Leukocyte telomere length has been proposed as a biomarker of cellular aging and atherosclerosis. The aim of this study was to determine whether leukocyte telomere length is independently associated with incident coronary heart disease (CHD) in the general population. Telomere length was measured using a polymerase chain reaction method for participants enrolled in the 1995 Nova Scotia Health Survey (NSHS95; n = 1,917). The primary end point was the first occurrence of a fatal or nonfatal CHD event. During a mean follow-up period of 8.7 years, 164 fatal or nonfatal CHD events occurred. Compared with participants in the longest tertile of telomere length, those in the middle and shortest tertiles had increased incidence of CHD events (6.2, 11.2, and 12.2 per 1,000 person-years, respectively). After adjustment for demographics, traditional risk factors, and inflammatory markers including high-sensitivity C-reactive protein, interleukin-6, and soluble intercellular adhesion molecule–1, those in the middle tertile had significantly elevated risk for incident CHD (hazard ratio 1.63, 95% confidence interval 1.07 to 2.51, p = 0.02) compared with the longest tertile, whereas the risk for those in the shortest tertile was nonsignificantly elevated (hazard ratio 1.25, 95% confidence interval 0.82 to 1.90, p = 0.30). In conclusion, these findings do not support a linear association between leukocyte telomere length and incident CHD risk in the general population.
Telomere length has been proposed as a novel biomarker for vascular aging and for coronary heart disease (CHD) onset. In 2003, Cawthon et al reported that shorter leukocyte telomere length was associated with an increased age-adjusted risk for cardiovascular mortality in a convenience sample of 143 initially healthy subjects. Since that report, discordant findings have been published, with some studies showing weak or no association between leukocyte telomere length and cardiovascular risk and others suggesting a moderate to strong association. These studies had notable limitations, such as restricting enrollment to the very elderly, leading to possible survival bias ; the inclusion of participants with previous CHD, who are already at increased risk for subsequent events ; and limited adjustment for important confounders such as traditional CHD risk factors. Few studies have been population based, further limiting the generalizability of their findings. The extent to which leukocyte telomere length constitutes a valid biomarker for incident CHD events in the general population is thus unclear. To address this, we examined whether shorter leukocyte telomere length was associated with the development of incident CHD events in participants enrolled in the 1995 Nova Scotia Health Survey (NSHS95).
Methods
The NSHS95 is a population-based survey implemented by Heart Health Nova Scotia and the Nova Scotia Department of Health. Study participants consisted of noninstitutionalized, nonpregnant Nova Scotians aged ≥18 years and listed in the registry of the national health insurance plan. Of 4,500 targeted participants, a total of 3,227 provided informed consent and were enrolled. The overall recruitment percentage (72%) is comparable with those obtained in other large health surveys, and weights applied from propensity score analyses revealed no meaningful response bias. The present study was approved by the institutional review boards of Dalhousie University (Halifax, Nova Scotia, Canada) and Columbia University Medical Center (New York, New York).
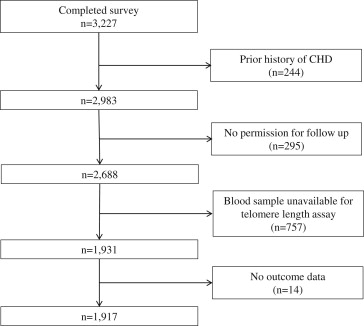
For this analysis, we excluded 1,310 participants as follows ( Figure 1 ): 244 participants with histories of CHD, as determined by claims records for the 5 years preceding the baseline survey using International Classification of Diseases (ICD), Ninth Revision codes 410.x through 414.x (myocardial infarction, acute or chronic ischemic heart disease, angina); 295 participants who did not provide permission for ascertainment of cardiac outcomes; 757 participants who did not have blood samples for telomere length assay; and 14 participants who granted permission but did not have available outcome data. The final cohort thus consisted of 1,917 participants. Compared with the 1,917 participants who had blood samples for telomere length assessment and had available outcome data, there were no significant differences in age (p = 0.20), gender (p = 0.52), and Framingham risk score (p = 0.92) as defined in the following discussion for participants who did not have telomere length assessment and/or outcome data (n = 771).
