = −0.14, p = 0.08) was found.



