Rare and Eponymous Vascular Disorders Spectrum of degenerative aortic pathology (now thought to be a variant of acute aortic dissection pathology) leading to acute, painful conditions affecting the aorta (at any point). Patients often present with pain (back pain/interscapular pain). The syndrome includes penetrating aortic ulcer (PAU) and intramural haematoma (IMH), and may represent a prequel to acute aortic dissection (or aneurysm formation). An IMH is a haematoma confined to the medial layer of the aorta (in the absence of communication between the haematoma in the false lumen and the true lumen or an identifiable aortic flap), whereas a PAU has breached the endothelium and internal elastic lamina to penetrate into the media with a risk of dissection or free rupture. An intramural haematoma may be due to spontaneous rupture of vasa vasora. A penetrating ulcer is restricted by the atherosclerotic process, thereby limiting the dissection of the vessel wall. They are both found more commonly in older patients with hypertension and typically affect the descending thoracic aorta. It is thought that an IMH is more likely to behave like a classic aortic dissection, whereas a PAU is more prone to aneurysmal degeneration (50%) and is less prone to dissection. Fifty to eighty per cent of patients with asymptomatic IMH or PAU of the descending aorta (type B) will heal spontaneously and should be treated with medical therapy alone (as in aortic dissection) with CT scan surveillance, unless the aortic diameter exceeds 4 cm (best predictor of complications). Treatment may be with stenting (preferred) or open surgery. Ascending pathology should be treated surgically because of the higher risk of complications and true progression to either dissection of aneurysmal degeneration. Recurrent trauma or repetitive motion, typically in high-performing athletes (especially cyclists), affects the external iliac artery, giving rise to claudication on extreme exercise. Repetitive trauma leads to medial fibrosis and thickening of the tunica intima. May be treated conservatively by reducing exercise workload. Classically affects younger males and heavy smokers. Also prevalent among people of Middle Eastern and Asian origin. Numerous thrombotic occlusions of small and medium-sized arteries (i.e. BK). Vessels on angiogram are normal to a sudden point of occlusion with numerous, tortuous, cork-screw collaterals. Raynaud’s phenomenon is also associated. Excellent prognosis with smoking cessation and exercise. Usually spontaneous occurrence (although traumatic dissection is associated with head and neck trauma) that may be asymptomatic or symptomatic (unexplained neurological deficit such as stroke [>50%)], TIA, Horner’s syndrome). There are three recognised subtypes: type I has vessel irregularity but no significant stenosis; type II has >70% stenosis or 50% dilatation; and type III has a characteristic ‘flame-shaped’ occlusion just above the bifurcation. Twenty-five per cent are bilateral. Treatment is with anticoagulation to reduce the risk of stroke, and most will heal within 3 and 6 months. Typically benign tumour within the adventitial layer of the common carotid artery (typically at the bifurcation), derived from embryonic neural crest cells. They are often asymptomatic, but may present as a painless neck lump. Compressive symptoms may also occur (e.g. dysphagia, hoarseness, XII nerve palsy, Horner’s syndrome). They are well encapsulated, thus allowing complete dissection from the carotid complex usually without the need for reconstruction. Five per cent are bilateral and 5% malignant (with either local or distant metastasis). See ‘May-Thurner syndrome’. Cystic degeneration of the tunica adventitia of an artery, typically affecting the popliteal artery leading to stenosis, chronic ischaemia and/or acute thrombosis. Pathologically it consists of a true cyst (epithelial lined) within the adventitia, which may be in continuity with the synovium of the knee joint. On examination, pulses are present at rest, but disappear on knee flexion. Surgical resection with popliteal artery reconstruction is the management of choice. Angioplasty should be avoided because results are poor and associated with a high complication rate (acute thrombosis and distal embolisation of cystic material). Inherited connective tissue disorder (defect in type III collagen) of which there are 10 recognised subtypes (varying genotype and phenotype), but characterised by increased elasticity of the skin, joint hypermobility, thin skin and easy bruisability. Incidence is 1 : 150,000. Types I and IV are most likely to present to a vascular service in a young population. Type I (Gravis) may have varicose veins. Type IV (Sack-Barabas) may have aneurysmal degeneration (especially thoracic and abdominal aorta) or even spontaneous arterial rupture (and/or gravid uterine and intestinal rupture). Disease of unknown aetiology with fibrotic thickening and muscular hyperplasia affecting the tunic media of the vessel, more commonly affecting women. It usually affects the renal and carotid arteries but the external iliac artery may also be affected). Angiograms classically show a beaded appearance to the affected vessel (‘chain of lakes’).
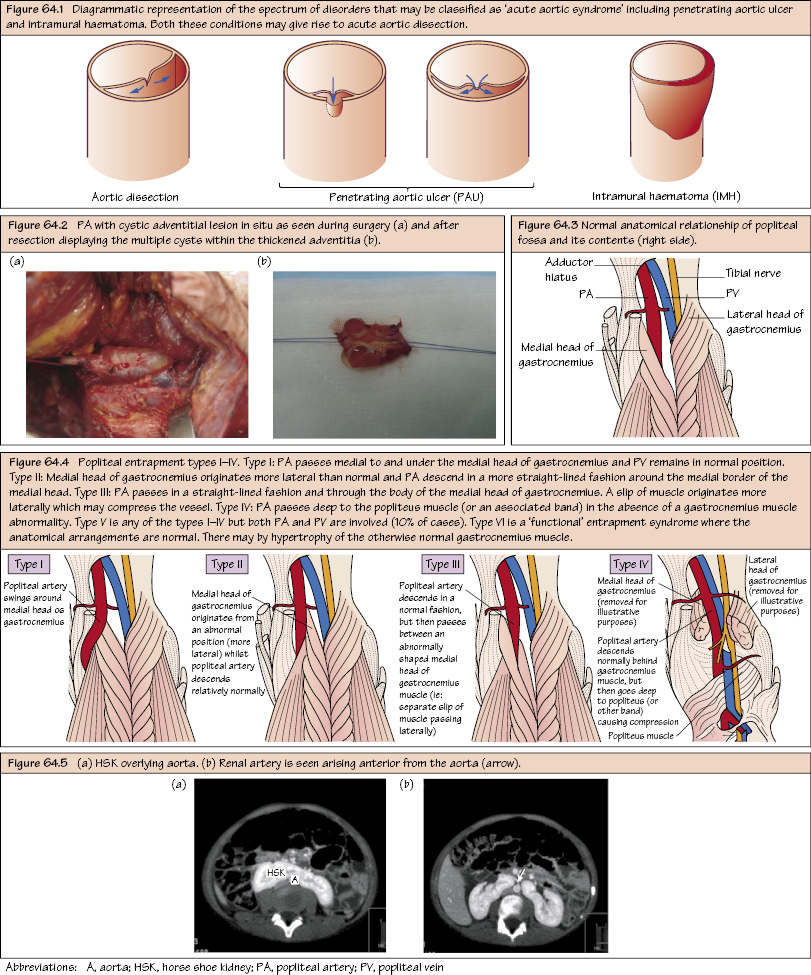
Acute Aortic Syndrome
Arterial Endofibrosis
Buerger’s Disease (Thromboangiitis Obliterans)
Carotid Artery Dissection
Carotid Body Tumour (CBT)
Cockett Syndrome
Cystic Adventitial Disease
Ehlers-Danlos Syndrome
Fibromuscular Dysplasia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


