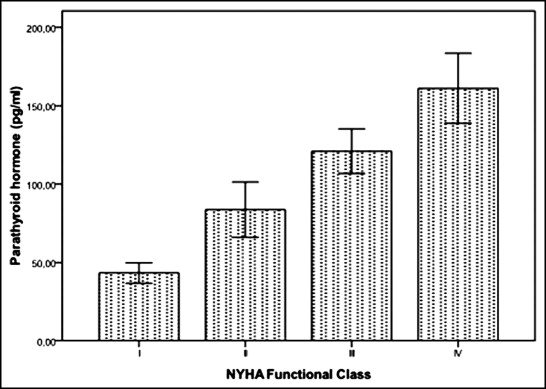
Increased parathyroid hormone (PTH) level is associated with all-cause mortality in patients with heart failure (HF). However its role for identifying advanced HF has not been previously studied. We aimed to investigate whether the assessment of serum PTH could enable clinicians to identify patients with advanced HF. One hundred fifty consecutive patients who visited our outpatient clinic with systolic HF were enrolled in the present study. Serum levels of PTH and brain natriuretic peptide (BNP) were measured across all New York Heart Association functional classes. Mean levels of PTH were 43 ± 19, 84 ± 56, 121 ± 47, and 161 ± 60 pg/ml in New York Heart Association functional classes I, II, III, and IV, respectively (p <0.001). In univariate analysis, body mass index, disease duration, PTH, BNP and hemoglobin levels, creatinine clearance, heart rate, systolic blood pressure, left ventricular ejection fraction, left ventricular diastolic diameter, left atrial size, presence of atrial fibrillation, and diuretic usage were found to be predictors of advanced HF. In multivariate logistic regression analysis, PTH level (hazard ratio 1.032, 95% confidence interval 1.003 to 1.062, p = 0.003) and body mass index (hazard ratio 0.542, 95% confidence interval 0.273 to 1.075, p = 0.079) were associated with advanced HF. Furthermore, serum PTH levels were correlated with BNP level and left ventricular ejection fraction (p <0.001 for the 2 comparisons). In receiver operator characteristics curve analysis, the optimal cut-off value of PTH to predict advanced HF was >96.4 pg/ml, with 93.3% sensitivity and 64.2% specificity. In conclusion, measurement of serum PTH could provide complementary information and a simple biomarker strategy to categorize patients with advanced HF based on increased PTH levels, allowing rapid risk stratification in these patients.
Hyperparathyroidism is associated with heart failure (HF) in patients with primary and secondary aldosteronism. Increased serum parathyroid hormone (PTH) levels are thought to be related to the systemic induction of oxidative stress that contributes to loss of soft tissues and bone that eventuates in a wasting syndrome termed “cardiac cachexia.” The present study was conducted in 2 participating centers to determine whether circulating levels of PTH in outpatients could identify advanced HF and the need for referral for advanced-stage therapies without delay.
Methods
One hundred fifty consecutive outpatients with systolic HF were enrolled into the current study after obtaining informed consent in 2 participating centers. Left ventricular ejection fraction (LVEF) was <40% on echocardiogram in all patients. Patients with creatinine clearance <60%, recent exacerbation within 1 month, long-term alcoholism, sepsis, pancreatitis, primary hyperparathyroidism, cancer, severe hepatic disease, and those taking spironolactone were excluded.
Blood samples were collected for intact PTH and brain natriuretic peptide (BNP) measurements. Serum intact PTH levels were obtained at an outpatient clinic using an Immulite intact PTH assay (Diagnostics Product Corporation, 2000, Los Angeles, California). The established normal range for this assay was 10 to 65 pg/ml.
Patients were classified into 4 groups based on New York Heart Association (NYHA) functional class. Consensus of 2 experienced clinicians blinded to each other was required for classification of functional classes. In case of disagreement, a third opinion was obtained from an expert physician. Anemia was defined as hemoglobin levels <13 g/dl in men and <12 g/dl in women in accordance with World Health Organization criteria. Hypertension was defined as blood pressure >140/90 mm Hg on >2 occasions during office measurements or during antihypertensive treatment. Diabetes mellitus was defined as fasting blood glucose ≥126 mg/dl or use of antidiabetic treatment. Hyperlipidemia was defined as serum low-density lipoprotein cholesterol >160 mg/dl or total cholesterol >240 mg/dl or triglyceride >200 mg/dl or high-density lipoprotein cholesterol <40 mg/dl or use of lipid-lowering drugs. Coronary artery disease was recorded as present if there was a clinical history of coronary artery disease, abnormal stress test results with evidence of ischemia, or documented coronary stenosis >50%. Those who continued smoking during the index admission were considered current smokers. Rhythm, medications, and hemodynamic findings such as heart rate and systolic and diastolic blood pressures were evaluated.
