The objectives of this study were to describe contemporary postdischarge death rates of patients hospitalized at all Worcester, Massachusetts, hospitals after initial acute myocardial infarctions (AMIs) and to examine factors associated with a poor prognosis. The medical records of patients discharged from 11 central Massachusetts medical centers after initial AMIs during 2001, 2003, 2005, and 2007 were reviewed, identifying 2,452 patients. This population was composed of predominantly older patients, men (58%), and whites. Overall, the 3-month, 1-year, and 2-year all-cause death rates were 8.9%, 16.4%, and 23.4%, respectively. Over time, reductions in postdischarge mortality were observed in crude as well as multivariate-adjusted analyses. In 2001, the 3-month, 1-year, and 2-year all-cause death rates were 11.1%, 17.1%, and 25.6%, respectively, compared to rates of 7.9%, 12.7%, and 18.6% in patients discharged in 2007. Older age, male gender, hospitalization for a non–ST-segment elevation AMI, renal dysfunction, and preexisting heart failure were associated with an increased risk for dying after hospital discharge. These results suggest that the postdischarge prognosis of patients with initial AMIs has improved, likely reflecting enhanced in-hospital and postdischarge management practices. In conclusion, patients with initial AMIs can also be identified who are at increased risk for dying after hospital discharge, in whom increased surveillance and targeted treatment approaches can be directed.
Using data from the Worcester Heart Attack Study, we describe trends in postdischarge total mortality in residents of the Worcester, Massachusetts, metropolitan area who survived hospitalization for initial acute myocardial infarctions (AMIs) in recent years and factors associated with a poor long-term prognosis.
Methods
The Worcester Heart Attack Study is an ongoing clinical and epidemiologic investigation examining long-term trends in the incidence, hospital, and postdischarge case-fatality rates of AMI among residents of the Worcester metropolitan area hospitalized at all greater Worcester medical centers in 16 biennial periods from 1975 to 2007. Residents of the Worcester metropolitan area hospitalized with principal or secondary discharge diagnoses of AMI (International Classification of Diseases, Ninth Revision, code 410) were included in our study. In addition, a random sample of records from related diagnostic rubrics in which the diagnosis of AMI might have occurred (e.g., International Classification of Diseases, Ninth Revision, codes 411 to 414) was carried out to identify potentially misclassified cases of AMI. This study was approved by the institutional review board at the University of Massachusetts Medical School.
The present study sample consisted of patients hospitalized at all 11 greater Worcester medical centers during the most recent years under study (2001, 2003, 2005, and 2007) to provide more contemporary insights into possible changing trends in the long-term prognosis of patients with first AMIs.
Cases of AMI were defined as having ≥2 of 3 clinical, serum biomarker, or electrocardiographic criteria present. Standardized definitions for the classification of type of AMI (ST-segment AMI and non–ST-segment AMI [NSTEMI]) were used. Cases of perioperative or trauma-associated AMI were excluded, as were patients with prior diagnoses of AMI, on the basis of a review of information contained in hospital medical records or with electrocardiographic changes indicative of previous myocardial necrosis. The clinical complications of AMI that may have developed during hospitalization were assessed on the basis of information available from medical records and the use of standardized diagnostic criteria.
The approaches used to ascertain survival status after hospital discharge included a review of medical records for additional hospitalizations and a statewide search of death certificates. Our principal study end point was all-cause mortality. For patients discharged from all central Massachusetts hospitals, follow-up was continued through 2009.
Differences in the distribution of demographic and clinical characteristics between respective comparison groups were examined using chi-square tests for discrete variables and Student’s t tests for continuous variables. A life-table approach was used to examine the overall long-term death rates, and trends in long-term prognosis, after hospital discharge. A logistic multiple regression approach was used to identify factors associated with postdischarge mortality at 3 and 24 months after hospital discharge. These times points were chosen because several previous investigations have shown these follow-up points to be high-risk periods for patients discharged from the hospital after AMIs. In our regression models, we did not control for the use of different cardiac treatment approaches, because we could not account for confounding by treatment indication given the nonrandomized nature of this study.