From March through November 1995, a group of trained nurses contacted eligible subjects and interviewed those who agreed to participate. Those who were interviewed also visited a health care clinic approximately 1 week afterward. At the clinic visit, height and weight were measured, and a comprehensive set of cardiovascular risk factors and full medical history were assessed. A fasting blood sample was obtained and processed for plasma and buffy coat samples. Medication use was recorded during a home visit.
Deoxyribonucleic acid (DNA) was extracted from frozen buffy coat samples. Average telomere length was determined using a real-time polymerase chain reaction (PCR) method modified from that of Cawthon et al. Real-time PCR was performed using a CFX384 thermocycler (Biorad, Richmond, California). The assay method was optimized for use of telomere (T) and single copy gene (S) amplifications on the same 384-well plate, with reference standard DNA samples on each plate. Test DNA samples each underwent 2 triplicate PCR reactions, with the use of calibrator samples for correction of interplate variability. Amplification primers for telomeres included T for : 5′-CGGTTTGTTTGGGTTTGGGTTTGGGTTTGGGTTTGGGTT-3′ and T rev : 5′- GGCTTGCCTTACCCTTACCCTTACCCTTACCCTTACCCT-3′, and for single copy gene (β-globin) S for 5′-GCTTCTGACACAACTGTGTTCACTAGC-3′ and S rev 5′-CACCAACTTCATCCACGTTCACC-3′. Thermocycling parameters were 95°C × 10-minute activation, followed by 34 cycles of 95°C × 15 seconds and 55°C × 120 seconds. The assay coefficient of variance was 5% to 8%. Because the T/S ratio depends on particular DNA standards used, T/S ratios were converted to telomere base pairs using the formula base pairs = (1,585 × T/S ratio) + 3,582, derived from coanalysis of 19 selected DNA samples (r = 0.90), using PCR and terminal restriction fragment methods (nonradioactive TeloTAGGG Telomere Length; Roche Diagnostics GmbH, Mannheim, Germany). Because telomere base pairs are calculated from T/S ratio in a linear fashion, tertiles of telomere length and all resulting statistics were identical between the 2 measurements. In this analysis, we present telomere length results in base pairs, although caution should be used in comparing absolute telomere length measurements between studies because of differing methodologies.
Participants’ ages and gender were recorded from the provincial health insurance registry and verified by the interviewer. Body mass index was calculated as weight in kilograms divided by the square of height in meters. Systolic blood pressure and diastolic blood pressure were measured using manual sphygmomanometers. Total cholesterol, high-density lipoprotein cholesterol, and triglyceride levels were assayed from plasma samples, and low-density lipoprotein cholesterol was calculated using the Friedewald formula. History of diabetes was ascertained by self-report. Those who reported smoking currently or in the past year were considered smokers. Framingham risk score was calculated using age, gender, total and high-density lipoprotein cholesterol levels, systolic blood pressure, and histories of diabetes and cigarette smoking. Lipid-lowering medication use was defined as the use of statins, fibrates, bile acid sequestrants, or nicotinic acid. Physical activity was assessed using the Paffenbarger scale. Three inflammatory markers, high-sensitivity C-reactive protein (hs-CRP), interleukin-6 (IL-6), and soluble intercellular adhesion molecule–1 (sICAM-1), were measured from plasma samples. Hs-CRP was measured using a latex-enhanced immunonephelometry assay (Cardiophase BN II; Dade Behring, New Castle, Delaware). IL-6 was assessed using a high-sensitivity enzyme-linked immunosorbent assay kit (Quantikine HS IL-6; R&D Systems, Minneapolis, Minnesota) and sICAM-1 using a commercially available enzyme-linked immunosorbent assay kit (R&D Systems). Additional details of study procedures and biomarkers assessments have been published previously.
