Certain patients with type 2 diabetes mellitus (DM) do not have increased cardiovascular (CV) risk. The aim of the present study was to stratify hypertensive adults with DM into those with low or high CV risk according to the absence or presence of coronary artery calcium (CAC). The study group included 423 patients, a subgroup of the 544 participants in the calcification side arm of the International Nifedipine Study: Intervention as Goal for Hypertension Therapy. All underwent a baseline computed tomography scan with an unenhanced dual-detector spiral computed tomography scan for CAC measurements. All were free of CV disease and completed 3 years (short-term) of follow-up. A total of 268 patients were included in the 15-year (long-term) follow-up period. The study group was divided into 4 subgroups according to the presence or absence of DM and CAC and was analyzed for a first CV event. Of the 423 patients, 164 (39%) had DM. Cardiovascular events occurred in 41 patients during the first 3 years and in 111 of 268 patients during the long-term follow-up. The rate of CV events was greater in the patients with DM with CAC than in those without (15% vs 7% after 3 years and 52% vs 32% after 15 years). Compared to those without DM without CAC, the short-term adjusted hazard ratio for CV event in those with DM with and without CAC was 6.6 (95% confidence interval 1.4 to 30.5) and 3.9 (95% confidence interval 0.7 to 22.6), respectively. A similar trend was seen in the long-term follow-up study. In conclusion, patients with hypertension and DM can be stratified into a lower CV risk in the absence of CAC.
Coronary artery calcium (CAC) as measured using computed tomography (CT) is well accepted as a reliable marker of the total burden of coronary atherosclerosis. The presence of CAC among the asymptomatic population indicates subclinical coronary heart disease (CHD) and is associated with increased cardiovascular (CV) risk and all-cause mortality, and the absence of CAC indicates a more favorable prognosis. This has also been shown in high-risk patients such as those with hypertension, smokers, patients with chronic renal failure, and those with diabetes mellitus (DM). Recently, the concept that type 2 DM is a CHD equivalent has been challenged by several investigators, who demonstrated that not all patients with DM bear an increased CV risk. The present study was designed to evaluate whether CAC measurement can identify patients with hypertension and DM who have a relatively low CV risk. For this purpose, we analyzed the CV outcomes according to the absence or presence of CAC in subgroups of the participants in the calcification side arm of the International Nifedipine GITS [Gastrointestinal Therapeutic System] Study: Intervention as Goal for Hypertension Therapy (INSIGHT) during short- and long-term follow-up.
Methods
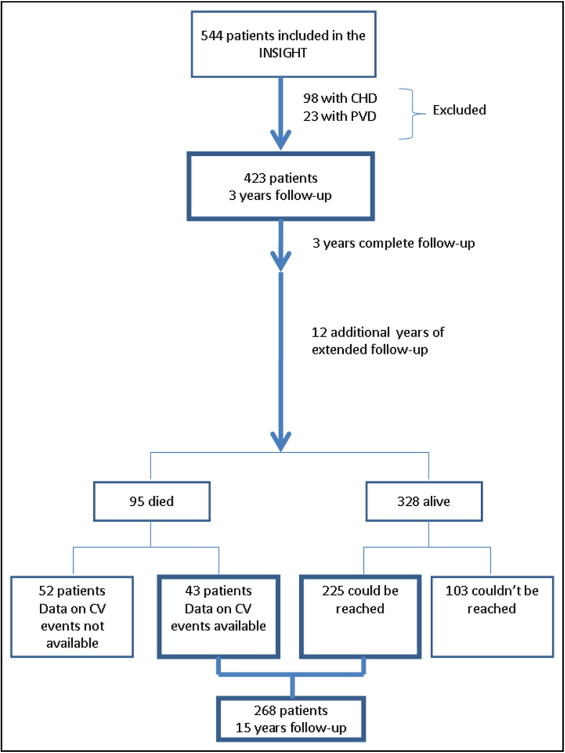
The study group was a subgroup of 544 high-risk hypertensive patients who enrolled in 1995 to the calcification side arm study of the INSIGHT that aimed to compare the effect of the calcium antagonist, nifedipine gastrointestinal therapeutic system, versus a diuretic on the progression of coronary calcification. A total of 98 patients with CHD and 23 with peripheral vascular disease at baseline were excluded. The remaining 423 patients, without symptoms or established CV disease, completed 3 years of the INSIGHT follow-up and constituted the short-term study group. In July 2010, we identified 95 patients who had died. During the subsequent 6 months, we interviewed the 328 survivors and were successful in reaching 225 (69%). The 15-year long-term analysis included those who were successfully interviewed (n = 225), and those who had died with evidence of a first CV event (n = 43; Figure 1 ) .
