FIGURE 28-1 Access-site complications and hospital stay in transradial and transfemoral access after PTCA.
Access
Objective | To compare procedural and clinical outcomes of PTCA via the TRA, TBA, or TFA |
Study Population | 900 patients (300 in each group) undergoing PTCA for ACS |
Follow-up | In-hospital and 1 mo |
End Point | Procedural outcomes and MACE (death, MI, CABG, or repeat PTCA) at 1 mo |
Procedural Success Rate/Crossover | TRA → TFA: 20; TBA → TFA: 12; TFA → TRA: 1 |
Main Results (Fig. 28-2) | • Successful coronary cannulation—TRA:TBA:TFA = 93.0%:95.7%:99.7% (P < 0.001) • Major entry site complications—TRA:TBA:TFA = 0%:2.3%:2.0% (P = 0.035) • Entry site complications requiring transfusion—TRA:TBA:TFA = 0%:0.7%:0.7% (P = NS) • RAO: 9 patients (3%) • Similar rates of PTCA success (TRA:TBA:TFA = 88%:88%:90% [P = NS]), procedural and fluoroscopy times, and MACE at 1 mo • No difference in length of hospital stay—TRA: 1.5 ± 2.5 d vs TBA: 1.8 ± 3.8 d vs TFA: 1.8 ± 4.2 d (P = NS) |
Conclusion | Procedural and clinical success of PTCA were similar for the three subgroups, with reduced entry site complications but increased access failure with transradial PTCA |
Reference | Kiemeneij F, Laarman GJ, Odekerken D, et al. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997;29(6):1269–1275. |
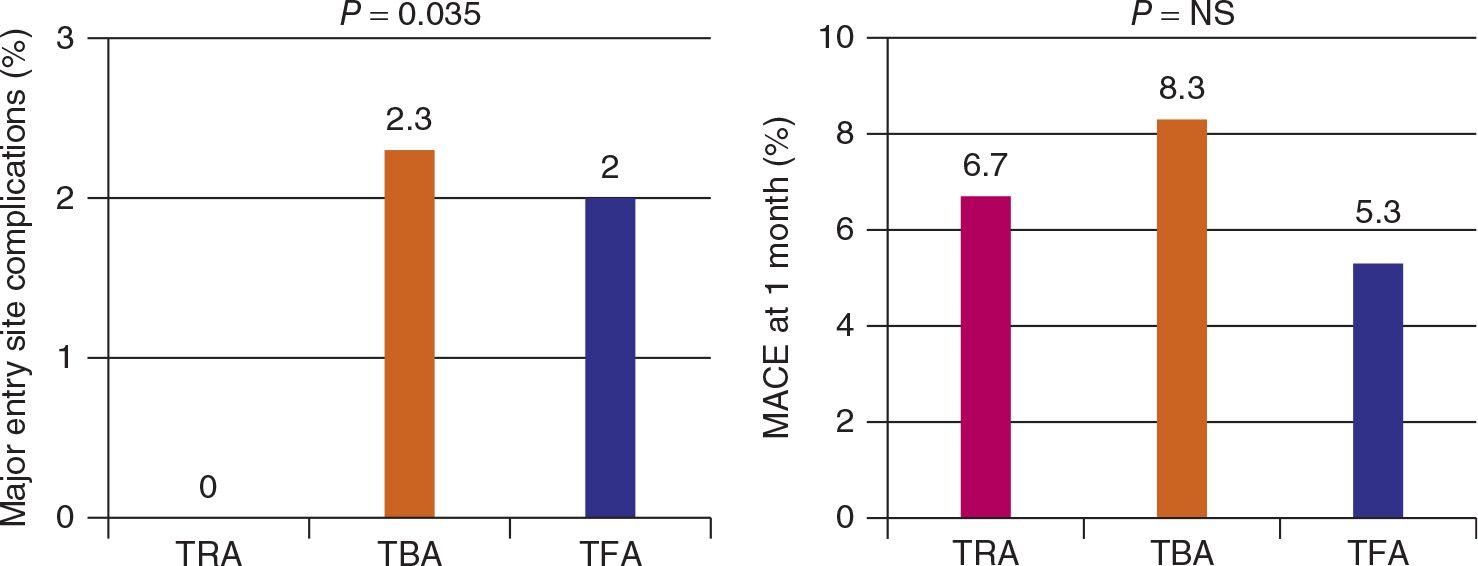
FIGURE 28-2 Major entry site complications and MACE rates in transradial, transbrachial and transfemoral access after PTCA.
