Aortic stenosis (AS) and systemic atherosclerosis have been shown to be closely related. We evaluated the prevalence of aortic arch plaques and their possible association with the risk of cerebral infarction in patients with severe AS. Transesophageal echocardiography was performed in 116 patients with severe AS (55 men, mean age 71 ± 7 years, mean aortic valve area 0.68 ± 0.15 cm 2 ) who were scheduled for aortic valve replacement. The presence, thickness, and morphology of the aortic arch plaques were evaluated using transesophageal echocardiography. Cerebral infarcts (chronic cerebral infarction and cerebral infarction after cardiac catheterization and aortic valve replacement) were assessed in all patients. Compared to age- and gender-matched control subjects, the patients with severe AS had a significantly greater prevalence of aortic arch plaques (74% vs 41%; p <0.0001) and complex arch plaques such as large plaques (≥4 mm), ulcerated plaques, or mobile plaques (30% vs 10%; p = 0.004). Multivariate logistic analyses showed that the presence of complex arch plaques was independently associated with cerebral infarction in patients with AS after adjusting for traditional atherosclerotic risk factors and coronary artery disease (odds ratio 8.46, 95% confidence interval 2.38 to 30.12; p = 0.001). In conclusion, the results from the present study showed that there is a greater prevalence of aortic arch plaques in patients with AS and that the presence of complex plaques is independently associated with cerebral infarction in these patients. Therefore, the identification of complex arch plaques using transesophageal echocardiography is important for risk stratification of cerebrovascular events in patients with severe AS.
Because aortic stenosis (AS) shares many characteristics with atherosclerotic disease such as clinical risk factors, it has been recognized as an atherosclerotic disease. A recent study, performed using transesophageal echocardiography (TEE), showed that the amount of aortic plaques gradually increases as AS progresses from mild to severe, suggesting a close relation between the severity of AS and aortic plaques in patients with AS. Additionally, case-control and prospective studies have demonstrated that the presence of aortic plaques in the aortic arch, detected using TEE, is associated with the risk of stroke. In particular, complex aortic arch plaques, such as large plaques, ulcerated plaques, or mobile plaques, contribute to an increased risk of stroke. In patients with severe AS, the presence of complex plaques in the aortic arch might be an important risk factor for cerebrovascular events. In the present study, we investigated the prevalence of aortic arch plaques using TEE in patients with severe AS, who were scheduled for aortic valve replacement (AVR). We also evaluated the potential association of the presence of complex arch plaques with the risk of cerebral infarction in these patients.
Methods
The study population consisted of 116 consecutive patients with severe AS who underwent TEE and were scheduled for AVR (55 men, mean age 71 ± 7 years, mean aortic valve area 0.68 ± 0.15 cm 2 ). The patients were ineligible if they had aortic artery disease, endocarditis, prosthetic valves, or had undergone other cardiac surgery. A total of 58 age- and gender-matched patients with primary mitral regurgitation who were referred for TEE (28 men, mean age 71 ± 7 years) served as the controls. The hospital ethics committee approved the study protocol, and all patients provided written informed consent.
For each study patient, the clinical data and history of risk factors were obtained. Diabetes mellitus was determined by the presence of an existing diagnosis, a fasting blood glucose level of >126 mg/dl, glycated hemoglobin A1c level of >5.8%, or the use of antidiabetic medications or insulin. Hypertension was defined by a systolic blood pressure of >140 mm Hg and a diastolic blood pressure of >90 mm Hg or the use of antihypertensive medications. Hypercholesterolemia was determined by a serum cholesterol value of >220 mg/dl or the use of cholesterol-lowering medications. Patients were classified as nonsmokers if they had never smoked or if they had stopped smoking for ≥1 year before the study. All other patients were classified as smokers. All patients underwent cardiac catheterization because of preoperative evaluation of coronary artery disease. Quantitative coronary angiography was conducted using the view that showed the greatest degree of stenosis. Coronary artery disease was defined as >70% diameter stenosis or a history of percutaneous coronary intervention. AVR was performed with conventional techniques of cardiopulmonary bypass using standard ascending aortic cannulation or right axillary arterial cannulation according to the surgeon’s decision. During surgery, epiaortic ultrasound scanning was performed to evaluate the ascending aorta for determination of the aortic cannulation site.
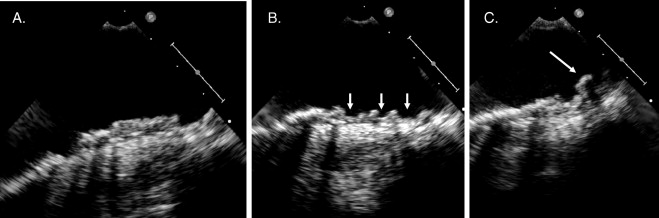
The severity of AS and cardiac function were assessed using transthoracic echocardiography. The aortic valve area was calculated using the continuity equation. The left ventricular ejection fraction was calculated using the biplane Simpson formula. TEE was performed using a multiplane transducer before AVR. The aortic arch was defined as the portion of the aorta between the curve at the end of the ascending aorta and the origin of the left subclavian artery. The plaques were defined as discrete protrusions of the intimal surface of the vessel, ≥2 mm in thickness, and different in appearance and echogenicity from the adjacent intact intimal surface. In the case of multiple plaques, the most advanced lesion was considered. An ulceration was defined as a discrete indentation of the luminal surface of the plaque with a base width and maximum depth of ≥2 mm each. Large plaques ≥4 mm in thickness, plaques with ulceration, or mobile components were defined as complex plaques ( Figure 1 ). The interpretation of echocardiographic studies was performed by an experienced echocardiographer who was unaware of the patient information.
