In-hospital cardiac arrest (IHCA) is common and is associated with poor prognosis. Data on the effect of smoking on outcomes after IHCA are limited. We analyzed the Nationwide Inpatient Sample databases from 2003 to 2011 for all patients aged ≥18 years who underwent cardiopulmonary resuscitation (CPR) for IHCA to examine the differences in survival to hospital discharge and neurologic status between smokers and nonsmokers. Of the 838,464 patients with CPR for IHCA, 116,569 patients (13.9%) were smokers. Smokers were more likely to be younger, Caucasian, and male. They had a greater prevalence of dyslipidemia, coronary artery disease, hypertension, chronic pulmonary disease, obesity, and peripheral vascular disease. Atrial fibrillation, heart failure, and diabetes mellitus with complications were less prevalent in smokers. Smokers were more likely to have a primary diagnosis of acute myocardial infarction (14.8% vs 9.1%, p <0.001) and ventricular tachycardia or ventricular fibrillation as the initial cardiac arrest rhythm (24.3% vs 20.5%, p <0.001). Smokers had a higher rate of survival to hospital discharge compared with nonsmokers (28.2% vs 24.1%, adjusted odds ratio 1.06, 95% confidence interval 1.05 to 1.08, p <0.001). Smokers were less likely to have a poor neurologic status after IHCA compared with nonsmokers (3.5% vs 3.9%, adjusted odds ratio 0.92, 95% confidence interval 0.89 to 0.95, p <0.001). In conclusion, among patients aged ≥18 years who underwent CPR for IHCA, we observed a higher rate of survival in smokers than nonsmokers—consistent with the “smoker’s paradox.” Smokers were also less likely to have a poor neurologic status after IHCA.
Smoking is the leading preventable cause of morbidity and mortality in the United States. Although cigarette smokers have higher rates of acute myocardial infarction (AMI) than nonsmokers, multiple studies have shown a lower mortality rate after AMI in smokers. This phenomenon, termed the “smoker’s paradox,” has largely been attributed to younger age of and fewer co-morbidities in smokers. However, some studies have shown that the association between smoking and improved survival after AMI persists even after adjustment for these variables. Smoking has also been found to be associated with lower risk-adjusted in-hospital mortality in patients with acute heart failure and patients with acute ischemic stroke. Although smoking is a well-defined risk factor for cardiac arrest, data on the effect of smoking on outcomes after in-hospital cardiac arrest (IHCA) are limited. Given potential physiological similarities of IHCA with AMI, acute heart failure, and acute ischemic stroke, it is possible that a history of smoking may be associated with improved outcomes after cardiopulmonary resuscitation (CPR) of IHCA. The primary objective of this study was to examine the association of smoking status with outcomes after IHCA using the Nationwide Inpatient Sample databases from 2003 to 2011.
Methods
Data were obtained from the 2003 to 2011 Nationwide Inpatient Sample databases. The Nationwide Inpatient Sample, sponsored by the Agency for Healthcare Research and Quality as a part of Healthcare Cost and Utilization Project, is the largest publicly available all-payer inpatient care database in the United States. It contains discharge-level data from approximately 8 million hospital stays from about 1,000 hospitals designed to approximate a 20% stratified sample of all community hospitals in the United States. Criteria used for stratified sampling of hospitals include hospital ownership, patient volume, teaching status, urban or rural location, and geographic region. Discharge weights are provided for each patient discharge record, which were used to obtain national estimates.
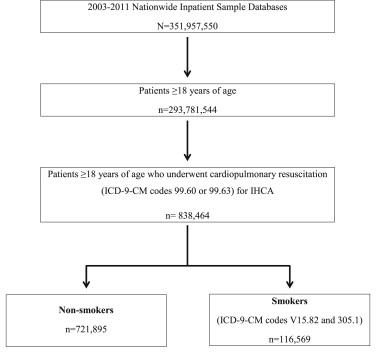
We used the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 99.60 or 99.63 to identify all patients aged ≥18 years who underwent CPR for IHCA (n = 838,464; Figure 1 ). This approach has been used in previous studies using administrative databases to accurately identify patients with IHCA. Smokers were then identified using ICD-9-CM codes V15.82 or 305.1 (n = 116,569). Patients who did not have either of these ICD-9-CM codes were considered as nonsmokers (n = 721,895). Previous study has shown that these ICD-9-CM codes have a sensitivity of 100%, a specificity of 32%, and an accuracy of 66% to identify smokers in a general patient population with little evidence of documentation bias.