Brafe Stent
Objective | To compare procedural outcomes and length of hospitalization times |
Study Population | 150 patients (TRA: 56; TBA: 38; TFA: 56) undergoing PTCA for ACS |
Follow-up | In-hospital and 1 mo |
End Point | Primary-entry site complications (bleeding, hematoma, transfusion, occlusion, surgery) and average hospitalization time post–stent implantation |
Procedural Success Rate/Crossover | TRA → TFA: 1; TBA → TFA: 0; TFA → TRA: 0 |
Main Results (Fig. 28-3) | • Similar entry site complications • Similar in-hospital and 1 month outcomes (death, MI, revascularization, bleeding, and transfusions) • Similar hospitalization time (TBA: 77 ± 36 h vs TFA: 83 ± 33 h vs TRA: 86 ± 39 h; P = NS) • TRA had longer procedural times (TBA: 31.0 ± 10.0 min vs TFA: 42.2 ± 21.8 min vs TRA: 55.8 ± 31.3 min; P ≤ 0.001) |
Conclusion | Procedural and clinical outcomes were similar for all three subgroups, with TRA having longer procedural times |
Reference | Benit E, Missault L, Eeman T, et al. Brachial, radial, or femoral approach for elective Palmaz-Schatz stent implantation: a randomized comparison. Catheter Cardiovasc Diagn. 1997;41(2):124–130. |
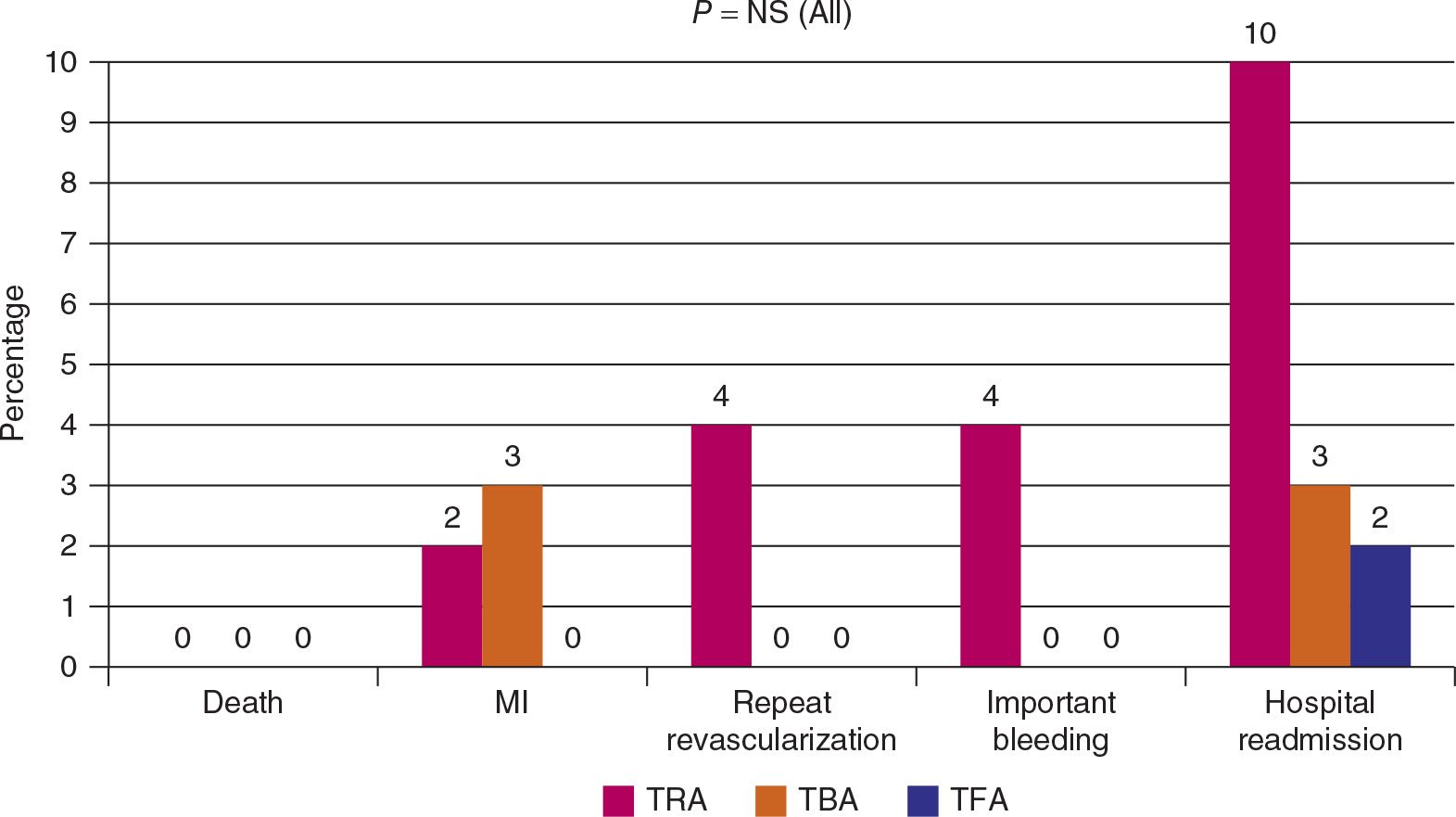
FIGURE 28-3 Death, MI, repeat revascularization, bleeding and hospital readmission rates in transradial, transbrachial and transfemoral access after PTCA.
