Potassium plays a key role in normal myocardial function, and current guidelines recommend that serum potassium levels be maintained from 4.0 to 5.0 mEq/L in patients with acute myocardial infarction (AMI). However, the impact of serum potassium levels on long-term mortality has not been evaluated. We retrospectively studied 1,924 patients diagnosed with AMI. The average serum potassium levels measured throughout the hospitalization were obtained and statistically analyzed. Patients were categorized into 5 groups to determine the relation between mean serum potassium and long-term mortality: <3.5, 3.5 to <4.0, 4.0 to <4.5, 4.5 to <5.0, and ≥5 mEq/L. The long-term mortality was lowest in the group of patients with potassium levels of 3.5 to <4.0 mEq/L, whereas mortality was higher in the patients with potassium levels ≥4.5 or <3.5 mEq/L. In a multivariate Cox-proportional regression analysis, the mortality risk was greater for serum potassium levels of >4.5 mEq/L (hazard ratio [HR] 1.71, 95% confidence interval [CI] 1.04 to 2.81 and HR 4.78, 95% CI 2.14 to 10.69, for patients with potassium levels of 4.5 to <5.0 mEq/L and ≥5.0, respectively) compared with patients with potassium levels of 3.5 to <4.0 mEq/L. The mortality risk was also higher for patients with potassium levels <3.5 mEq/L (HR 1.55, 95% CI 0.94 to 2.56). In contrast to the association with long-term mortality, there was no relation between serum potassium levels and the occurrence of ventricular arrhythmias. The results of the current analysis suggest that there is a need for change in our current concepts of the ideal serum potassium levels in patients with AMI.
Potassium is an important determinant of myocardial function and hypokalemia, usually defined as <3.5 mEq/L, has frequently been observed in patients with acute myocardial infarction (AMI), and is associated with arrhythmia and sudden cardiac death. Based on previous studies, the current clinical guidelines recommend that serum potassium levels be maintained at ≥4 mEq/L or even ≥4.5 mEq/L in patients with AMI. However, these recommendations are based on a relatively low quality of evidence—experimental work or small observational studies, most of which were conducted more than 20 years ago. Since then, there have been substantial changes in the management of AMI, it is therefore necessary to re-evaluate the optimal level of serum potassium with respect to mortality and the incidence of ventricular arrhythmias in patients with AMI. Recently, Goyal et al reported that the lowest in-hospital mortality was observed in patients with potassium levels of 3.5 to <4.0 mEq/L and raised questions about current guidelines that recommend maintaining serum potassium levels at >4 mEq/L in patients with AMI. To address this critical discordance, the above result needs to be confirmed by further research. The present study aimed to assess the effect of serum potassium level on long-term mortality and on the incidence of ventricular arrhythmias in patients with AMI.
Methods
A total of 2,289 patients who were admitted to the emergency department of Chonnam National University Hospital from January 2006 to October 2009 with a diagnosis of MI were evaluated retrospectively. Of these patients, 305 who did not have at least 2 serum potassium measurements during their hospitalization were excluded from the study, and an additional 60 patients were excluded because they met the following exclusion criteria: lack of follow-up data after discharge (n = 35) and end-stage renal disease with dialysis (n = 25).
Demographic, clinical, laboratory, and treatment data were obtained from the hospital’s computerized database. AMI was diagnosed on the basis of the triad of chest pain, electrocardiogram changes, and elevated serum cardiac enzyme levels. ST-segment elevation myocardial infarction was defined as the presence of new ST-segment elevation of at least 1 mm (0.1 mV) in continuous leads or new left bundle-branch block on the index electrocardiogram. Patients not classified as ST-segment elevation myocardial infarction were considered to have non–ST-segment elevation myocardial infarction on the basis of positive biomarkers. This study was approved by the institutional review board of the Chonnam National University Hospital, Gwangju, Republic of Korea.
Serial serum potassium levels during hospitalization were obtained from the patients’ medical records and reviewed by a trained study coordinator. The mean potassium level was defined as the average of all potassium levels measured during hospitalization. Patients were categorized into 5 groups to determine the relation between mean serum potassium and long-term mortality: <3.5, 3.5 to <4.0, 4.0 to <4.5, 4.5 to <5.0, and ≥5 mEq/L. The primary end point of the study was 3-year mortality after AMI. Assessment of the survival status and validation of the clinical outcomes were performed by collecting records from the outpatients clinic or by follow-up telephone interviews. The occurrence of ventricular arrhythmias was determined from the patients’ medical records during hospitalization, which were reviewed by a trained study coordinator. Ventricular arrhythmias were classified as ventricular tachycardia (VT) or ventricular fibrillation, and VT was further categorized into sustained and nonsustained VT, depending on the occurrence or not of tachycardia lasting more than 30 s and leading to hemodynamic collapse. Left ventricular ejection fraction was evaluated by echocardiogram that performed in 98% patients at 1.08 ± 2.10 days after admission.