The primary outcome measure was time to the first occurrence of a fatal or nonfatal CHD event, as determined from hospital discharge codes (ICD, Ninth Revision, codes 410 through 414 and ICD, 10th Revision, codes I21 to I25) and causes of death listed on death certificates. In Canada, the available medical care utilization data included nearly all hospital care delivered to the survey participants. The ICD codes were gathered from the provincial hospital discharge database for a 10-year period after the date of the baseline assessment. For nonfatal CHD events, personnel who performed abstraction were trained and certified and met regularly with a data quality committee from the Department of Health (Nova Scotia) to ensure accuracy and to adjudicate data entry irregularities. In Canada, Statistics Canada keeps vital statistics at the national level, capturing all deaths, including those that occur at home. Causes of death were coded using ICD codes through a nationally consistent process. For secondary analyses, we also examined the combined end point of fatal or nonfatal CHD events or all-cause mortality, as well as all-cause mortality only, nonfatal CHD events only, and fatal CHD events only.
For the primary analysis, on the basis of previous studies, the exposure variable was specified a priori as tertiles of telomere length. Baseline demographics and cardiovascular risk factors as well as levels of inflammatory markers were calculated by tertiles of telomere length. Testing for trend of association of baseline characteristics with increasing tertiles of telomere length was performed using Goodman and Kruskal’s gamma statistic for categorical variables and the chi-square statistic from linear regression for continuous variables. The association between log-transformed telomere length (because of skewed distribution) and age was assessed using linear regression. To determine the relation between telomere length and incident CHD events, 3 Cox proportional-hazards regression models were constructed to estimate the hazard ratios (HR) of having telomere length in the middle and shortest tertiles compared with the longest tertile (the reference group). Model 1 adjusted only for age and gender; model 2 adjusted for variables in model 1 plus body mass index, Framingham risk score as a continuous variable, use of lipid-lowering medications, and physical activity; and model 3 adjusted for variables in model 2 plus inflammatory biomarker levels including log-transformed hs-CRP and log-transformed IL-6 (both because of skewed distributions), and sICAM-1. Next, secondary end points (the composite of fatal and nonfatal CHD events and all-cause mortality, all-cause mortality only, nonfatal CHD events only, and fatal CHD events only) were used as outcome measures in fully adjusted models that included all covariates in model 3. Because telomere biology may differ between men and women, sensitivity analyses were performed using tertiles stratified by gender. For each model, assumptions of proportional hazards were verified using a formal significance test based on Schoenfeld residuals. A test of nonlinearity was conducted by considering tertiles of telomere length as linear and quadratic terms while adjusting for all other covariates in model 3. All statistical analyses were performed using Stata version 10.0 (StataCorp LP, College Station, Texas) and SPSS version 18.0 (IBM, Chicago, Illinois).
Results
For the 1,917 participants included for this analysis, the mean age was 46.6 ± 18.4 years, and 51% were women. Tests for linear trends demonstrated that participants in shorter tertiles of telomere length were older, were less likely to be smokers, had higher systolic and diastolic blood pressures, had higher Framingham risk score and risk categories, had higher levels of low-density lipoprotein cholesterol, and had higher levels of hs-CRP ( Table 1 ). Log telomere length was inversely correlated with age (r = −0.22, R 2 = 0.049, p <0.001). For each decade increase in age, a 1.3% (95% confidence interval [CI] 1.0% to 1.5%) decrease in telomere length was observed (p <0.001).