Stenting in Acute Coronary Syndromes: A Comparison of Radial versus Femoral Access Sites
Objective | To compare TRA with TRF for coronary stenting in patients with ACS |
Study Population | 142 patients (TRA: 74; TRF: 68) undergoing PTCA for ACS |
Follow-up | In-hospital |
End Point | Hospital procedural and clinical outcomes |
Procedural Success Rate/Crossover | TRA → TFA: 9; TFA → TRA: 0 |
Main Results (Fig. 28-4) | • Similar primary PTCA success rates (96%), death, MI, and CABG • TRA had fewer access site complications (TRA: 0% vs TRF: 4%; P < 0.01) • TRA had lower total hospital length of stay (TRA: 3.0 ± 0.3 d vs TRF: 4.5 ± 0.5 d; P < 0.01) and total hospital charge (reduction of 15%; P < 0.01) |
Conclusion | Coronary stenting from the radial approach is efficacious in patients with ACSs. Access site bleeding complications are reduced, and early ambulation results in a shorter hospital length of stay |
Reference | Mann T, Cubeddu G, Bowen J, et al. Stenting in acute coronary syndromes: a comparison of radial versus femoral access sites. J Am Coll Cardiol. 1998;32(3):572–576. |
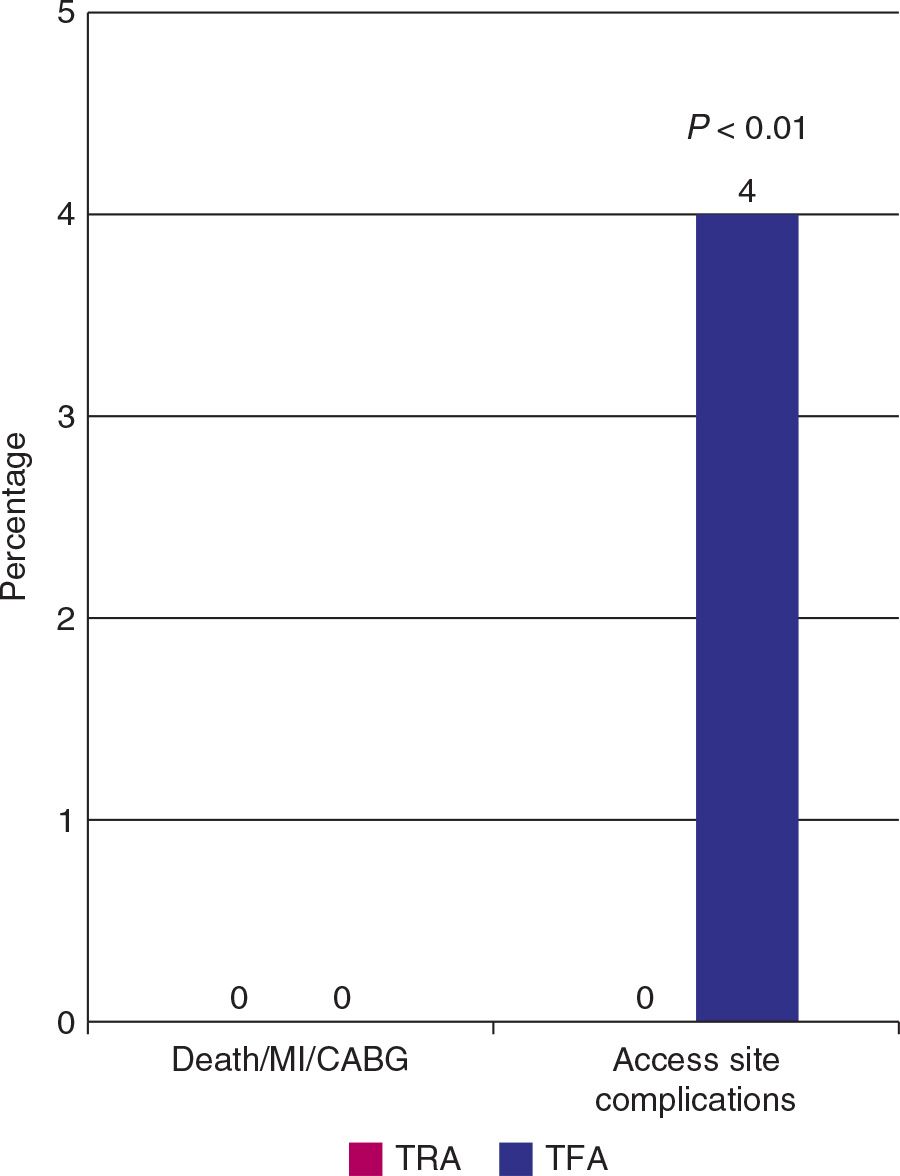
FIGURE 28-4 Death, MI, CABG and access site complications, in patients undergoing PTCA for ACS, using the transradial and transfemoral access.
Effect of Transradial Access on Quality of Life and Cost of Cardiac Catheterization: A Randomized Comparison
Objective | To assess QOL and costs of the TRA and TFA |
Study Population | 200 patients (TRA: 101 vs TRF: 99) undergoing catheterization |
Follow-up | In-hospital and 1 wk |
End Point | QOL (acute SF-36) measurements and hospitalization costs |
Procedural Success Rate/Crossover | TRA → TFA: 2; TFA → TRA: 1 |
Main Results (Fig. 28-5) | • TFA group had longer procedural times (47 ± 2.7 min vs 31. ± 1.7 min; P < 0.001 • Measures of body and back pain as well as walking ability favored TRA on the first day and 1-wk follow-up (P < 0.05) • TRA significantly reduced duration of hospital stay (10.4 [8.3–22.7] h vs 3.6 [3.0–4.6] h; P < 0.0001) and total hospital costs (13%) |
Conclusion | Among patients undergoing diagnostic cardiac catheterization, TRA leads to improved QOL after the procedure and reduced hospital costs |
Reference | Cooper CJ, El-Shiekh RA, Cohen DJ, et al. Effect of transradial access on quality of life and cost of cardiac catheterization: a randomized comparison. Am Heart J. 1999;138(3 pt 1):430–436. |
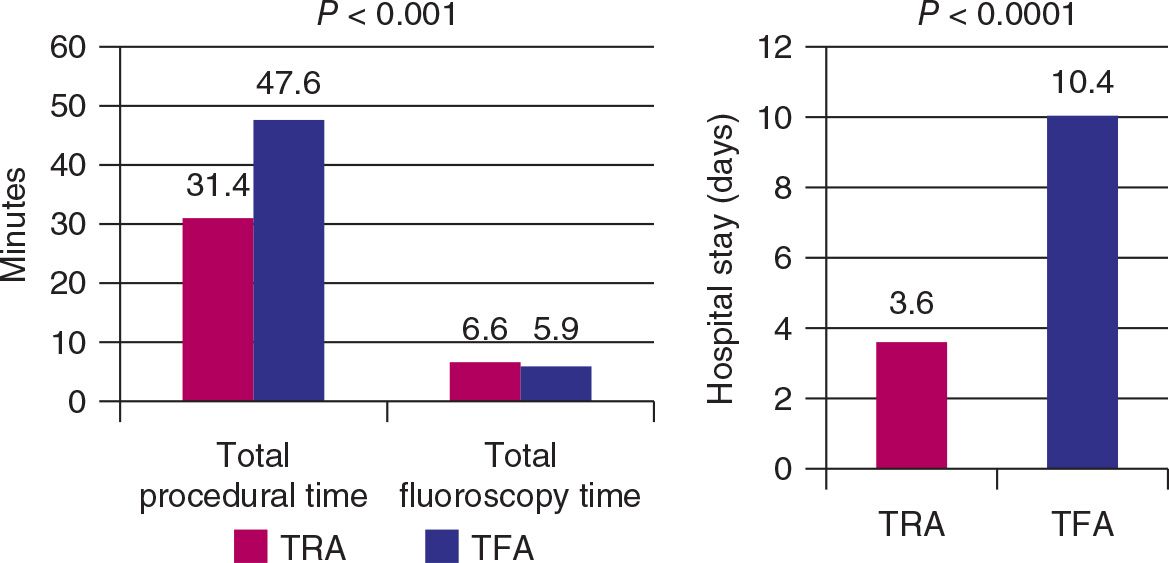
FIGURE 28-5 Total procedural and fluoroscopy time and hospital stay, in patients undergoing coronary angiogrpahy, using the transradial and transfemoral access.