Continuous variables with normal distributions are expressed as mean ± SD and were compared using one-way analysis of variance. Continuous variables with a skewed distribution are presented as median (with 25th and 75th percentiles) and were compared using the Kruskal-Wallis test. Pearson’s chi-square or Fisher’s exact test were used to evaluate the differences in categorical variables, which are expressed as numbers and percentages. Cox proportional regression analysis was used to compare 3-year mortality by categories of mean serum potassium level. Patients lost to follow-up were censored at the date of last follow-up. The hazard ratios indicate the relative risk of death in each potassium level group compared with those in the lowest-risk potassium group (3.5 to <4.0 mEq/L). The confounders analyzed included age, gender, Killip classification, left ventricular ejection fraction, co-morbidities (hypertension, diabetes mellitus, ischemic heart disease, hyperlipidemia, and smoking status), diagnosis (ST-segment elevation myocardial infarction vs non–ST-segment elevation myocardial infarction), in-hospital procedure (coronary angiography [CAG], percutaneous coronary intervention, thrombolysis, and coronary artery bypass graft), estimated glomerular filtration rate calculated by the Chronic Kidney Disease-Epidemiology Collaboration equation, cardiac enzymes (peak troponin-I during hospitalization), and medical treatment during hospitalization. Increasingly adjusted models were built for 3-year mortality to assess the relative confounding effect of certain factors. Multivariable logistic regression analysis was conducted to determine the risk of ventricular arrhythmias during hospitalization according to each potassium category, and the same variables mentioned above were used for multivariable analysis. All statistical tests were 2-tailed, and p Values <0.05 were considered significant. Statistical analysis was performed using the Statistical Package for Social Sciences software, version 18.0 (SPSS; IBM, Armonk, New York).
Results
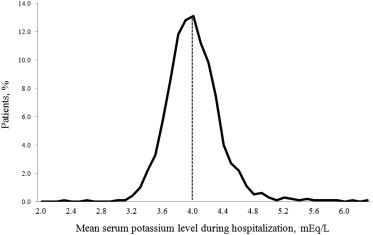
A total of 1,924 patients (mean age 64.0 ± 12.8 years; men 69%) were included in the present study. Figure 1 shows the distribution of the serum potassium levels measured during hospitalization, which was approximately a normal distribution with a mean of 3.99 ± 0.35 mEq/L. The patients’ clinical characteristics, stratified by mean serum potassium level, are listed in Table 1 . There were complex differences in clinical characteristics among the groups, especially at the extremes of serum potassium level (≥5 or <3.5 mEq/L). With regard to clinical outcomes, the lowest mortality occurred in patients with potassium levels of 3.5 to <4.0 mEq/L.
| Mean Serum Potassium Level, mEq/L (n = 1,924) | p Value | |||||
|---|---|---|---|---|---|---|
| <3.5 (n = 96) | 3.5−<4.0 (n = 907) | 4.0−<4.5 (n = 784) | 4.5−<5.0 (n = 113) | ≥5.0 (n = 24) | ||
| Age (yrs) | 67 ± 13 | 64 ± 13 | 63 ± 13 | 66 ± 12 | 70 ± 14 | 0.005 |
| Men | 44 (45) | 589 (64) | 607 (77) | 81 (71%) | 14 (58) | <0.001 |
| Potassium (mEq/L) | 3.3 ± 0.2 | 3.8 ± 0.1 | 4.2 ± 0.1 | 4.6 ± 0.1 | 5.4 ± 0.4 | <0.001 |
| Number of potassium measurements per patient | 5.1 ± 3.4 | 4.9 ± 5.7 | 5.1 ± 6.3 | 4.9 ± 4.9 | 4.0 ± 2.9 | 0.848 |
| History | ||||||
| Hypertension | 61 (63) | 431 (47) | 356 (45) | 65 (57) | 18 (75) | <0.001 |
| Diabetes mellitus | 22 (22) | 191 (21) | 244 (31) | 58 (51) | 12 (50) | <0.001 |
| Ischemic heart disease | 12 (12) | 113 (12) | 107 (13) | 16 (14) | 4 (16) | 0.918 |
| Hyperlipidemia | 2 (2) | 39 (4) | 41 (5) | 6 (5) | 0 (0) | 0.466 |