Each subject was evaluated clinically at baseline, and a detailed medical history was taken and standard physical examination performed. The following variables were recorded: age, height, weight, blood pressure, concomitant diseases, smoking habits, and laboratory test results. The estimated glomerular filtration rate was calculated according to the Chronic Kidney Disease Epidemiology Collaboration equation. Proteinuria was defined as urinary protein excretion >0.5 g/24 hours. DM was considered present when a history of DM was reported or the subject used insulin or oral hypoglycemic medications. Each patient underwent coronary computed tomography and echocardiography at baseline.
All computed tomography scans were done in a single center and analyzed by a single experienced physician. All computed tomography scans were performed using a dual-detector spiral computed tomography machine without electrocardiographic gating and without contrast injection. The scanning protocol and CAC measuring were done according to a previously published protocol using the modified Agatston method. The total CAC score was the sum of all the individual calcific lesions identified within the area of the coronary arteries. The reproducibility of calcification scoring using this method is high, with an intraclass correlation coefficient of 0.99 and interobserver agreement of 0.94. A total CAC score >0 was considered positive for the presence of CAC.
Echocardiographic studies were performed with the patient at rest, at steady state, and in the left lateral position, using commercially available Hewlett-Packard 1000 or newer systems with 2.5-MHz transducers, as previously described. The left ventricular mass was calculated using the corrected American Society of Echocardiography formula described by Devereux et al. The left ventricular mass index was calculated by dividing the left ventricular mass by the body surface area. Left ventricular hypertrophy was diagnosed when the intraventricular septum and/or posterior wall thickness were ≥12 mm or when the left ventricular mass index was >110 g/m 2 in women or >134 g/m 2 in men.
Events were recorded from the source documents during the first 3 years as a part of the main INSIGHT study and by telephone interview for the extended long-term follow-up period at the end of 15 years. Data on mortality and the cause of death through July 2010 were available for all participants and derived from the registry of the Ministry of Internal Affairs. Only the first CV event was counted. Death from CV cause included sudden death, death from coronary heart disease, congestive heart failure and cerebrovascular disease. The CV events included acute myocardial infarction, hospitalization for unstable angina or coronary catheterization that resulted in angioplasty or coronary artery bypass surgery, and stroke or transient ischemic attack.
The institutional Helsinki committee approved the entire study.
The data were analyzed using SPSS software, version 19.0 (SPSS, Chicago, Illinois). The significance level was set at p = 0.05.
The chi-square test was used to compare the 4 study groups, defined according the presence or absence of CAC and the presence or absence of DM. Independent t tests and 1-way analysis of variance were performed to compare the patients with and without CV events for the continuous variables. The length of follow-up was calculated as interval from the baseline computed tomography scan to a CV event, CV death, or the end of follow-up. Hazard ratios (HRs) and 95% confidence intervals (CIs) for the incidence of CV events were estimated using the Cox proportional hazard models, adjusting for potential confounders according to an association with a CV event on univariate analysis or the findings of significant associations in previous studies. For the present study, with follow-up periods of 3 and 15 years and ≥30 patients in each subgroup, we had a power of 90% to compare a HR of 1.0 to 2.5 (significance level of 5%). The goodness of fit of the model was evaluated using the C index. The C index is a probability of concordance between predicted and observed survival with C = 0.5 for random predictions and C = 1 for a perfect discriminating model. The C index is relatively unaffected by the amount of censoring. The log-rank test was calculated to compare the survival curves across the 4 groups, adjusting for age and gender.