CARAFE
Objective | To compare TRA and TFA with experienced radial operators |
Study Population | 210 (TRA: 140 vs TFA: 70) undergoing PTCA |
Follow-up | In-hospital |
End Point | Procedural and cost outcomes |
Procedural Success Rate/Crossover | TRA → TFA: 0; TFA → TRA: 0 |
Main Results (Fig. 28-6)
| • Procedural duration was longer with left TRA (14.2 ± 3.3 min; P < 0.05) than with right TRA (12.4 ± 5.8 min) and TFA (11.2 ± 3.3 min) • X-ray exposure was shorter in the femoral group (3.1 ± 1.7 min) than in both radial groups (right: 3.8 ± 2.2 min; left: 4.2 ± 1.7 min) • Higher comfort grade and preference for TRA • Major complications (requiring prolonged hospitalization) were more in TFA than in TRA (3% vs 0%) • Longer hospitalization in TFA (42.0 ± 44.8 h vs 31.4 ± 22.5 h; P < 0.05), causing higher hospitalization fees (P < 0.03) |
Conclusion | After an initial learning period, TRA can be performed with a high success rate and a low complication rate. It is associated with a slight increase in procedural and fluoroscopy times, but permits earlier ambulation and discharge, improves patient comfort, and reduces costs |
Reference | Louvard Y, Lefèvre T, Allain A, et al. Coronary angiography through the radial or the femoral approach: The CARAFE study. Catheter Cardiovasc Interv. 2001;52(2):181–187. |
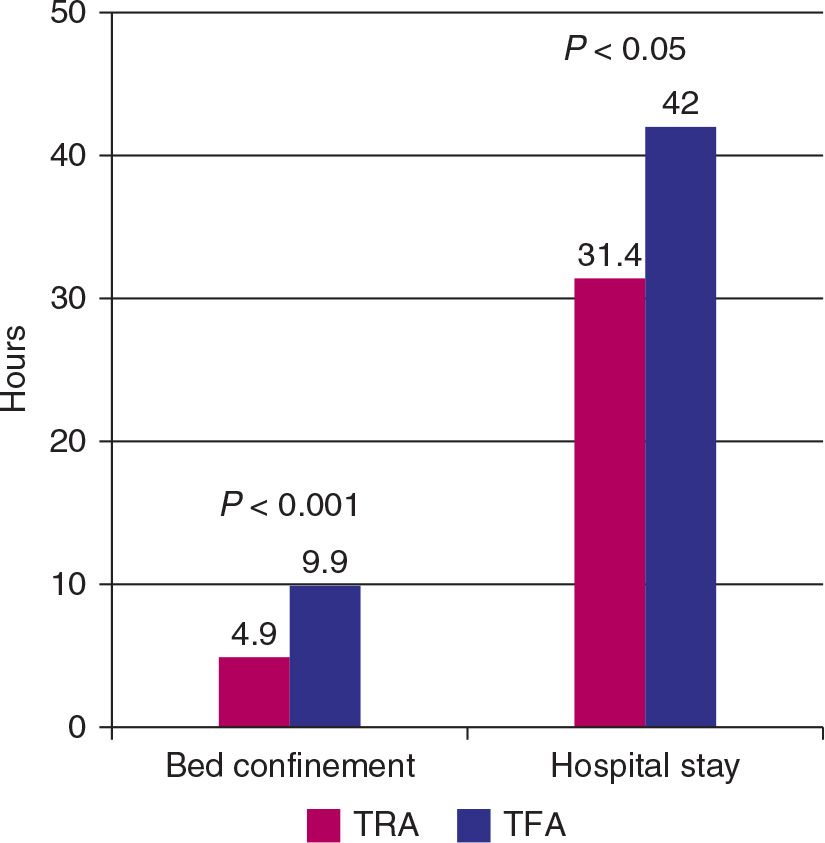
FIGURE 28-6 Bed confinement time and hospital stay, in patients undergoing PTCA, using the transradial and transfemoral access.
