Previous reports have shown that female gender is associated with impaired outcomes among patients with ST-segment elevation myocardial infarction (STEMI) treated by thrombolysis, mainly owing to a worst risk profile (more diabetes, more advanced age, and higher Killip class at presentation) compared to men. Still contrasting are data on the effect of gender on the outcome in patients with STEMI undergoing primary angioplasty. In particular, it is still unclear whether a larger infarct size might contribute to the explanation of the worse outcome in women. Therefore, the aim of the present study was to investigate gender-related differences in infarct size as evaluated by myocardial scintigraphy in a large cohort of patients with STEMI undergoing primary percutaneous coronary intervention. We included 830 patients with STEMI undergoing primary percutaneous coronary intervention. The infarct size was evaluated at 30 days using technetium-99m-sestamibi. A logistic regression analysis was performed to determine the relation between gender and infarct size (as percentage of patients above the median) after correction for baseline confounding factors. We also evaluated the presence of a potential age–gender interaction. A total of 183 patients (20.8%) were women. Female gender was associated with more advanced age and a greater prevalence of hypertension; previous infarction and smoking were more frequently observed in men. Female gender was associated with a smaller infarct size (p <0.001) that was confirmed after correction for baseline confounding factors (adjusted odds ratio 0.48, 95% confidence interval 0.33–0.7, p <0.001). No age–gender interaction was observed (p = 0.13). In conclusion, the results of the present study have shown that despite the presence of high-risk features at presentation, female gender was associated with a smaller infarct size than that in men, without any interaction between age and gender.
The treatment of ST-segment elevation myocardial infarction (STEMI) has greatly improved in the past decades, mainly because of the greater availability of pharmacologic and mechanical reperfusion therapies. Previous reports have shown that among patients with STEMI treated by thrombolysis, female gender was associated with impaired outcomes, mainly owing to the worst risk profile (more diabetes, more advanced age, and higher Killip class at presentation) compared to men. Still contrasting are data on the effect of gender on outcome in patients with STEMI undergoing primary angioplasty. In particular, is still unclear whether a larger infarct size might contribute to the explanation of the worse outcome observed in women. Therefore, the aim of the present study was to investigate the gender-related differences in infarct size as evaluated by myocardial scintigraphy in a large cohort of patients with STEMI undergoing primary percutaneous coronary intervention (PCI).
Methods
Our initial population included 894 patients with STEMI treated by primary angioplasty scheduled to undergo evaluation of the infarct size at 30 days after the intervention. A total of 64 patients (16 women [8.7%] and 48 men [7.4%]) were excluded because of death (n = 16), reinfarction (n = 7) or target vessel revascularization (n = 11) within 30 days from revascularization, or refusal to undergo scintigraphy (n = 30). Therefore, our final population was 830 patients.
All 830 patients were admitted within 12 hours from symptom onset and received aspirin (500 mg intravenously) and heparin (60 IU/kg intravenously). The decision to provide glycoprotein IIb/IIIa inhibitors was left to the discretion of the operator. All patients received dual oral antiplatelet therapy (aspirin and clopidogrel or ticlopidine) for ≥4 weeks after stent implantation.
Selective coronary angiography was performed in multiple projections before mechanical reperfusion. Immediately after diagnostic angiography, PCI with stenting of the infarct-related vessel was performed using standard material. Successful primary PCI was defined as Thrombolysis In Myocardial Infarction grade 3 coronary flow in the treated vessel with residual stenosis of <20%.
As previously described, gated, single photon emission computed tomographic acquisition began 60 minutes after technetium-99m-sestamibi injection (740 MBq), using a double-head γ-camera equipped with high-resolution collimators, 180° rotation arc, 32 projections, 60 s/projection, 8 frames/heart cycle, and 64 × 64 matrices. The studies were reconstructed using filtered back projection without attenuation or scatter correction and realigned along the heart axis. Perfusion defects were quantified as the percentage of the left ventricular wall, with the defect threshold set at 60% of the peak uptake.
Statistical analysis was performed using the SPSS, version 15.0, statistical package (SPSS, Chicago, Illinois). Continuous data are expressed as medians and 25th to 75th percentiles. The analysis of variance test or Mann-Whitney U test was appropriately used for continuous variables, according to the normality of distribution, as evaluated by the Shapiro-Wilk test. The chi-square test or Fisher’s exact test was used for categorical variables. Multiple logistic regression analysis was used to evaluate the effect of gender on infarct size (as percentage of patients above the median) after adjustment for significant (p <0.05) confounding baseline characteristics. Interaction between age and gender on infarct size was evaluated by analyzing the categorical by continuous variable interactions, as previously described.
