Although 2-dimensional (2D) transesophageal echocardiography (TEE) is the gold standard for the diagnosis of prosthetic valve thrombosis, nonobstructive clots located on mitral valve rings can be missed. Real-time 3-dimensional (3D) TEE has incremental value in the visualization of mitral prosthesis. The aim of this study was to investigate the utility of real-time 3D TEE in the diagnosis of mitral prosthetic ring thrombosis. The clinical outcomes of these patients in relation to real-time 3D transesophageal echocardiographic findings were analyzed. Of 1,263 patients who underwent echocardiographic studies, 174 patients (37 men, 137 women) with mitral ring thrombosis detected by real-time 3D TEE constituted the main study population. Patients were followed prospectively on oral anticoagulation for 25 ± 7 months. Eighty-nine patients (51%) had thrombi that were missed on 2D TEE and depicted only on real-time 3D TEE. The remaining cases were partially visualized with 2D TEE but completely visualized with real-time 3D TEE. Thirty-seven patients (21%) had thromboembolism. The mean thickness of the ring thrombosis in patients with thromboembolism was greater than that in patients without thromboembolism (3.8 ± 0.9 vs 2.8 ± 0.7 mm, p <0.001). One hundred fifty-five patients (89%) underwent real-time 3D TEE during follow-up. There were no thrombi in 39 patients (25%); 45 (29%) had regression of thrombi, and there was no change in thrombus size in 68 patients (44%). Thrombus size increased in 3 patients (2%). Thrombosis was confirmed surgically and histopathologically in 12 patients (7%). In conclusion, real-time 3D TEE can detect prosthetic mitral ring thrombosis that could be missed on 2D TEE and cause thromboembolic events.
Prosthetic valve thrombosis (PVT) is a life-threatening complication that usually occurs on mitral prostheses in patients with inadequate levels of anticoagulation. The true incidence of mitral PVT is unknown because data are based on autopsy and surgical findings, which do not include the large number of nonobstructive cases. Two-dimensional (2D) transesophageal echocardiography (TEE) has been the conventional diagnostic method for detecting obstructive and nonobstructive PVT. However, nonobstructive PVT can be missed with 2D imaging. Real-time 3-dimensional (3D) TEE provides a live “en face” surgical view of the mitral valve, which can improve diagnostic accuracy for detecting mitral prosthetic valve pathologies. In this study, we compared the diagnostic and clinical utility of real-time 3D TEE and 2D TEE in a previously underrecognized pathology, namely, nonobstructive, “Doppler-silent,” annular-type, mitral ring–located PVT.
Methods
From November 2008 to December 2012, 1,263 patients with mechanical prosthetic mitral valves underwent 2D transthoracic echocardiography, 2D TEE, and real-time 3D TEE at the Heart Valve Center of Kosuyolu Kartal Heart Training and Research Hospital (Istanbul, Turkey). Mechanical mitral PVT was diagnosed in 242 patients (19%). Patients with obstructive thrombi (n = 37), left atrial (n = 2) and left atrial appendage (n = 4) thrombi, severe spontaneous echocardiographic contrast (n = 8), left ventricular ejection fractions ≤30% (n = 3), and poor real-time 3D transesophageal echocardiographic image quality (n = 12) were excluded. Two patients with clinical and laboratory findings suggesting infective endocarditis were also excluded. The remaining 174 patients with mitral ring thrombosis constituted the main study population. The study group was monitored closely on therapeutic anticoagulation. Patients with histories of thromboembolism or with other clinical indications were reevaluated every 6 months with history and physical examination, 2D transthoracic echocardiography, 2D TEE, and real-time 3D TEE. Written informed consent was obtained from the participants, and the study was approved by the local ethics board.