TEMPURA
Objective | To compare the MACE between TRA and TFA |
Study Population | 149 patients (TRA: 77 vs TFA: 72) with STEMI |
Follow-up | In-hospital and 9 mo |
End Point | In-hospital and 9 mo MACE (repeat MI, TLR, and death) |
Procedural Success Rate/Crossover | TRA → TFA: 0; TFA → TRA: 1 |
Main Results (Fig. 28-7) | • Similar fluoroscopy times but TRA had shorter procedural times (44 ± 18 min vs 51 ± 21 min; P = 0.033) • Similar MACE, length and cost for hospital admission |
Conclusion | In selected patients with AMI, PCI by TRA is feasible as compared to TFA |
Reference | Saito S, Tanaka S, Hiroe Y, et al. Comparative study on transradial approach vs. transfemoral approach in primary stent implantation for patients with acute myocardial infarction: results of the TEst for Myocardial infarction by Prospective Unicenter Randomization for Access sites (TEMPURA) trial. Catheter Cardiovasc Interv. 2003;59(1):26–33. |
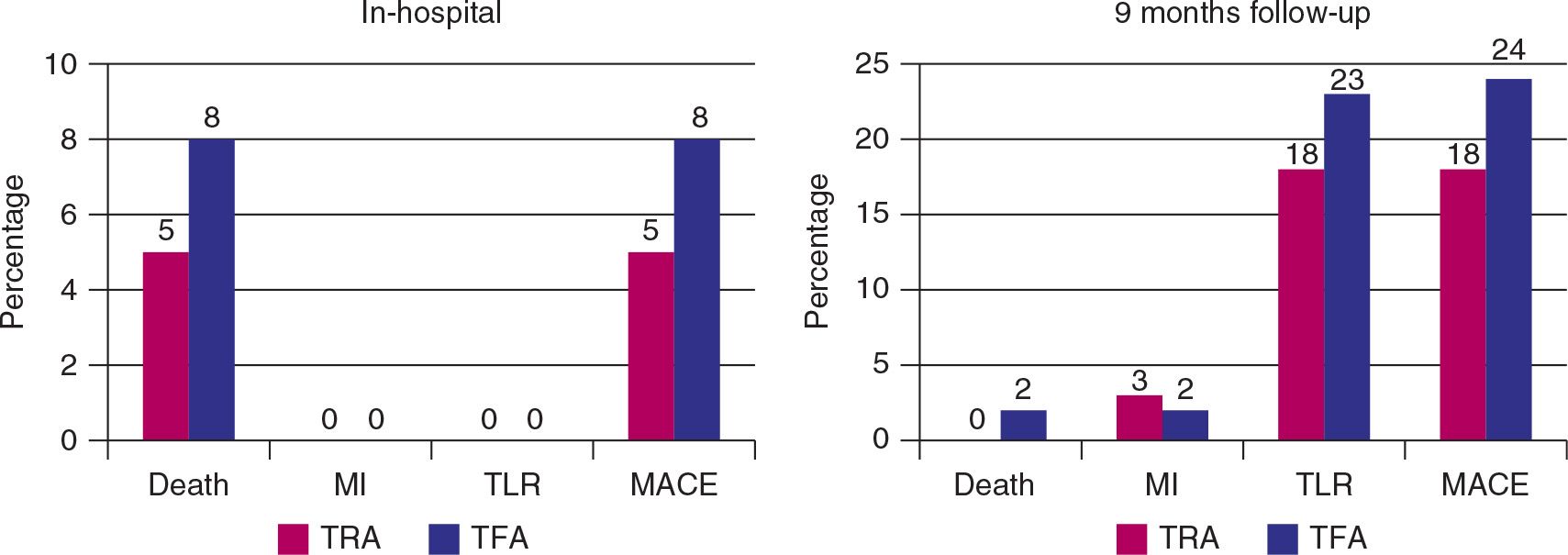
FIGURE 28-7 In-hospital MACE rates and at 9 months follow-up, in patients with STEMI undergoing PCI, using the in transradial and transfemoral access.
OCTOPLUS
Objective | To compare the incidence of significant vascular complications delaying hospital discharge in patients older than 80 yr |
Study Population | 377 patients (TRA: 192 vs TFA: 185) undergoing PCI for ACS or STEMI |
Follow-up | In-hospital |
End Point | Vascular complications |
Procedural Success Rate/Crossover | TRA → TFA: 2; TFA → TRA: 0 |
Main Results (Fig. 28-8) | • Similar procedural success rates (96%) • TRA had longer fluoroscopy (4.5 ± 3.7 min vs 6.0 ± 4.4 min) and procedural times (15.9 ± 9.5 min vs radial 18.5 ± 10.5 min) during coronary angiography, with no differences observed during PCI • RAO: 5% • Vascular complications were significantly fewer in TRA (1.6% vs 6.5%; P = 0.03) |