Results
Of the 830 patients, 183 were women (20.8%). The patient characteristics stratified by gender are listed in Table 1 . Female gender was associated with a more advanced age (median 72 years, 25th to 75th percentile 63 to 80, vs 62 years, 25th to 75th percentile 54 to 70; p <0.001) and a greater incidence of hypertension (60.1% vs 39.3%, p <0.001) but less often with smoking (32.4% vs 52.5%, p <0.001) and previous myocardial infarction (1.2% vs 4.9%, p = 0.03).
| Variable | Men (n = 657) | Women (n = 173) | p Value |
|---|---|---|---|
| Demographic and clinical characteristics | |||
| Age (yrs) | <0.0001 | ||
| Median | 62 | 72 | |
| 25th to 75th Percentile | 54–70 | 63–80 | |
| Family history of coronary artery disease | 4.0% | 3.5% | 0.57 |
| Smoking | 52.5% | 32.4% | <0.0001 |
| Dyslipidemia | 34.1% | 33.5% | 0.89 |
| Arterial hypertension | 39.3% | 60.1% | <0.0001 |
| Diabetes mellitus | 12.2% | 20.2% | 0.48 |
| Previous myocardial infarction | 4.9% | 1.2% | 0.03 |
| Previous bypass surgery | 0.9% | 0.6% | 0.67 |
| Previous coronary angioplasty | 4.1% | 1.7% | 0.14 |
| Preinfarction angina (<24 h) | 9.8% | 15.7% | 0.12 |
| Cardiogenic shock | 3.5% | 5.8% | 0.17 |
| Interval to treatment (min) | 0.22 | ||
| Median | 200 | 210 | |
| 25th to 75th Percentile | 140–270 | 155–290 | |
| Angiographic and procedural characteristics | |||
| Collateral circulation (Rentrop class) | 0.47 | ||
| 0 | 88.7% | 91.0% | |
| 1 | 7.4% | 6.7% | |
| 2 | 3.7% | 1.1% | |
| 3 | 0.3% | 1.1% | |
| Chronic occlusion | 6.4% | 5.6% | 0.78 |
| Multivessel disease | 40.3% | 44.2% | 0.36 |
| Infarct-related artery | 0.12 | ||
| Left main | 0.2% | 0% | |
| Left anterior descending artery | 40.2% | 39.9% | |
| Circumflex branch | 15.8% | 8.7% | |
| Right coronary artery | 43.7% | 51.4% | |
| Saphenous venous graft | 0.2% | 0% | |
| Preprocedural Thrombolysis In Myocardial Infarction flow | 0.65 | ||
| 0-1 | 80.9% | 82.6% | |
| 2 | 10.6% | 11% | |
| 3 | 8.6% | 6.4% | |
| Abciximab administration | 89.2% | 93.1% | 0.13 |
| Stent implantation | 98.4% | 100% | 0.77 |
| Intra-aortic balloon pump | 3.3% | 5.2% | 0.25 |
| Postprocedural Thrombolysis In Myocardial Infarction 3 flow | 93% | 89.5% | 0.13 |
No difference was observed in terms of the extension of coronary artery disease, preprocedural Thrombolysis In Myocardial Infarction flow, procedural features such as coronary stent implantation, abciximab administration, or postprocedural Thrombolysis In Myocardial Infarction 3 flow.
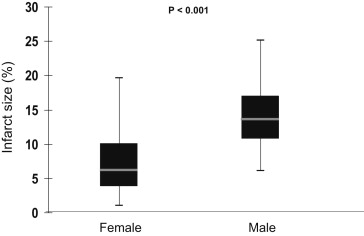
As shown in Figure 1 , female gender was associated with a smaller infarct size (median 6.9%, 25th to 75th percentile 1% to 19.6%, vs 13.9%, 25th to 75th percentile 6.1% to 25.1%, p <0.001), confirmed by the analysis of the peak creatine kinase-MB mass (median 151 ng/ml, 25th to 75th percentile 67 to 225, vs 212 ng/ml, 25th to 75th percentile 116 to 403; p <0.001).
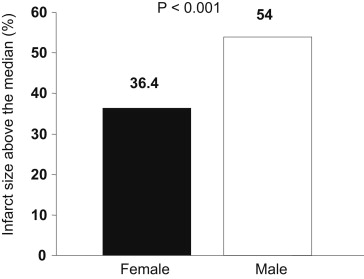
The results were confirmed when the analysis was performed using the percentage of patients with an infarct size above the median (36.4% vs 54%, odds ratio 0.48, 95% confidence interval 0.35 to 0.69, p <0.001; Figure 2 ), even after correction for baseline confounding factors on multivariate analysis (adjusted odds ratio 0.48, 95% confidence interval 0.33 to 0.7, p <0.001).
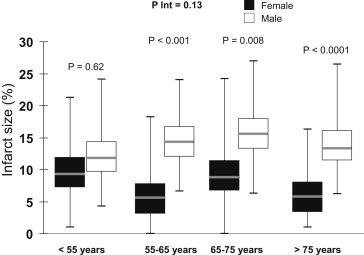
Furthermore, we specifically investigated the potential age–gender interaction on infarct size. As shown in Figure 3 , female gender was associated with a smaller infarct size in all age categories, especially after 55 years (<55 years, 9.6%, 25th to 75th percentile 1% to 21.3%, vs 12%, 25th to 75th percentile 4.3% to 24.1%, p = 0.62; 55 to 65 years, 5.5%, 25th to 75th percentile 0% to 18.2% vs 14.4%, 25th to 75th percentile 6.5% to 23.9%, p <0.001; 65 to 75 years, 9.1%, interquartile range 0% to 24.2%, vs 15.6%, 25th to 75th percentile 6.3% to 27%, p = 0.008; >75 years, 5.7%, 25th to 75th percentile 1% to 16.3%, vs 13.8%, 25th to 75th percentile 6.1% to 26.6%, p <0.001), without any significant interaction (p interaction = 0.13).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


