There is controversy regarding type of bundle branch block (BBB) that is associated with increased mortality risk in patients with heart failure (HF). The present study was designed to explore the association between BBB pattern and long-term mortality in hospitalized patients with systolic HF. Risk of 4-year all-cause mortality was assessed in 1,888 hospitalized patients with systolic HF (left ventricular ejection function <50%) without a pacemaker in a prospective national survey. Cox proportional hazards regression modeling was used to compare mortality risk in patients with right BBB (RBBB; 10%), left BBB (LBBB; 14%), and no BBB (76%) on admission electrocardiogram. At 4 years of follow up, mortality rates were highest in patients with RBBB (69%), intermediate in those with LBBB (63%), and lowest in those without BBB (50%, p <0.001). Multivariate analysis demonstrated a significant 36% increased mortality risk in patients with RBBB versus no BBB (p = 0.002) but no significant difference in mortality risk for patients with LBBB versus no BBB (hazard ratio 1.04, p = 0.66). RBBB versus LBBB was associated with a 29% (p = 0.035) increased risk for 4-year mortality in the total population and with a 58% (p = 0.015) increased risk in patients with ejection fraction <30%. In conclusion, RBBB but not LBBB on admission electrocardiogram is associated with a significant increased long-term mortality risk in hospitalized patients with systolic HF. Deleterious effects of RBBB compared to LBBB appear to be more pronounced in patients with more advanced left ventricular dysfunction.
Prolongation of QRS interval (≥120 ms) in patients with heart failure (HF) is common (14% to 47%) and is associated with higher all-cause mortality, cardiovascular death, or hospitalization for HF compared to patients with HF and normal QRS interval. There is controversy regarding type of bundle branch block (BBB) that is associated with poorer outcome in patients with HF, with most studies showing that left BBB (LBBB) is an independent prognostic marker, whereas right BBB (RBBB) is a weaker marker or not associated with worse prognosis. Conversely, we previously showed in hospitalized patients with HF that RBBB, but not LBBB, is associated with increased 1-year mortality risk, an association that was stronger for patients with systolic HF, particularly for patients with severe left ventricular (LV) dysfunction. However, currently there are limited data regarding the effect of BBB pattern on long-term mortality in patients with LV dysfunction. Accordingly, the present study aimed to investigate the association between QRS morphology and long-term mortality in 1,888 patients hospitalized with systolic HF who were prospectively followed-up over an extended 4-year period.
Methods
Baseline and admission characteristics of patients were extracted from the Heart Failure Survey in Israel (HFSIS; 2003) database. Design and methods of the HFSIS registry have been described previously. Briefly, the survey, conducted in March and April 2003, included 4,102 patients admitted with a diagnosis of HF. Criteria used for diagnosis of HF were symptoms of HF (at rest or during exercise) and objective evidence of cardiac dysfunction at rest. There were 3 subgroups of diagnoses for hospitalized patients: (1) acute de novo HF, (2) worsening of chronic HF, and (3) chronic stable HF with hospitalization unrelated to HF exacerbation. There were 2,090 patients with HF and LV ejection fraction (LVEF) <50% as demonstrated by echocardiography. We excluded from the study 188 patients who had a permanent pacemaker including a biventricular pacemaker and 14 patients who lacked electrocardiographic data. Thus, the final analysis included 1,888 patients. The end point of the study was all-cause mortality, which was assessed for all patients by matching their identification numbers with the Israeli National Population Registry. Mortality data were obtained for all study patients at a 4-year period from hospitalization, providing an extended follow-up to the previously reported 1-year outcome study. LBBB was defined as QRS duration ≥120 ms, upright complexes with notched R waves in leads I, V 5 , and V 6 , and QS or rS pattern in lead V 1 . RBBB was defined as QRS duration ≥120 ms, a monophasic R wave in lead V 1 or rSR in leads V 1 and V 2 , and deep slurred S waves in leads I, V 5 , and V 6 . LVEF classes determined by echocardiography with visual assessment were classified as normal (≥50%), mildly impaired (40% to 49%), moderately impaired (30% to 39%), and severely impaired (<30%). Median and interquartile range timing of echocardiography were 0 month and 0 month to 6 months.