Conclusion | In octogenarians, the incidence of vascular complications was significantly less in the TRA group, with no reduction of efficacy |
Reference | Louvard Y, Benamer H, Garot P, et al. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am J Cardiol. 2004;94(9):1177–1180. |
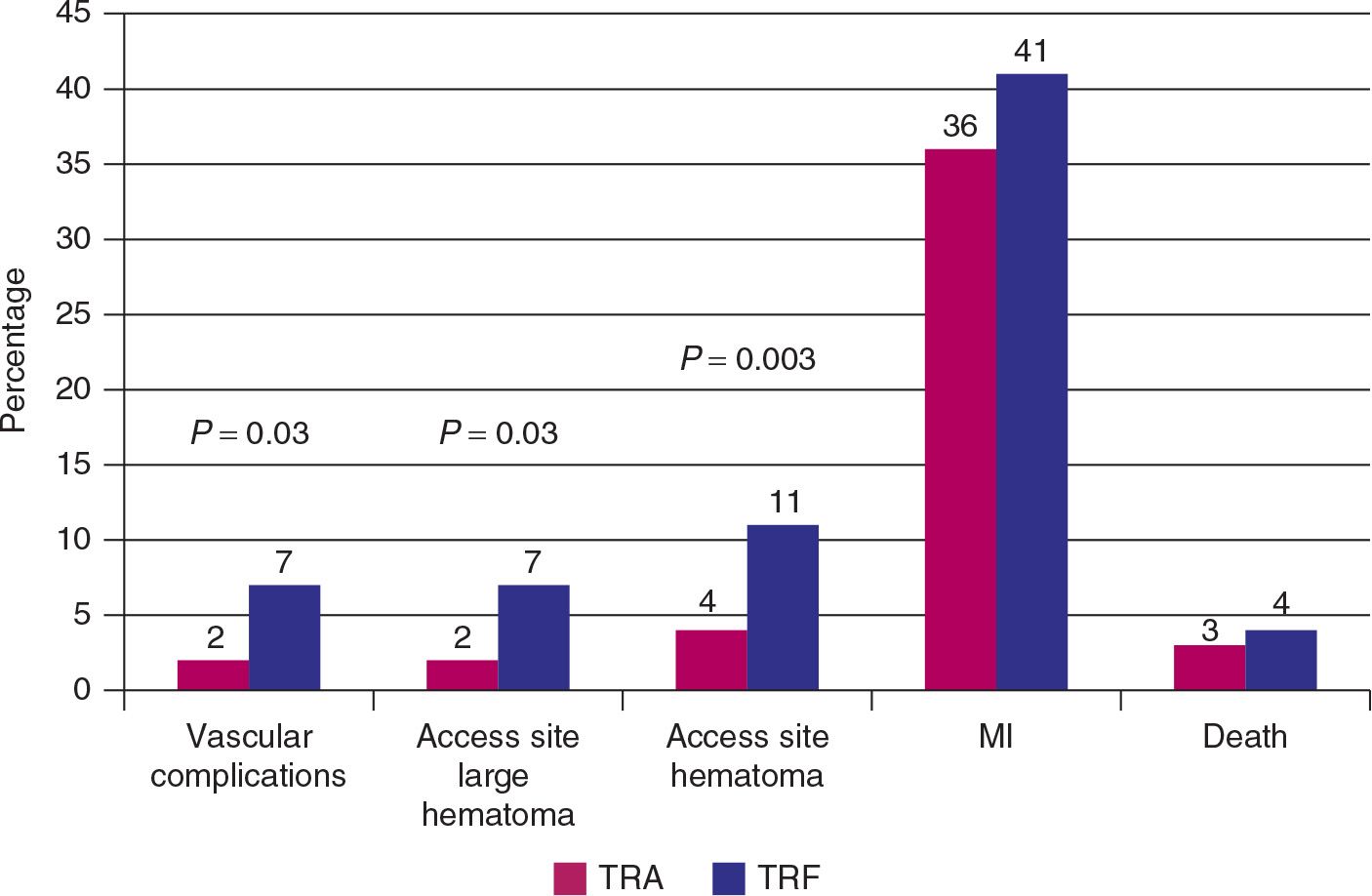
FIGURE 28-8 Vascular complications, MI and death rates, in patients >80 years old with ACS and undergoing PCI, using the transradial and transfemoral access.
OUTCLAS
Objective | To test the safety and feasibility of outpatient coronary angioplasty |
Study Population | 644 patients (322 in each group) undergoing PCI for SA or UA |
Follow-up | In-hospital and 1 mo |
End Point | MACE (cardiac death/MI/TVR), vascular complications, and major bleeding (>2 mmol/L drop) |
Procedural Success Rate/Crossover | NA |
Main Results (Fig. 28-9)
| • Similar PCI success rates (96% vs 97%; P = NS) • Similar in-hospital and 1-mo rates of cardiac death/MI/TVR • TFA group had a higher number of patients with significant in-hospital bleeding (14.3% vs 6.3%), but no difference in transfusion rates was observed • RAO: 0.3% • A larger proportion (61% vs 55%; P = NS) of TRA patients could undergo same-day discharge (major bleeding was the sole reason for discharge delay in the TFA group) |
Conclusion | PCI on an outpatient basis, performed via TRA or TFA, is safe and feasible in a considerable portion of a routine PCI population |
Reference | Slagboom T, Kiemeneij F, Laarman GJ, et al. Outpatient coronary angioplasty: feasible and safe. Catheter Cardiovasc Interv. 2005;64(4):421–427. |
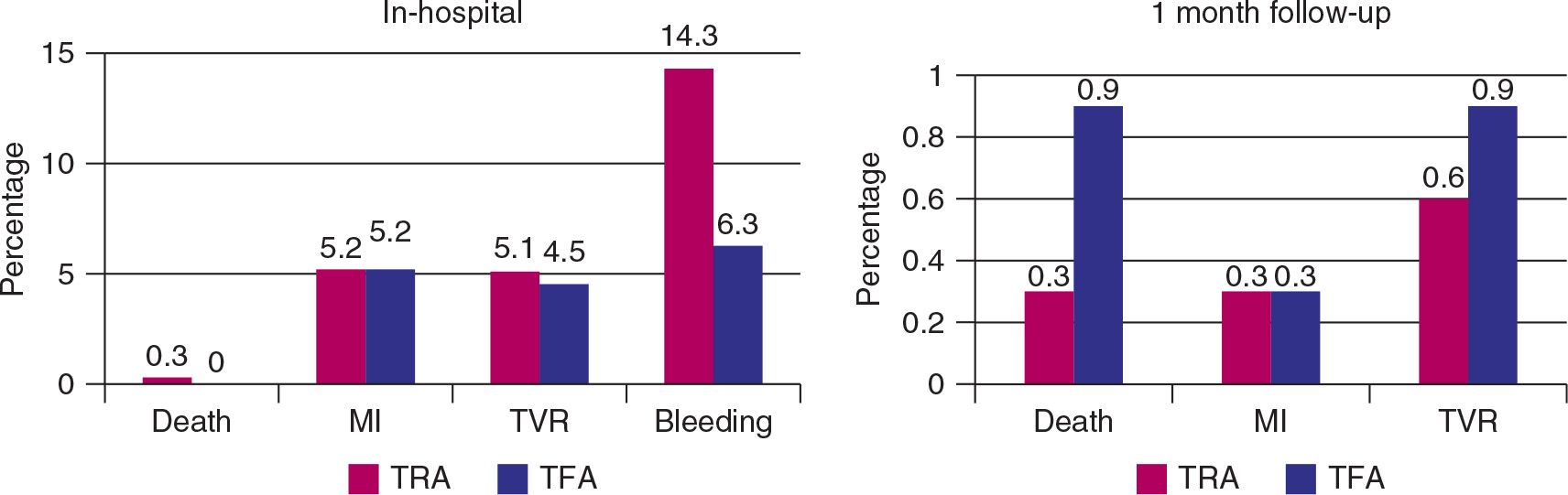
FIGURE 28-9 In-hospital MACE and bleeding rates and MACE rates at 1 month follow-up, in patients with stable or unstable angina undergoing PCI, using the transradial and transfemoral access.