Results
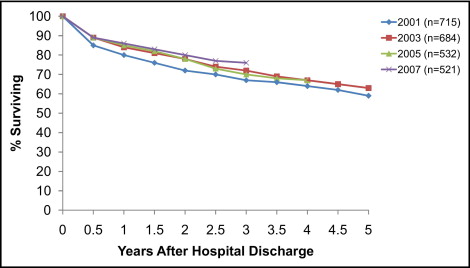
The study population consisted of 2,452 residents of the Worcester metropolitan area who were discharged from all central Massachusetts hospitals after incident AMIs from 2001 to 2007 and in whom further follow-up information was obtained. Of these, 715 patients were discharged in 2001, 684 in 2003, 532 in 2005, and 521 patients in 2007.
Overall, the population was predominately Caucasian with an average age of 69 years, 42% were women, and most were diagnosed with NSTEMI ( Table 1 ). The 2 most common cardiovascular co-morbidities in these patients were hypertension and diabetes. Length of hospital stay averaged 5.6 days, and a considerable proportion of patients developed heart failure or atrial fibrillation (AF) while hospitalized. In comparing the characteristics of patients hospitalized in 2001 and 2007, there was a decrease in the average age at the time of the patient’s index hospitalization, length of stay, and slightly lower levels of serum glucose, total cholesterol, and low-density lipoprotein cholesterol ( Table 1 ).
| Characteristic | Overall Population (n = 2,452) | 2001 Cohort (n = 715) | 2007 Cohort (n = 521) |
|---|---|---|---|
| Age (years) | |||
| Mean | 68.7 | 69.2 | 66.3 |
| <65 | 933 (38.1%) | 256 (35.8%) | 216 (41.5%) |
| 65–74 | 484 (19.8%) | 162 (22.7%) | 80 (15.4%) |
| 75–84 | 636 (26.0%) | 200 (28.0%) | 141 (27.2%) |
| ≥85 | 397 (16.2%) | 97 (13.6%) | 82 (15.8%) |
| Male | 1,414 (57.7%) | 425 (59.4%) | 316 (60.7%) |
| White | 2,180 (88.9%) | 646 (90.4%) | 465 (89.3%) |
| Prehospital delay (hours) | 3.9 | 3.4 | 3.5 |
| Length of stay (days) | 5.6 | 6.6 | 4.8 |
| ST-segment elevation AMI | 913 (37.2%) | 284 (39.7%) | 179 (34.4%) |
| Angina pectoris | 336 (13.7%) | 130 (18.2%) | 39 (7.5%) |
| Hypertension | 1,638 (66.8%) | 450 (62.9%) | 357 (68.5%) |
| Atrial fibrillation | 270 (11.0%) | 79 (11.1%) | 60 (11.5%) |
| Diabetes mellitus | 674 (27.5%) | 206 (28.8%) | 146 (28.0%) |
| Heart failure | 356 (14.5%) | 107 (15.0%) | 63 (12.1%) |
| Stroke | 207 (8.4%) | 65 (9.1%) | 45 (8.6%) |
| Kidney disease | 329 (13.4%) | 78 (10.9%) | 90 (17.3%) |
| Physiologic variables | |||
| Ejection fraction (%) | 49 | 48 | 50 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 63 | 62 | 66 |
| Diastolic blood pressure (mm Hg) | 79 | 80 | 79 |
| Systolic blood pressure (mm Hg) | 144 | 146 | 142 |
| Glucose (mg/dl) | 169 | 178 | 159 |
| Total cholesterol (mg/dl) | 180 | 186 | 173 |
| Hospital complications | |||
| AF | 477 (19.5%) | 134 (18.7%) | 90 (17.3%) |
| Heart failure | 780 (31.8%) | 228 (31.9%) | 170 (32.6%) |
| Cardiogenic shock | 87 (3.6%) | 32 (4.5%) | 24 (4.6%) |
| Stroke | 21 (0.9%) | 6 (0.8%) | 2 (0.4%) |
The overall postdischarge death rates at 3 months, 1 year, and 2 years were 8.9%, 16.4%, and 23.4%, respectively ( Figure 1 ). We observed a decrease in the death rate at each of these time points in patients discharged in the most recent study year compared to those discharged during earlier study years. The 3-month death rate decreased from 11.1% in 2001 to 7.9% in 2007, the 1-year death rate decreased from 17.1% to 12.7%, and the 2-year death rate decreased from 25.6% to 18.6% ( Figure 1 ). After we adjusted for several baseline demographic, medical history, and clinical characteristics, patients discharged from the hospital in 2007 were more likely to have survived to 3 months (odds ratio 0.53, 95% confidence interval 0.43 to 0.98), 1 year (odds ratio 0.74, 95% confidence interval 0.48 to 1.14), and 2 years (odds ratio 0.95, 95% confidence interval 0.61 to 1.49) compared to those discharged in 2001.