Results
A total of 423 patients with hypertension (mean age 64 ± 5 years, 48% men) were included in the present study. The baseline characteristics stratified by the presence or absence of DM are presented in Table 1 . The patients with DM had a higher body mass index, higher systolic and lower diastolic blood pressure, higher frequency of proteinuria, higher triglyceride levels and lower total low-density lipoprotein and high-density lipoprotein cholesterol, and were less likely to be smokers than the patients without DM. Long-term information was available for 268 patients, with a mean age of 64 ± 6 years. These patients had baseline characteristics similar to those of the entire 423 patients and included 142 men (53%), 96 with DM (36%), and 173 with detectable CAC (65%).
| Variable | DM | p Value | |
|---|---|---|---|
| Yes (n = 164) | No (n = 259) | ||
| Age (years) | 64 ± 6 | 65 ± 6 | 0.340 |
| Men | 85 (52%) | 117 (45%) | 0.182 |
| Body mass index (kg/m 2 ) | 29.9 ± 4.9 | 28.5 ± 4.1 | 0.003 |
| Systolic blood pressure (mm Hg) | 168 ± 15 | 165 ± 16 | 0.029 |
| Diastolic blood pressure (mm Hg) | 92 ± 9 | 94 ± 8 | 0.005 |
| Heart rate (beats/min) | 74 ± 9.0 | 73 ± 9.5 | 0.138 |
| Duration of hypertension (years) | 12.2 ± 8.6 | 11.0 ± 8.7 | 0.194 |
| Smokers | 15 (9%) | 63 (24%) | <0.001 |
| Left ventricular hypertrophy (per echocardiography) | 107 (65%) | 155 (60%) | 0.265 |
| Estimated glomerular filtration rate (ml/min) | 70.5 ± 17.1 | 71.0 ± 15.5 | 0.830 |
| Proteinuria | 25 (15%) | 15 (6%) | 0.001 |
| Creatinine (mg/dl) | 1.037 ± 0.30 | 1.002 ± 0.23 | 0.199 |
| Serum glucose (mg/dl) | 164 ± 46 | 96 ± 12 | <0.001 |
| Total cholesterol (mg/dl) | 226 ± 38 | 243 ± 46 | <0.001 |
| High-density lipoprotein cholesterol (mg/dl) | 42 ± 14 | 47 ± 13 | 0.009 |
| Low-density lipoprotein cholesterol (mg/dl) | 151 ± 35 | 164 ± 40 | 0.004 |
| Triglycerides (mg/dl) | 192 ± 105 | 160 ± 83 | 0.001 |
| Total calcium score (score) | 137 ± 334 | 148 ± 486 | 0.793 |
The frequency of CAC (total CAC score >0) was similar in the DM (65%) and non-DM population (64%). Patients with CAC were older and were more likely to be men than those without CAC ( Table 2 ). The patients with DM and CAC had the highest levels of creatinine and triglycerides, a greater rate of proteinuria, and the lowest diastolic blood pressure and cholesterol levels ( Table 2 ). The total CAC score was similar in those with and without DM, with a CAC score of 210 ± 395 and 233 ± 593, respectively.