| Characteristic | Tertiles of Telomere Length (kb) | p Value ∗ | ||
|---|---|---|---|---|
| 5.5 to 8.2 (n = 639) | 5.0 to <5.5 (n = 639) | 4.1 to <5.0 (n = 639) | ||
| T/S ratio | 1.20 to 2.90 | 0.92 to <1.20 | 0.30 to <0.92 | |
| Age (yrs) | 41.7 ± 18.0 | 46.1 ± 17.8 | 51.8 ± 18.1 | <0.001 |
| Women | 330 (51.6%) | 340 (53.2%) | 308 (48.2%) | 0.11 |
| Smokers | 193 (30.2%) | 160 (25.0%) | 158 (24.7%) | 0.01 |
| Body mass index (kg/m 2 ) | 26.6 (5.4) | 27.2 (6.1) | 27.1 (5.0) | 0.10 |
| Diabetes mellitus | 21 (3.3%) | 26 (4.1%) | 23 (3.6%) | 0.38 |
| Systolic blood pressure (mm Hg) | 123.3 ± 16.1 | 124.6 ± 17.7 | 127.1 ± 17.5 | <0.001 |
| Diastolic blood pressure (mm Hg) | 76.0 ± 9.9 | 77.0 ± 9.5 | 77.5 ± 9.2 | 0.01 |
| Low-density lipoprotein | ||||
| mmol/L | 3.1 ± 0.9 | 3.2 ± 0.9 | 3.4 ± 0.9 | <0.001 |
| mg/dl | 119.9 ± 34.8 | 123.7 ± 34.8 | 131.5 ± 34.8 | |
| High-density lipoprotein | ||||
| mmol/L | 1.3 ± 0.3 | 1.3 ± 0.3 | 1.3 ± 0.4 | 0.42 |
| mg/dl | 50.3 ± 11.6 | 50.3 ± 11.6 | 50.3 ± 15.5 | |
| Use of lipid-lowering medications | 21 (3.3%) | 18 (2.8%) | 16 (2.5%) | 0.20 |
| Framingham risk score | −0.8 ± 9.9 | 1.5 ± 8.9 | 3.7 ± 8.0 | <0.001 |
| Framingham risk category | <0.001 | |||
| 0%–10% | 491 (76.8%) | 466 (72.9%) | 394 (61.7%) | |
| 10%–20% | 75 (11.7%) | 111 (17.4%) | 139 (21.8%) | |
| >20% | 73 (11.4%) | 62 (9.7%) | 106 (16.6%) | |
| hs-CRP (mg/L) † | 1.4 (0.5–3.4) | 1.6 (0.5–3.6) | 1.9 (0.7–4.4) | 0.005 |
| IL-6 (pg/ml) † | 1.1 (0.7–1.9) | 1.1 (0.7–1.9) | 1.2 (0.8–2.2) | 0.38 |
| sICAM-1 (ng/ml) | 635.5 ± 341.7 | 543.2 ± 328.2 | 528.4 ± 313.9 | <0.001 |
∗ Calculated using Goodman and Kruskal’s gamma statistic for categorical variables and the chi-square statistic derived from linear regression for continuous variables.
† Trend testing for hs-CRP and IL-6 was performed after log transformation because of skewed distribution.
During a mean follow-up period of 8.7 years, 164 fatal or nonfatal CHD events occurred. The incidence of fatal and nonfatal CHD events was higher for participants in the middle and shortest tertiles compared with those in the longest tertile ( Table 2 , Figure 2 ). After adjusting for age and gender, participants in the middle tertile continued to have a significantly increased risk for incident CHD (HR 1.63, 95% CI 1.08 to 2.47, p = 0.02), whereas participants in the shortest tertile had a nonsignificantly increased risk (HR 1.22, 95% CI 0.81 to 1.83, p = 0.35; Table 2 , model 1). These relations were similar after adjustment for body mass index, Framingham risk score, baseline lipid-lowering medication use including statins, and physical activity ( Table 2 , model 2) and further adjustment for inflammatory biomarkers including hs-CRP, IL-6, and sICAM-1 ( Table 2 , model 3). Nonlinearity of the association of tertiles of telomere length with incident CHD events was demonstrated using a model that included tertiles of telomere length as linear and quadratic terms (p = 0.028) in addition to all other covariates in model 3.