Characteristics of patients categorized by BBB type were compared by nonparametric Kruskal-Wallis test or chi-square test. Cumulative probability of survival by BBB type was graphically displayed according to the Kaplan-Meier method with comparison by log-rank test. To examine the relation between RBBB, LBBB, and no BBB and mortality, several models were applied. First, potential variables (identified in previous published studies as risk factors for mortality or clinical variables that were associated with mortality) were evaluated by univariate analysis and selected based on clinical and statistical significance. Second, multivariate analysis was carried out using Cox proportional hazards regression modeling adjusted for age (continuous), gender, New York Association (NYHA) functional classes III to IV versus I to II, previous myocardial infarction, atrial fibrillation, previous stroke, diabetes, chronic obstructive pulmonary disease, cirrhosis, malignant tumor, LVEF class, admission creatinine levels (continuous), systolic blood pressure <115 versus ≥115 mm Hg, sodium <136 versus ≥136 mEq/L, hemoglobin <10 versus ≥10 g/dl and long-term use of statins, β blockers, and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Analyses were conducted with SAS 9.2 (SAS Institute, Cary, North Carolina).
Results
Of the 1,888 patients with systolic HF, 306 (14%) had LBBB on admission electrocardiogram and 193 (10%) had RBBB. Table 1 presents baseline clinical characteristics of patients indicating that patients with LBBB were older than those with RBBB or no BBB. Prevalence of NYHA functional classes III to IV and low EF was highest in LBBB, lower in RBBB, and lowest in no BBB. Long-term therapy with furosemide, spironolactone, and digoxin was more frequent in patients with LBBB compared to those with RBBB or no BBB. In the RBBB subgroup the proportion of women was smaller than in the LBBB or no-BBB subgroups. Systolic pulmonary arterial pressure data were available for 841 patients (45%). There was a trend toward a higher systolic pulmonary arterial pressure in patients with RBBB compared to those with LBBB or no BBB (mean ± SD 46 ± 14, 43 ± 15, and 43 ± 16 mm Hg, respectively, p = 0.107 for overall comparison among the 3 subgroups).
| Variable | Total (n = 1,888) | Bundle Branch Block | p Value ⁎ | ||
|---|---|---|---|---|---|
| Left (n = 306, 14%) | Right (n = 193, 10%) | None (n = 1,389, 76%) | |||
| History | |||||
| Age (years) | 73 (63–80) | 76 (68–81) | 74 (67–81) | 71 (62–79) | <0.001 |
| Women | 33% | 33% | 25% | 35% | 0.026 |
| Hypertension | 65% | 65% | 69% | 64% | 0.392 |
| Diabetes mellitus | 53% | 55% | 55% | 53% | 0.554 |
| Smoker | 35% | 31% | 38% | 36% | 0.144 |
| Coronary heart disease | 82% | 82% | 82% | 82% | 0.995 |
| New York Heart Association functional class III to IV | 40% | 51% | 45% | 35% | <0.001 |
| Previous myocardial infarction | 62% | 55% | 67% | 62% | 0.021 |
| Previous stroke | 13% | 13% | 11% | 14% | 0.563 |
| Chronic obstructive pulmonary disease | 18% | 17% | 17% | 18% | 0.855 |
| Atrial fibrillation | 25% | 29% | 28% | 24% | 0.120 |
| Acute heart failure | 61% | 60% | 57% | 61% | 0.588 |
| Left ventricular ejection fraction estimated by echocardiography (%) | |||||
| 40–49 | 30% | 15% | 20% | 35% | <0.001 |
| 30–39 | 36% | 34% | 40% | 36% | |
| <30 | 34% | 51% | 40% | 29% | |
| Admission systolic blood pressure (mm Hg) | 135 (118–157) | 135 (118–153) | 131 (116–156) | 136 (119–158) | 0.362 |
| Admission heart rate (beats/min) | 81 (70–98) | 80 (69–95) | 80 (68–92) | 82 (70–100) | 0.061 |
| Admission laboratory values | |||||
| Creatinine (mg/dl) † | 1.2 (0.9–1.6) | 1.3 (1.0–1.8) | 1.4 (1.1–1.8) | 1.2 (0.9–1.6) | 0.160 |
| Sodium (mmol/L) | 138 (136–141) | 138 (135–141) | 138 (135–141) | 139 (136–141) | 0.903 |
| Hemoglobin (g/dl) | 12.5 (11.0–13.8) | 12.6 (11.2–13.7) | 12.5 (11.3–13.8) | 12.4 (10.9–13.8) | 0.563 |
| Long-term medications | |||||
| β Blockers | 72% | 69% | 71% | 73% | 0.332 |
| Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers | 81% | 83% | 82% | 80% | 0.510 |
| Furosemide | 75% | 89% | 81% | 71% | <0.001 |
| Spironolactone | 25% | 34% | 32% | 22% | <0.001 |
| Digoxin | 17% | 28% | 23% | 14% | <0.001 |
| Statins | 53% | 52% | 43% | 55% | 0.005 |
⁎ For overall difference among the 3 subgroups.