According to protocol, all participating centers were advised to perform transthoracic echocardiography at admission. Echocardiographic examinations were performed with the Vivid 7 system (GE Healthcare, Wauwatosa, Wisconsin) with 2.5- to 5-MHz probes in all participating centers. LVEF was calculated by the modified Simpson method. Chamber sizes were defined according to recent guidelines. Systolic pulmonary artery pressure was estimated from the tricuspid regurgitant velocity profile using the modified Bernoulli equation. Digital records of transthoracic echocardiographic examinations without recorded identities were sent to the main center and evaluated offline by an expert sonographer blinded to the study plan. The study was performed in accordance with the Declaration of Helsinki for human research and was approved by the institutional review board.
Parametric data were expressed as mean ± SD and categorical data as percentages. SPSS 16.0 (SPSS, Inc., Chicago, Illinois) was used to perform statistical procedures. Receiver operator characteristic curve analysis was performed to identify the optimal cut-off point of PTH (at which sensitivity and specificity would be maximal) for the prediction of advanced HF. Areas under the curve were calculated as measurements of the accuracy of the tests. We compared areas under the curve using the Z test. Comparisons between groups were performed using 1-way analysis of variance and Kruskal–Wallis tests for normally and abnormally distributed data, respectively. Categorical variables between groups were analyzed using chi-square test. Correlation was evaluated by the Pearson correlation test or Spearman correlation test. We used univariate analysis to quantify the association of variables with advanced HF. Variables found to be statistically significant in univariate analysis were used in a multivariate logistic regression model with forward stepwise method to determine the independent predictors of advanced HF. A p value of 0.05 was considered statistically significant.
Results
Considering the entire cohort, mean age of patients was 66 ± 10 years (69% men, 31% women). Mean LVEF was 27 ± 9% and mean PTH level was 101 ± 63 pg/ml. Advanced HF (NYHA functional class IV) was observed in 30 patients (20%).
A comparison of the 4 groups of patients with HF is presented in Table 1 . Body mass index, disease duration, PTH, BNP, creatinine clearance, hemoglobin levels, diuretic usage, LVEF, LV diastolic diameter, and left atrial size differed significantly in relation to NYHA functional class ( Table 1 ). Mean levels of PTH increased as NYHA functional class increased ( Figure 1 , Table 1 ).
| Variable | NYHA Class | p Value | |||
|---|---|---|---|---|---|
| I | II | III | IV | ||
| (n = 34) | (n = 41) | (n = 45) | (n = 30) | ||
| Age (years) | 62 ± 11 | 67 ± 8 | 67 ± 11 | 68 ± 8 | 0.091 |
| Women | 26 (76%) | 24 (58%) | 32 (71%) | 22 (73%) | 0.340 |
| Body mass index (kg/m 2 ) | 28 ± 4 | 26 ± 3 | 26 ± 3 | 22 ± 4 | 0.001 |
| Hypertension | 15 (47%) | 28 (70%) | 22 (52%) | 13 (43%) | 0.102 |
| Diabetes mellitus | 8 (25%) | 12 (30%) | 16 (38%) | 7 (23%) | 0.507 |
| Coronary artery disease | 21 (64%) | 22 (54%) | 30 (71%) | 20 (67%) | 0.394 |
| Smoker | 9 (28%) | 18 (45%) | 20 (47%) | 14 (47%) | 0.324 |
| Hyperlipidemia | 9 (28%) | 12 (30%) | 8 (19%) | 6 (20%) | 0.595 |
| Disease duration (months) | 12 ± 15 | 19 ± 13 | 24 ± 26 | 34 ± 32 | 0.003 |
| Heart rate (beats/min) | 78 ± 11 | 85 ± 18 | 88 ± 22 | 94 ± 25 | 0.036 |