Chronic cerebral infarction and cerebral infarction after cardiac invasive procedures were investigated. All patients underwent brain computed tomography to diagnose chronic cerebral infarction before preoperative cardiac catheterization. Chronic cerebral infarcts were identified by experienced neuroradiologists as hypodense lesions on computed tomography scans compatible with a history of clinical signs or symptoms of stroke or as those compatible with the findings of cerebral infarcts by brain magnetic resonance imaging. We excluded lacunar stroke defined clinically and by brain computed tomography or magnetic resonance imaging as the presence of a small infarct <15 mm in diameter located in the territory of small vessel disease. Furthermore, information regarding cerebral infarction after cardiac catheterization and AVR was obtained for all patients. The diagnosis of cerebral infarction after a cardiac procedure was made by experienced neurologists and required evidence of neurologic deficits, lasting for >24 hours due to ischemic lesions.
The results are expressed as the mean ± SD. When the 2 groups were compared, the unpaired t test or Mann-Whitney U test was used, as appropriate. A statistical comparison among the 3 groups was performed using 1-way analysis of variance, and post hoc multiple comparisons were conducted using Scheffe’s test. The categorical variables were compared using a chi-square test or Fisher’s exact test. Univariate logistic regression analysis was used to assess the association of clinical factors and the presence of complex arch plaques with the risk of cerebral infarction. The association of the presence of complex arch plaques with the risk of cerebral infarction was then evaluated using multivariate logistic regression analysis after adjustment for atherosclerotic risk factors (e.g., age, gender [men], hypertension, diabetes mellitus, smoker, and hypercholesterolemia) and coronary artery disease. Age was entered as a continuous variable in regression analyses. The values of p <0.05 were considered significant.
Results
Of the 116 patients with severe AS, aortic arch plaques were detected in 86 (74%) and complex arch plaques in 35 (30%; large plaques in 33 [28%], ulcerated plaques in 20 [17%], and mobile plaques in 10 [9%]) using TEE. The characteristics of the 116 patients with AS according to the presence of arch plaques and those of the controls are listed in Table 1 . No significant differences were noted between patients with AS and the controls with respect to the prevalence of hypertension, diabetes mellitus, and smoking; however, the prevalence of hypercholesterolemia (p = 0.01) and coronary artery disease (p = 0.009) was significantly greater in patients with AS than in controls ( Table 1 ). Compared to controls, the patients with AS had a significantly greater prevalence of arch plaques (74% vs 41%; p <0.0001) and complex arch plaques (30% vs 10%; p = 0.004; Figure 2 ). Among the 3 groups of patients with AS with complex, noncomplex, or no plaques, the mean age (p = 0.001) and the prevalence of coronary artery disease (p = 0.03) were significantly different, and they were greater in patients with complex arch plaques (p = 0.001 and p = 0.04, respectively; Table 1 ).
| Variable | AS (n = 116) | p Value | Controls (n = 58) | ||
|---|---|---|---|---|---|
| No Plaques (n = 30) | Noncomplex Plaques (n = 51) | Complex Plaques (n = 35) | |||
| Age (years) | 67 ± 7 | 71 ± 7 ⁎ | 73 ± 7 ⁎ | 0.001 | 71 ± 7 |
| Men | 16 (53%) | 24 (47%) | 15 (43%) | 0.70 | 28 (48%) |
| Hypertension | 17 (57%) | 32 (63%) | 29 (83%) | 0.05 | 35 (60%) |
| Diabetes mellitus | 8 (27%) | 18 (35%) | 14 (40%) | 0.53 | 15 (26%) |
| Smoker | 10 (33%) | 13 (25%) | 12 (34%) | 0.64 | 10 (18%) |
| Hypercholesterolemia † | 13 (43%) | 21 (41%) | 17 (49%) | 0.80 | 13 (22%) ‡ |
| Coronary artery disease | 5 (17%) | 14 (27%) | 16 (46%) ⁎ | 0.03 | 6 (10%) ‡ |
| Left ventricular ejection fraction (%) | 59 ± 10 | 59 ± 8 | 56 ± 12 | 0.21 | — |
| Peak aortic velocity (m/s) | 5.0 ± 0.7 | 4.8 ± 0.9 | 4.5 ± 1.1 | 0.09 | — |
| Aortic valve area (cm 2 ) | 0.70 ± 0.12 | 0.69 ± 0.17 | 0.67 ± 0.15 | 0.86 | — |
‡ p <0.05 vs. aortic stenosis.
† Total cholesterol >220 mg/dl or use of cholesterol-lowering medications.
Chronic cerebral infarction was detected in 15 of 116 patients with AS. Cerebral infarction occurred in 2 patients after cardiac catheterization and in 4 patients after AVR. The prevalence of chronic cerebral infarction was significantly greater in patients with complex arch plaques than in those without complex arch plaques (31% vs 5%; p = 0.0003). The incidence of cerebral infarction after cardiac procedures was also significantly greater in patients with complex plaques (14% vs 1%; p = 0.009). Overall, the prevalence of cerebral infarction (chronic cerebral infarction or cerebral infarction after cardiac procedures) was greater in patients with complex arch plaques than those without complex arch plaques (40% vs 6%; p <0.0001; Figure 3 ).
Univariate logistic analyses showed that age, coronary artery disease, and complex arch plaques were associated with cerebral infarction. However, atrial fibrillation was not (odds ratio 1.93, 95% confidence interval 0.60 to 6.15; p = 0.27). On multivariate logistic analyses, after adjusting for traditional atherosclerotic risk factors and coronary artery disease, the presence of complex arch plaques was found to be an independent risk factor for cerebral infarction in patients with severe AS (odds ratio 8.46, 95% confidence interval 2.38 to 30.12; p = 0.001; Table 2 ).