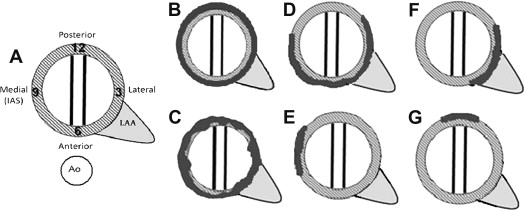
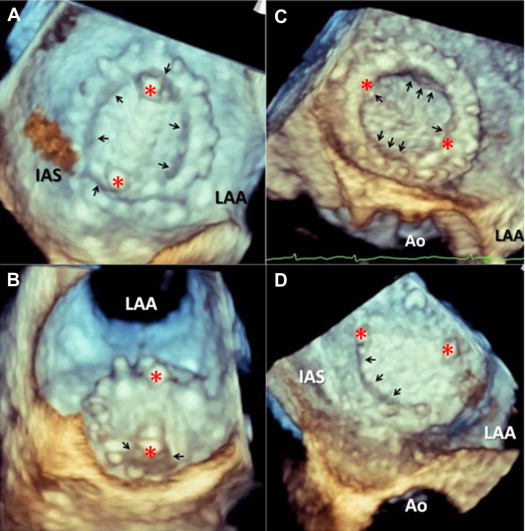
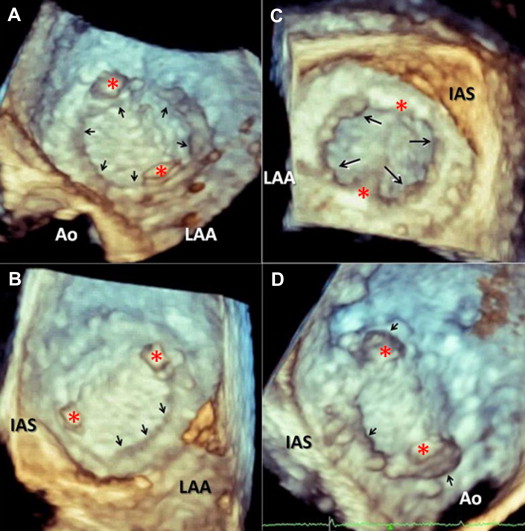
TEE was performed using an x7-2t transducer on an iE33 ultrasound machine (Philips Medical Systems, Andover, Massachusetts) capable of multiplane 2D and real-time 3D imaging. Two-dimensional and 3D TEE were performed during the same procedure, and 2D images were interpreted before the 3D images. Transmitral gradients and effective orifice area were measured using 2D transthoracic echocardiography according to current guidelines. Gain settings were optimized using the narrow-angle acquisition mode, which allows real-time 3D imaging of a pyramidal volume of approximately 30° × 60°. The 3D zoom mode was subsequently used to image prosthetic valves. An en face view of the mitral valve from the left atrium (the surgeon’s-eye view) was carefully reconstructed for each patient when the mitral valve was closed because this method provided the best contrast to detect thrombus. Linear, purple- or violet-colored echodensity on a bright cream color base of the endothelialized sewing ring surrounding the prosthetic valve suture line or medial to it suggested thrombus. A thrombus was defined as a soft and homogenous, mobile or fixed echodensity, similar to myocardium, located at the valve occluder, hinges, and/or valve struts by 2D TEE. The largest diameter of the thrombus and the length of the mobile portion, if present, were measured. The location of a thrombus was described using a clockwise format in relation to the aortic valve ( Figure 1 ). Characteristics of the thrombi were analyzed according to their locations, morphologies, sizes, mobility, and hemodynamic features. Thrombi may be present anywhere along the sewing ring of the annulus, including the hinges and/or struts ( Figures 1 to 3 ). An echodense thrombus located along the annulus may be a regular or irregular shape ( Figures 1 to 3 ). Thrombi could either extend toward the orifice or remain as a single thin strip. They may be either sessile and immobile or pedunculated and mobile, making them visible on 2D TEE.
The subgroup of patients (n = 18) with “Doppler-positive” mitral PVT (mean transmitral gradient 11 ± 3 mm Hg, mean valve area 1.2 ± 0.3 cm 2 ) had annular ring–located PVT with accompanying tissue overgrowth, most likely pannus formation on the basis of transthoracic echocardiographic, 2D transesophageal echocardiographic, and real-time 3D transesophageal echocardiographic findings. An increased transmitral gradient with decreased valve area, without evidence of inadequate anticoagulation and visible thrombi, suggested pannus overgrowth. A diagnosis of pannus formation was made when fixed, bright, echodense structures, sometimes containing focal calcific deposits, were present primarily along the valve ring with extension into the valve orifice on 2D TEE. Visualization of the atrial and ventricular sides of the prosthesis by on real-time 3D TEE provided improved understanding of the relation between cardiac structures and helped discriminate pannus from thrombus.
Two-dimensional and 3D images were initially evaluated by 2 experienced echocardiographers independently; they were transferred to the Philips Xcelera workstation and analyzed off-line by the first reviewer in a subsequent session. In 50 randomly selected patients with ring-located nonobstructive thrombosis, intraobserver (first echocardiographer) and interobserver agreement for exact 3D localization of the annular thrombi was 98% and 90%, respectively.
Continuous variables are presented as medians and interquartile ranges or as mean ± SD as appropriate. Categorical variables are presented as observed frequencies and percentages. The variables were investigated using analytic methods (Kolmogorov-Smirnov or Shapiro-Wilk test) to determine whether they were normally distributed. Because the thickness and length of thrombi were not normally distributed, Mann-Whitney tests were conducted to compare 3D measurements. Categorical data were compared using chi-square or Fisher’s exact tests. SPSS for Windows version 16.0 (SPSS, Inc., Chicago, Illinois) was used for statistical analysis.