RADIAL-AMI
Objective | To compare TRA with TFA for coronary stenting in patients with STEMI (primary and rescue) |
Study Population | 50 patients (25 in each) undergoing PCI for STEMI with the use of thrombolytics and/or glycoprotein IIb/IIIa inhibitors |
Follow-up | In-hospital and 1 mo |
End Point | Perfusion time, major bleeding and access site bleeding |
Procedural Success Rate/Crossover | TRA → TFA: 1; TFA → TRA: 0 |
Main Results (Fig. 28-10)
| • Similar PCI success rates (87% vs 88%) • Only difference in time intervals was greater time in TRA group from local anesthesia to first balloon inflation (32 min [26–38] vs 26 min [22–33]; P = 0.04) • No difference in fluoroscopy and procedural times • RAO: 9% • Similar death/MI/TVR at 30 d and for QOL score (walking and back pain) • No patient from either group experienced major bleeding or required blood transfusion |
Conclusion | Primary and rescue PCI can be performed, with high success rates, using either TRA or TFA. Major bleeding and vascular complications were infrequent with either access site despite the high rates of thrombolysis and glycoprotein IIb/IIIa inhibitors use |
Reference | Cantor WJ, Puley G, Natarajan MK, et al. Radial versus femoral access for emergent percutaneous coronary intervention with adjunct glycoprotein IIb/IIIa inhibition in acute myocardial infarction-the RADIAL-AMI pilot randomized trial. Am Heart J. 2005;150(3):543–549. |
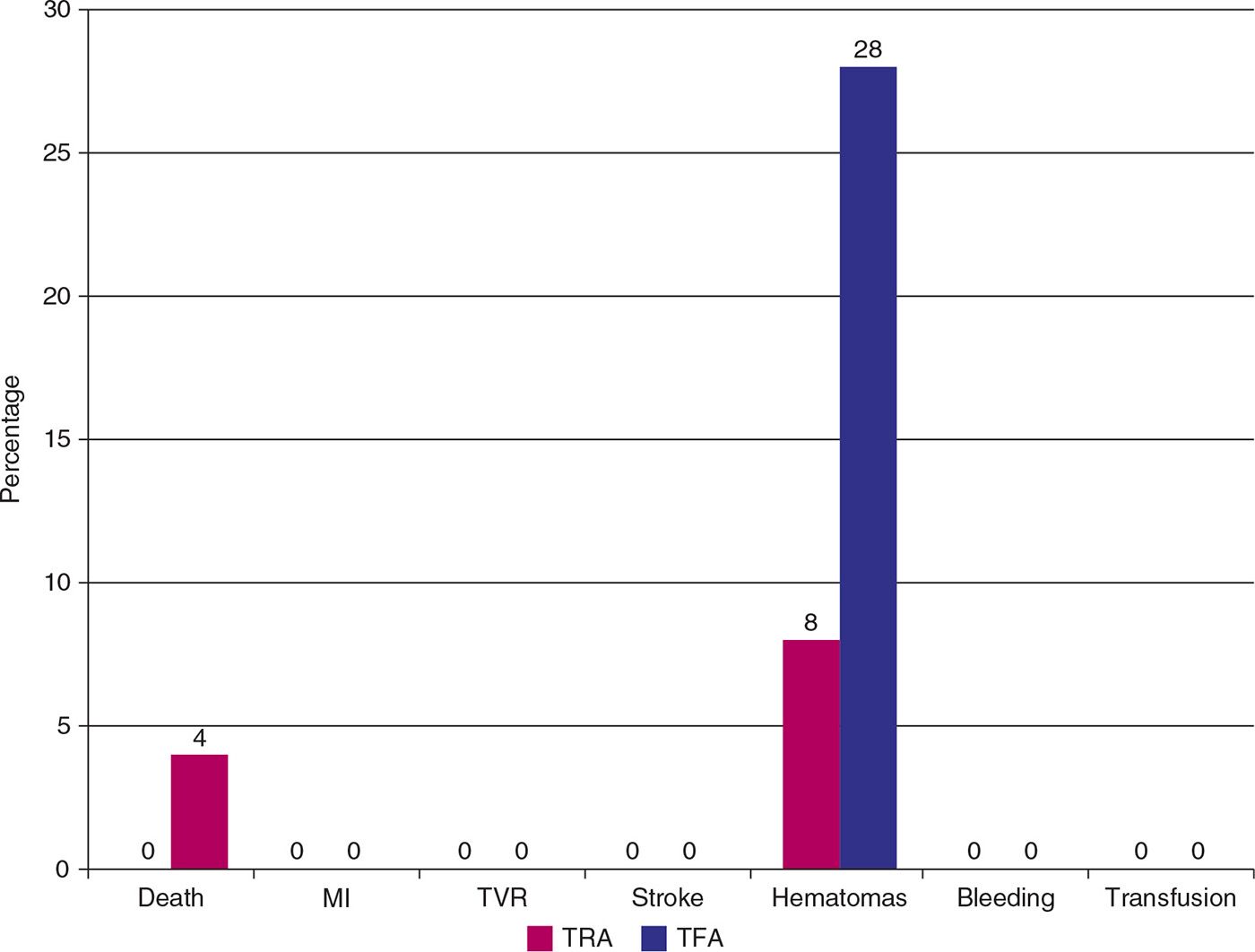
FIGURE 28-10 Thirty days clinical outcomes (MACE, procedural complications and bleeding) in STEMI patients undergoing transradial and transfemoral PCI.