| Systolic blood pressure (mm Hg) | 122 ± 16 | 124 ± 17 | 120 ± 30 | 109 ± 16 | 0.033 |
| Diastolic blood pressure (mm Hg) | 77 ± 8 | 74 ± 11 | 74 ± 13 | 63 ± 18 | <0.001 |
| Atrial fibrillation | 1 (3%) | 12 (32%) | 11 (32%) | 14 (48%) | 0.002 |
| Left ventricular ejection fraction (%) | 36 ± 5 | 27 ± 7 | 23 ± 7 | 22 ± 8 | <0.001 |
| Left ventricular diastolic diameter (mm) | 5.4 ± 0.9 | 5.9 ± 0.9 | 6.0 ± 0.6 | 6.4 ± 0.7 | <0.001 |
| Left atrial size (mm) | 4.1 ± 0.3 | 4.6 ± 0.4 | 4.9 ± 0.4 | 5.2 ± 0.5 | <0.001 |
| Systolic pulmonary artery pressure (mm Hg) | 35 ± 13 | 50 ± 19 | 47 ± 13 | 44 ± 9 | 0.097 |
| Parathyroid hormone (pg/ml) | 43 ± 19 | 84 ± 56 | 121 ± 47 | 161 ± 60 | <0.001 |
| Brain natriuretic peptide (pg/ml) | 322 ± 253 | 1,177 ± 1205 | 1,535 ± 1,143 | 2,617 ± 2113 | <0.001 |
| Creatinine clearance (ml/min) | 80 ± 13 | 75 ± 13 | 77 ± 11 | 65 ± 13 | 0.003 |
| Hemoglobin (g/dl) | 13.7 ± 1.7 | 12.7 ± 1.1 | 13.3 ± 1.8 | 12.5 ± 1.7 | 0.011 |
| Presence of anemia | 7 (21%) | 13 (32%) | 17 (39%) | 15 (50%) | 0.092 |
| Antiplatelet agents | 22 (65%) | 27 (66%) | 33 (73%) | 22 (73%) | 0.767 |
| β Blockers | 26 (76%) | 28 (68%) | 30 (66%) | 19 (63%) | 0.695 |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 26 (76%) | 29 (71%) | 28 (62%) | 17 (57%) | 0.317 |
| Statins | 7 (21%) | 12 (29%) | 12 (27%) | 9 (30%) | 0.812 |
| Diuretics | 20 (59%) | 29 (70%) | 39 (87%) | 27 (90%) | 0.006 |
In patients with HF, serum intact PTH levels were correlated with BNP level, LVEF, heart rate, creatinine clearance, left atrial size, LV diastolic diameter, diuretic usage, presence of atrial fibrillation, and hemoglobin level ( Table 2 ).
| R | p Value | |
|---|---|---|
| Brain natriuretic peptide | 0.657 | <0.001 |
| Left ventricular ejection fraction | −0.421 | <0.001 |
| Heart rate | 0.431 | <0.001 |
| Creatinine clearance | −0.381 | <0.001 |
| Left atrial size | 0.381 | <0.001 |
| Diuretic usage | 0.268 | 0.001 |
| Atrial fibrillation | 0.254 | 0.003 |
| Left ventricular diastolic diameter | 0.231 | 0.005 |
| Hemoglobin | -0.175 | 0.041 |
Univariate and multivariate logistic regression analyses for identifying advanced HF are presented in Table 3 . Disease duration, body mass index, PTH, BNP and hemoglobin levels, creatinine clearance, heart rate, systolic blood pressure, LVEF, LV diastolic diameter, left atrial size, presence of atrial fibrillation, and diuretic usage were found to designate advanced HF. In multivariate logistic regression analysis, PTH level and body mass index were associated with advanced HF ( Table 3 ).
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Body mass index | 0.695 | 0.569–0.848 | <0.001 | 0.542 | 0.273–1.075 | 0.079 |
| Disease duration | 1.015 | 1.004–1.026 | 0.010 | |||
| Parathyroid hormone | 1.010 | 1.006–1.015 | <0.001 | 1.032 | 1.003–1.062 | 0.030 |
| Brain natriuretic peptide | 1.000 | 1.000–1.001 | 0.001 | |||
| Creatinine clearance | 0.935 | 0.893–0.978 | 0.004 | |||
| Hemoglobin | 0.757 | 0.567–1.011 | 0.059 | |||
| Heart rate | 1.028 | 1.010–1.046 | 0.003 | |||
| Systolic blood pressure | 0.971 | 0.951–0.990 | 0.004 | |||
| Left ventricular ejection fraction | 0.933 | 0.890–0.978 | 0.004 | |||
| Left ventricular diastolic diameter | 1.528 | 1.038–2.250 | 0.032 | |||
| Left atrial size | 2.670 | 1.299–5.489 | 0.008 | |||
| Atrial fibrillation | 3.344 | 1.419–7.883 | 0.006 | |||
| Diuretic usage | 3.273 | 0.929–11.533 | 0.065 | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