Results
The baseline characteristics of the patients with and without ring thrombosis are listed in Table 1 .
| Characteristic | Patients Without PVT (n = 1,021) | Patients With Ring Thrombosis ∗ (n = 174) | p Value |
|---|---|---|---|
| Age (yrs) | 47 ± 18 (16–76) | 49 ± 11 (21–76) | 0.22 |
| Men/women | 267 (26%)/754 (74%) | 37 (21%)/137 (79%) | 0.52 |
| Time since valve replacement (mos) | 57 ± 42 (1–256) | 60 ± 6 (1–228) | 0.72 |
| Type of mitral prosthesis (single-leaflet/bileaflet) | 43 (4%)/978 (96%) | 12 (7%)/162 (93%) | 0.40 |
| Hypertension | 114 (11%) | 22 (13%) | 0.73 |
| Diabetes mellitus | 77 (7.5%) | 11 (6.3%) | 0.65 |
| Cardiac rhythm (atrial fibrillation/sinus rhythm) | 446 (44%)/575 (56%) | 84 (48%)/90 (52%) | 0.42 |
| Level of anticoagulation (adequate/inadequate) | 806 (79%)/215 (21%) | 23 (13%)/151 (87%) | <0.001 |
| New York Heart Association functional class (I or II/III or IV) | 950 (93%)/71 (7%) | 156 (90%)/18 (10%) | 0.58 |
| Admission with thromboembolism | 49 (5%) | 37 (21%) | <0.001 |
Eighty-nine of the 174 main study patients (51%) had mitral nonobstructive ring PVT that was not visible on initial 2D TEE and were depicted only on real-time 3D TEE (group 1). The remaining 85 patients (49%) had ring thrombosis that could be visualized partially with 2D TEE and completely with real-time 3D TEE (group 2). The annular thrombi in group 1 were always localized on the valve ring, had smaller sizes and regular shapes, and did not extend toward the valve orifice. In contrast, the annular thrombi in group 2 extended toward the valve hinges and orifice and had larger sizes and irregular shapes. There were no difference in baseline characteristics and presenting symptoms between these 2 groups of patients. Coexisting conditions included echocardiographically suspected pannus overgrowth in 18 patients (10%) and severe paravalvular leak in 7 patients (4%).
PVT was detected at various localizations: 1 or 2 hinges and/or 1 or both half sides of the annular ring (Figures 1 to 3 ). Thirty patients (17%) had fully covered ring PVT along the annulus. Sixty-six patients (38%) had PVT extending on more than half of the annulus, and 78 patients (45%) had relatively smaller PVT involving the rear (behind) and/or over hinges, over sewing ring sparing 1 or both hinges. At least 1 of the hinges was thrombosed in 113 patients (65%). Left atrial appendage vicinity involvement was present in 97 patients (56%). In the subgroup with pannus formation (n = 18), ring-located PVT had circumscribed the whole annulus in 9 patients. Overall, 147 patients (84%) had regular shaped ring PVT ( Figure 1 ) without extending into the orifice, forming a bandlike appearance. The rest were irregularly shaped with exceeding edges, especially at the vicinity of hinges and left atrial appendage ( Figure 1 ).
Thirty-seven patients (21%) with ring thrombosis had histories of recent thromboembolic events at the time of admission. This included transient ischemic attacks (n = 22), ischemic strokes (n = 8), coronary embolism (n = 5), retinal embolus (n = 1), and renal thromboembolism (n = 1) ( Figure 3 ). The main clinical and echocardiographic characteristics of the study patients (n = 174) admitted with and without thromboembolism are listed in Table 2 . The mean thickness and length of thrombi were significantly higher in patients with thromboembolism compared with patients without thromboembolism. There was no statistical difference with regard to the presence of mobile thrombus >2 mm ( Table 2 ).
| Characteristic | Thromboembolism (n = 37 [21%]) | No Thromboembolism (n = 137 [79%]) | p Value |
|---|---|---|---|
| Age (yrs) | 48 ± 12 | 49 ± 11 | 0.70 |
| Men/women | 5/32 | 32/105 | 0.26 |
| Time since valve replacement (mos) | 60 ± 5 | 61 ± 6 | 0.81 |
| Atrial fibrillation/sinus rhythm | 14/23 | 70/67 | 0.15 |
| International normalized ratio | 1.8 ± 0.4 | 2.0 ± 0.5 | 0.49 |
| Hypertension (yes/no) | 6/31 | 16/121 | 0.46 |
| Diabetes mellitus (yes/no) | 3/34 | 8/129 | 0.70 |
| New York Heart Association functional class | 1.9 ± 0.6 | 1.8 ± 0.4 | 0.49 |
| Echocardiographic findings | |||
| Left ventricular ejection fraction (%) | 58 ± 4 | 58 ± 6 | 0.86 |
| Left atrial diameter (mm) | 46 ± 2 | 46 ± 4 | 0.99 |
| Thickness of thrombus (mm) | 3.8 ± 0.9 | 2.8 ± 0.7 | <0.001 |
| Length of thrombus (mm) | 46 ± 10 | 29 ± 8 | <0.001 |
| Mobile thrombus (>2 mm) | 9 (24%) | 23 (17%) | 0.20 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