We examined factors associated with an increased risk for dying at 3 months using a logistic regression model ( Table 2 ). Being older, being male, having an NSTEMI, and having a history of stroke, heart failure, and kidney disease were important predictors of 3-month death rates. The development of AF, heart failure, cardiogenic shock, or a stroke during hospitalization was associated with a significantly poorer prognosis at 3 months; a low systolic blood pressure at the time of hospital presentation was also an important predictor of dying during the first 3 months of hospital discharge.
| Characteristic | 0–3 Months | 3–24 Months | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age (years) | ||||
| 55–64 | 0.92 | 0.31–2.68 | 1.71 | 0.82–3.57 |
| 65–74 | 3.51 | 1.46–3.48 | 4.96 | 2.55–9.68 |
| ≥75 | 7.88 | 3.39–18.35 | 7.77 | 4.04–14.94 |
| Male | 1.40 | 1.02–1.93 | 1.34 | 1.02–1.76 |
| White race | 1.25 | 0.70–2.21 | 1.18 | 0.76–1.83 |
| Length of stay | 1.03 | 1.00–1.05 | 1.02 | 0.99–1.04 |
| ST-segment elevation myocardial infarction | 0.81 | 0.56–1.18 | 0.53 | 0.38–0.73 |
| Co-morbidities | ||||
| Hypertension | 0.72 | 0.50–1.04 | 0.92 | 0.67–1.28 |
| AF | 1.31 | 0.86–2.02 | 0.60 | 0.41–0.87 |
| Stroke | 1.83 | 1.20–2.78 | 1.61 | 1.08–2.40 |
| Heart failure | 1.88 | 1.29–2.74 | 2.22 | 1.58–3.11 |
| Diabetes | 1.33 | 0.92–1.93 | 1.04 | 0.75–1.43 |
| Kidney disease | 1.65 | 1.11–2.45 | 1.31 | 0.90–1.91 |
| In-hospital complications | ||||
| AF | 1.56 | 1.10–2.21 | 0.66 | 0.47–0.93 |
| Heart failure | 1.60 | 1.13–2.25 | 1.60 | 1.19–2.13 |
| Cardiogenic shock | 1.86 | 0.95–3.67 | 2.42 | 1.25–4.69 |
| Stroke | 3.30 | 1.13–9.64 | 1.83 | 0.56–6.02 |
| Hemorrhage | 1.37 | 0.96–1.94 | 1.19 | 0.88–1.61 |
| Physiologic variables | ||||
| Systolic blood pressure (mm Hg) | ||||
| <100 | 1.76 | 1.03–3.03 | 1.16 | 0.67–2.04 |
| 120–139 | 0.79 | 0.50–1.27 | 0.84 | 0.56–1.27 |
| 140–159 | 0.67 | 0.42–1.08 | 0.59 | 0.39–0.88 |
| ≥160 | 0.60 | 0.38–0.96 | 0.74 | 0.50–1.08 |
| Estimated glomerular filtration rate (ml/min/1.73m 2 ) | ||||
| <30 | 1.65 | 0.97–2.79 | 4.14 | 2.59–6.64 |
| 30–59 | 1.19 | 0.82–1.73 | 1.41 | 1.04–1.91 |
| Glucose (mg/dl) | ||||
| <80 | 1.07 | 0.33–3.47 | 1.34 | 0.42–4.29 |
| 110–140 | 1.09 | 0.66–1.80 | 0.82 | 0.54–1.24 |
| 140–180 | 1.03 | 0.61–1.73 | 1.23 | 0.81–1.85 |
| ≥180 | 0.95 | 0.56–1.62 | 1.08 | 0.70–1.66 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