Our primary outcome of interest for this study was survival to hospital discharge. We used poor neurologic status (defined as coma [ICD-9-CM code 780.01], persistent vegetative state [ICD-9-CM code 780.03], or brain death [ICD-9-CM code 348.82]) as the secondary outcome.
Baseline patient characteristics used included demographics (age, gender, and race), primary expected payer, weekday versus weekend admission, median household income for patient’s zip code, 29 Elixhauser co-morbidities as defined by the Agency for Healthcare Research and Quality, other clinically relevant co-morbidities (dyslipidemia, known coronary artery disease, family history of coronary artery disease, previous myocardial infarction, previous transient ischemic attack or stroke, previous percutaneous coronary angioplasty, previous coronary artery bypass grafting, previous cardiac arrest, family history of sudden cardiac death, carotid artery disease, dementia, and atrial fibrillation), primary diagnosis of AMI, and initial cardiac arrest rhythm. A list of ICD-9-CM and Clinical Classifications Software codes used to identify co-morbidities is provided in Supplementary Table 1 . Hospital characteristics such as hospital region (Northeast, Midwest, South, and West), number of beds (small, medium, and large), location (rural and urban), and teaching status were also included.
We initially compared baseline patient and hospital characteristics between the 2 groups using Pearson’s chi-square test for categorical variables and Student t test for continuous variables to identify significant univariate associations. Multivariate logistic regression was used to compare outcomes between the 2 groups. The regression model adjusted for demographics, primary expected payer, weekday versus weekend admission, median household income, all Elixhauser co-morbidities, other clinically relevant co-morbidities (dyslipidemia, known coronary artery disease, family history of coronary artery disease, previous myocardial infarction, previous transient ischemic attack or stroke, previous percutaneous coronary angioplasty, previous coronary artery bypass grafting, previous cardiac arrest, family history of sudden cardiac death, carotid artery disease, dementia, and atrial fibrillation), primary diagnosis of AMI, and initial cardiac arrest rhythm.
Statistical analysis was performed using IBM SPSS Statistics 20.0 (IBM Corp., Armonk, New York). We used a 2-sided p value of <0.05 to assess for statistical significance for all analyses. Categorical variables are expressed as percentage and continuous variables as mean ± SD. Odds ratio (OR) and 95% confidence interval (CI) are used to report the results of logistic regression.
Results
From 2003 to 2011, of the 838,464 patients with CPR for IHCA, 116,569 patients (13.9%) were smokers. Smokers were more likely to be younger, Caucasian, and male (p <0.001). They were also more likely to have dyslipidemia, coronary artery disease, family history of coronary artery disease, previous myocardial infarction, previous transient ischemic attack or stroke, previous percutaneous coronary angioplasty, previous coronary artery bypass grafting, previous cardiac arrest, alcohol abuse, deficiency anemia, chronic blood loss anemia, chronic pulmonary disease, depression, drug abuse, hypertension, liver disease, metastatic cancer, obesity, peripheral vascular disease, psychoses, pulmonary circulation disorders, and solid tumor without metastasis (p <0.001 for all). Dementia, atrial fibrillation, heart failure, coagulopathy, diabetes mellitus with complications, hypothyroidism, lymphoma, fluid and electrolyte disorder, other neurologic disorders, paralysis, chronic renal failure, valvular disease, and weight loss were less prevalent in smokers (p <0.001 for all). Smokers were more likely to be admitted to large nonteaching hospitals (p <0.001). They were also more likely to have a primary diagnosis of AMI and ventricular tachycardia or fibrillation as the cardiac arrest rhythm ( Table 1 ).