† To convert creatinine to micromoles per liter, multiply by 88.4.
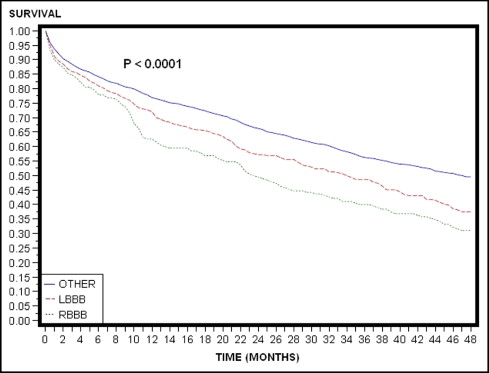
For the total study population, Kaplan-Meier survival curves ( Figure 1 ) demonstrated that during the first 8 months of follow-up mortality rates were higher in patients with RBBB and LBBB compared to those who had no BBB. After 8 months and until the end of the extended 4-year follow-up period, curves of RBBB and LBBB separated, showing graded decrements in survival in patients with RBBB, LBBB, and no BBB, respectively. Mortality rates at 4 years were 69%, 63%, and 50% in the RBBB, LBBB, and no-BBB groups, respectively (p <0.001; Figure 1 ). Consistent with these findings, multivariate analysis ( Table 2 ) showed a significant increase in mortality risk in patients with RBBB compared to those with no BBB, whereas no statistically significant difference in mortality risk was observed between patients with LBBB and those with no BBB. Comparison of the outcome between patients with RBBB and those with LBBB showed a significant 29% (p = 0.035) increase in long-term mortality risk in the former subgroup compared to the latter subgroup. Similar results were found for the 2 subgroups of acute and chronic HF. Notably, RBBB was associated with a similar magnitude of risk increase as demonstrated for other known predictors of mortality risk in this population including age, diabetes mellitus, advanced LV dysfunction, or renal dysfunction ( Table 3 ).
| Variable | Number of Patients | Crude Mortality | Hazard Ratio (95% confidence interval) | p Value |
|---|---|---|---|---|
| Left ventricular ejection fraction <50% | ||||
| All patients | 1,800 | 976 (54%) | — | — |
| Right versus no bundle branch block | 182 vs 1,322 | 124 (68%) vs 665 (50%) | 1.36 (1.12–1.65) | 0.002 |
| Left versus no bundle branch block | 296 vs 1,322 | 187 (63%) vs 665 (50%) | 1.04 (0.88–1.23) | 0.655 |
| Right versus left bundle branch block | 182 vs 296 | 124 (68%) vs 187 (63%) | 1.29 (1.02–1.64) | 0.035 |
| Left ventricular ejection fraction <30% | ||||
| All patients | 609 | 396 (65%) | — | — |
| Right versus no bundle branch block | 70 vs 389 | 54 (77%) vs 242 (62%) | 1.55 (1.14–2.11) | 0.005 |
| Left versus no bundle branch block | 150 vs 389 | 100 (67%) vs 242 (62%) | 1.03 (0.81–1.31) | 0.823 |
| Right versus left bundle branch block | 70 vs 150 | 54 (77%) vs 100 (67%) | 1.58 (1.09–2.28) | 0.015 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