| Smoking | 38 (39) | 520 (57) | 512 (65) | 63 (55) | 13 (54) | <0.001 |
| At admission | ||||||
| Systolic blood pressure (mm Hg) | 123 ± 42 | 129 ± 29 | 129 ± 29 | 131 ± 30 | 119 ± 54 | 0.161 |
| Diastolic blood pressure (mm Hg) | 77 ± 26 | 80 ± 18 | 80 ± 18 | 83 ± 19 | 73 ± 33 | 0.083 |
| Heart rate (rate/min) | 72.4 ± 25.4 | 75.3 ± 19.4 | 76.2 ± 18.5 | 79.8 ± 19.8 | 79.4 ± 33.2 | 0.053 |
| Killip classification | 1.7 ± 1.0 | 1.5 ± 0.9 | 1.4 ± 0.8 | 1.6 ± 0.9 | 1.8 ± 1.1 | 0.004 |
| Left ventricular ejection fraction (%) | 54.6 ± 14.1 | 54.2 ± 12.3 | 54.4 ± 12.6 | 54.4 ± 12.6 | 49.3 ± 17.6 | 0.514 |
| Diagnosis | 0.235 | |||||
| ST-segment elevated myocardial infarction | 53 (55) | 543 (59) | 475 (60) | 63 (55) | 19 (79) | |
| Non-ST-segment elevated myocardial infarction | 43 (44) | 364 (40) | 309 (39) | 50 (44) | 5 (20) | |
| Laboratory variables | ||||||
| Peak troponin-I (ng/ml) | 26 (7,63) | 30 (9,73) | 31 (8,78) | 21 (6,65) | 30 (9,88) | 0.308 |
| Peak creatine kinase-MB (ng/ml) | 34 (14,100) | 47 (14,119) | 38 (13,111) | 32 (12,103) | 61 (12,320) | 0.276 |
| Creatinine (mg/dl) | 0.96 ± 0.43 | 0.95 ± 0.39 | 1.06 ± 0.42 | 1.40 ± 0.91 | 1.63 ± 0.84 | <0.001 |
| eGFR ∗ (ml/min/1.73 m 2 ) | 76 ± 23 | 81 ± 22 | 76 ± 24 | 63 ± 28 | 49 ± 26 | <0.01 |
| In-hospital procedure | ||||||
| CAG | 96 (100) | 899 (99) | 777 (99) | 111 (98) | 23 (95) | 0.342 |
| Percutaneous angioplasty | 76 (80) | 780 (87) | 659 (85) | 74 (84) | 20 (87) | 0.276 |
| Thrombolysis | 5 (5) | 70 (7) | 58 (7) | 7 (6) | 0 (0) | 0.563 |
| Coronary artery bypass graft | 0 (0) | 6 (0) | 33 (4) | 2 (1) | 0 (0) | <0.001 |
| In-hospital medication | ||||||
| Aspirin | 96 (100) | 892 (98) | 781 (99) | 111 (98) | 23 (95) | 0.041 |
| Clopidogrel | 94 (97) | 889 (98) | 770 (98) | 110 (97) | 23 (95) | 0.907 |
| Anticoagulant | 96 (100) | 897 (98) | 777 (99) | 112 (99) | 23 (95) | 0.456 |
| β blocker | 75 (78) | 756 (83%) | 681 (86) | 91 (80) | 14 (58) | <0.001 |
| Calcium channel blocker | 19 (19) | 89 (9) | 81 (10) | 15 (13) | 1 (4) | 0.026 |
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 78 (81) | 797 (87) | 715 (91) | 92 (81) | 12 (50) | <0.001 |
| Statin | 56 (58) | 632 (69) | 556 (70) | 79 (69) | 9 (37) | 0.001 |
| Aldosterone antagonist | 20 (20) | 162 (17) | 125 (15) | 17 (15) | 3 (12) | 0.601 |
| Diuretics | 48 (50) | 297 (32) | 232 (29) | 45 (39) | 15 (62) | <0.001 |
| Potassium supplement | 76 (79) | 308 (33) | 123 (15) | 9 (8) | 2 (8) | <0.001 |
| Clinical outcomes | ||||||
| In-hospital mortality | 6 (6) | 27 (3) | 25 (3) | 11 (9) | 14 (58) | <0.001 |
| 3-yr all-cause mortality | 20 (20) | 109 (12) | 97 (12) | 25 (22) | 15 (62) | <0.001 |
| Ventricular arrhythmia during hospitalization | 9 (9) | 70 (7) | 46 (5) | 9 (8) | 3 (12) | 0.447 |
The patients were followed up for a mean period of 3.58 ± 1.96 years. The duration of follow-up was right censored at 3 years for Cox proportional regression analysis. Table 2 lists unadjusted and adjusted Cox proportional regression analysis for 3-year mortality according to serum potassium levels. Unadjusted analysis showed a U-shaped relation between serum potassium levels and long-term mortality risk, and this relation persisted even after adjustment for several confounders. Compared with the reference group (3.5 to <4.0 mEq/L), patients with potassium levels of 4.0 to <4.5 mEq/L showed a similar mortality risk, whereas the mortality risk was higher for serum potassium levels of >4.5 mEq/L. Although the level of statistical significance was only borderline, the mortality risk was also higher for patients with potassium levels <3.5 mEq/L.