| Variable | DM | p Value | |||
|---|---|---|---|---|---|
| Yes (n = 164) | No (n = 259) | ||||
| CAC | CAC | ||||
| Yes (n = 107) | No (n = 57) | Yes (n = 165) | No (n = 94) | ||
| Age (years) | 65 ± 6 | 62 ± 5 | 66 ± 6 | 63 ± 6 | <0.001 |
| Men | 66 (62%) | 19 (33%) | 86 (52%) | 31 (33%) | <0.001 |
| Body mass index (kg/hour ) | 30 ± 5 | 31 ± 5 | 28 ± 4 | 29 ± 4 | 0.006 |
| Systolic blood pressure (mm Hg) | 169 ± 14 | 168 ± 18 | 165 ± 17 | 165 ± 15 | 0.185 |
| Diastolic blood pressure (mm Hg) | 91 ± 9 | 92 ± 9 | 94 ± 8 | 95 ± 9 | 0.021 |
| Heart rate (beats/min) | 74 ± 9 | 74 ± 9 | 73 ± 9.3 | 72 ± 10 | 0.351 |
| Duration of hypertension (years) | 12 ± 8 | 13 ± 9 | 12 ± 9 | 10 ± 8 | 0.204 |
| Smokers | 11 (10%) | 4 (7%) | 37 (22%) | 26 (28%) | 0.001 |
| Left ventricular hypertrophy (per echocardiography) | 75 (70%) | 32 (56%) | 103 (62%) | 52 (55%) | 0.133 |
| Estimated glomerular filtration rate (ml/min) | 68 ± 18 | 75 ± 14 | 72 ± 16 | 69 ± 15 | 0.072 |
| Proteinuria | 21 (20%) | 4 (7%) | 11 (7%) | 4 (4%) | <0.001 |
| Creatinine (mg/dl) | 1.100 ± 0.34 | 0.92 ± 0.17 | 1.001 ± 0.22 | 1.004 ± 0.20 | <0.001 |
| Serum glucose (mg/dl) | 163 ± 47 | 167 ± 45 | 96 ± 12 | 97 ± 12 | <0.001 |
| Total cholesterol (mg/dl) | 223 ± 39 | 231 ± 37 | 242 ± 47 | 243 ± 44 | 0.001 |
| High-density lipoprotein cholesterol (mg/dl) | 41 ± 14 | 45 ± 13 | 46 ± 13 | 47 ± 13 | 0.035 |
| Low-density lipoprotein cholesterol (mg/dl) | 148 ± 37 | 156 ± 30 | 164 ± 39 | 162 ± 41 | 0.020 |
| Triglycerides (mg/dl) | 206 ± 118 | 165 ± 65 | 155 ± 87 | 169 ± 76 | <0.001 |
During the short-term follow-up period, 41 patients had a first CV event; 2 experienced CV death, 13 experienced acute myocardial infarction, 13 experienced unstable angina resulting in revascularization, and 13 experienced stroke/transient ischemic attack. Of these events, 21 occurred in those without DM (8.1%) and 20 in those with DM (12.2%; p = 0.014). The incidence of CV events was significantly greater among the patients with CAC than among those without CAC ( Table 3 ). The rate of CV events was twofold greater in those with DM and CAC than in those with DM without CAC. Compared to those without DM and without CAC, the HR for CV events was 8.1 (95% CI 1.8 to 36.1) for those with DM and CAC and 3.5 (95% CI 0.6 to 19.6) for those with DM without CAC. The same pattern remained after adjustment for age, gender, proteinuria, left ventricular hypertrophy, and estimated glomerular filtration rate ( Table 3 ). The C index was 0.744, demonstrating a relatively good fit of the model to predict CV events.
| Variable | DM | |||||||
|---|---|---|---|---|---|---|---|---|
| 3-yr Follow-Up | 15-yr Follow-Up | |||||||
| Yes (n = 164) | No (n = 259) | Yes (n = 96) | No (n = 172) | |||||
| CAC | CAC | CAC | CAC | |||||
| Yes (n = 107) | No (n = 57) | Yes (n = 165) | No (n = 94) | Yes (n = 62) | No (n = 34) | Yes (n = 111) | No (n = 61) | |
| Event rate | 16 (15%) | 4 (7%) | 19 (12%) | 2 (2%) | 32 (52%) | 11 (32%) | 55 (50%) | 13 (21%) |
| Unadjusted HR | 8.1 (1.8–36.1) | 3.5 (0.6–19.6) | 6.0 (1.4–26.3) | 1.0 | 3.2 (1.6–6.0) | 1.9 (0.8–4.1) | 2.7 (1.5–5.0) | 1.0 |
| Age and gender adjusted | 6.9 (1.5–31.4) | 3.5 (0.6–19.6) | 5.4 (1.2–23.9) | 1.0 | 2.6 (1.4–5.1) | 1.7 (0.7–3.8) | 2.2 (1.2–4.2) | 1.0 |
| Multivariate ⁎ adjusted | 6.6 (1.4–30.5) | 3.9 (0.7–22.6) | 5.8 (1.3–25.9) | 1.0 | 2.6 (1.3–5.1) | 1.7 (0.7–3.8) | 2.4 (1.3–4.6) | 1.0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