| Variable | Non-Smokers | Smokers | p Value |
|---|---|---|---|
| (n = 721,895) | (n = 116,569) | ||
| Age, mean ± standard deviation (years) | 67.8 ± 16.3 | 63.7 ± 14.2 | <0.001 |
| Women | 46.9% | 36.2% | <0.001 |
| Caucasian | 62.6% | 72.8% | <0.001 |
| African-American | 20.7% | 15.8% | |
| Hispanic | 10.1% | 6.8% | |
| Asian or Pacific Islander | 3.3% | 2.0% | |
| Other | 3.3% | 2.6% | |
| Primary expected payer | <0.001 | ||
| Medicare | 65.8% | 55.3% | |
| Medicaid | 9.8% | 11.9% | |
| Private insurance | 17.6% | 21.8% | |
| Uninsured | 4.8% | 8.0% | |
| Other | 2.0% | 3.1% | |
| Weekend admission | 23.7% | 23.9% | 0.207 |
| Median household income (percentile) | <0.001 | ||
| 0–25th | 31.3% | 30.7% | |
| 26th–50th | 25.6% | 26.9% | |
| 51st–75th | 23.1% | 24.5% | |
| 76th–100th | 20.0% | 17.9% | |
| Co-morbidities ∗ | |||
| Dyslipidemia | 15.8% | 28.7% | <0.001 |
| Coronary artery disease | 25.6% | 36.1% | <0.001 |
| Family history of coronary artery disease | 0.5% | 2.7% | <0.001 |
| Prior myocardial infarction | 4.8% | 9.3% | <0.001 |
| Prior transient ischemic attack/stroke | 1.9% | 3.8% | <0.001 |
| Prior percutaneous coronary intervention | 2.8% | 6.9% | <0.001 |
| Prior coronary bypass | 5.2% | 7.4% | <0.001 |
| Prior cardiac arrest | 0.2% | 0.5% | <0.001 |
| Family history of sudden cardiac death | <0.1% | <0.1% | 0.140 |
| Carotid artery disease | 0.8% | 1.5% | <0.001 |
| Dementia | 6.5% | 3.4% | <0.001 |
| Atrial fibrillation | 23.5% | 19.6% | <0.001 |
| AIDS | 0.3% | 0.4% | 0.010 |
| Alcohol abuse | 4.2% | 12.2% | <0.001 |
| Deficiency anemia | 20.5% | 21.4% | <0.001 |
| Rheumatoid arthritis/collagen vascular diseases | 2.4% | 2.3% | 0.829 |
| Chronic blood loss anemia | 2.0% | 1.6% | <0.001 |
| Congestive heart failure | 36.3% | 30.6% | <0.001 |
| Chronic pulmonary disease | 23.0% | 42.0% | <0.001 |
| Coagulopathy | 13.5% | 11.6% | <0.001 |
| Depression | 5.0% | 8.1% | <0.001 |
| Diabetes mellitus (uncomplicated) | 22.1% | 22.4% | 0.077 |
| Diabetes mellitus (complicated) | 7.8% | 5.2% | <0.001 |
| Drug abuse | 2.3% | 6.4% | <0.001 |
| Hypertension | 49.2% | 56.4% | <0.001 |
| Hypothyroidism | 8.5% | 8.3% | 0.009 |
| Liver disease | 4.1% | 5.3% | <0.001 |
| Lymphoma | 1.4% | 1.0% | <0.001 |
| Fluid and electrolyte disorder | 48.7% | 45.9% | <0.001 |
| Metastatic cancer | 3.8% | 4.7% | <0.001 |
| Other neurological disorders | 11.5% | 9.5% | <0.001 |
| Obesity | 7.5% | 11.2% | <0.001 |
| Paralysis | 3.7% | 2.3% | <0.001 |
| Peripheral vascular disease | 9.1% | 13.6% | <0.001 |
| Psychoses | 3.1% | 4.5% | <0.001 |
| Pulmonary circulation disorders | 4.7% | 5.5% | <0.001 |
| Renal failure (chronic) | 24.8% | 17.3% | <0.001 |
| Solid tumor without metastasis | 2.9% | 4.2% | <0.001 |
| Peptic ulcer (non-bleeding) | <0.1% | <0.1% | 0.533 |
| Valvular disease | 5.9% | 4.8% | <0.001 |
| Weight loss | 10.2% | 8.8% | <0.001 |
| Hospital characteristics | |||
| Number of beds † | <0.001 | ||
| Small | 10.0% | 9.2% | |
| Medium | 24.7% | 23.9% | |
| Large | 65.3% | 66.9% | |
| Urban location | 90.7% | 90.5% | 0.111 |
| Teaching hospital | 44.7% | 41.5% | <0.001 |
| Region | <0.001 | ||
| Northeast | 20.3% | 13.2% | |
| Midwest | 18.8% | 20.7% | |
| South | 37.6% | 38.6% | |
| West | 23.3% | 25.5% | |
| Ventricular tachycardia/fibrillation | 20.5% | 24.3% | <0.001 |
| Primary diagnosis of acute myocardial infarction | 9.1% | 14.8% | <0.001 |
∗ Co-morbidities (including the 29 Elixhauser co-morbidities) were extracted from the database using International Classification of Diseases, Ninth Edition, Clinical Modification diagnosis or Clinical Classification Software codes.
† Number of beds categories are specific to hospital location and teaching status, available at http://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