Randomized Comparison of Operator Radiation Exposure during Coronary Angiography and Intervention by Radial and Femoral Approaches
Objective | To evaluate whether significant differences in operator radiation exposure can be expected in the current era during radial coronary procedures |
Study Population | 297 patients (TRA → 146; TFA → 151) who underwent simple coronary angiography or PCI in one noncomplicated single epicardial vessel (no left ventriculogram or aortogram and no bypass grafts) |
Follow-up | In-hospital |
End Point | Fluoroscopy time and radiation measurements |
Main Results (Fig. 28-11) | • Fluoroscopy time was 18% (P < 0.001) longer with TRA angiographies and 10% (P 5 NS) longer with TRA PCI • DAP was 15% (P < 0.05) higher with TRA angiographies but did not increase with TRA PCI • Operator radiation exposure was 100% (P < 0.001) higher with TRA angiographies and 51% (P < 0.05) higher with TRA PCI |
Conclusion | TRA, compared to TFA, is burdened with an increase in operator radiation dose |
Reference | Lange HW, Von Boetticher H. Randomized comparison of operator radiation exposure during coronary angiography and intervention by radial and femoral approach. Catheter Cardiovasc Interv. 2006;67:12–16. |
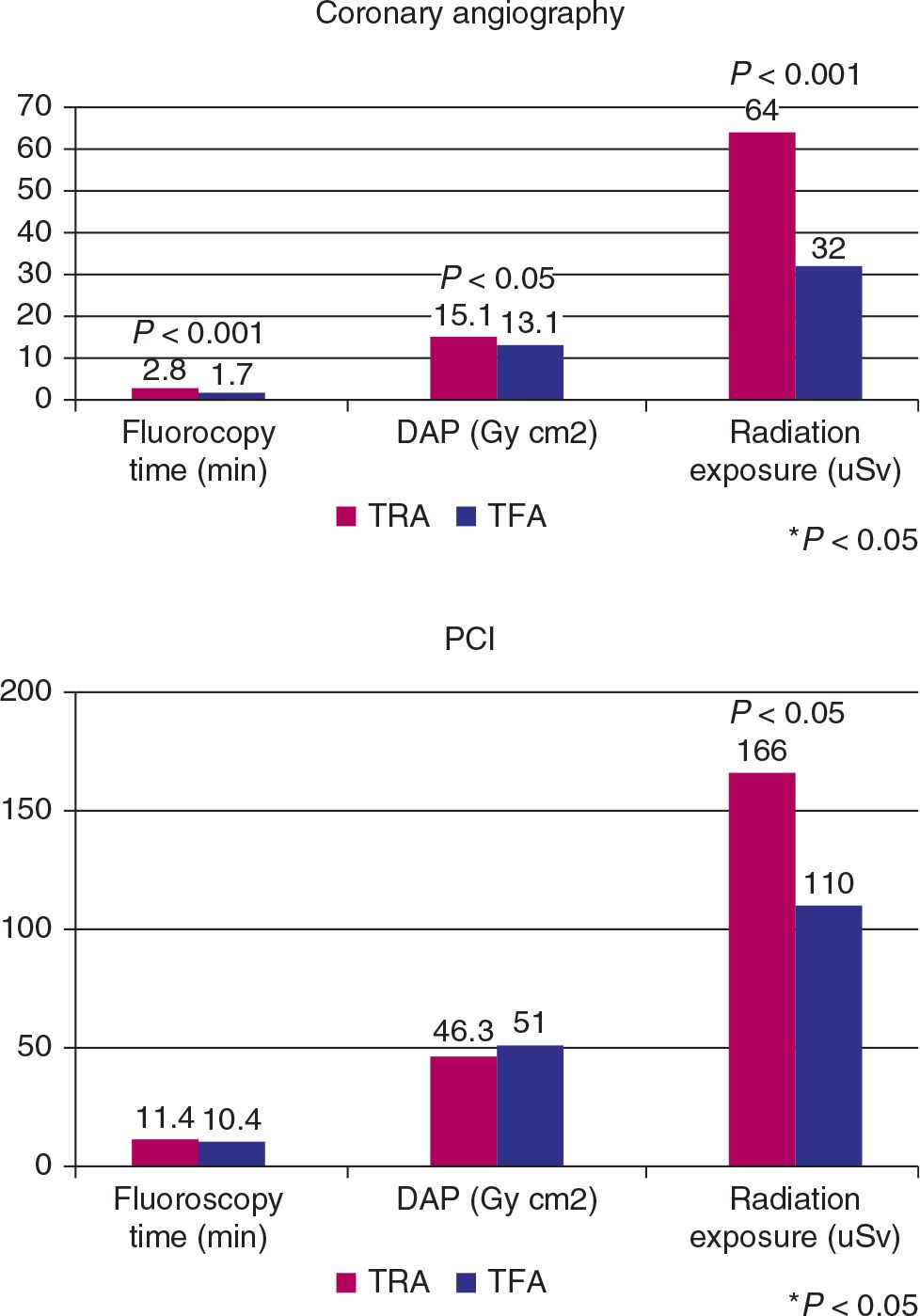
FIGURE 28-11 Fluoroscopy time, DAP and operator radiation exposure during coronary angiography and PCI in transradial and transfemoral access.
Safety and Feasibility of Emergent Percutaneous Coronary Intervention with the Transradial Access in Patients with Acute Myocardial Infarction
Objective | To study the safety and feasibility of TRA in STEMI |
Study Population | 370 patients (TRA: 184 vs TFA: 186) with STEMI |
Follow-up | In-hospital |
End Point | Procedural and hospital outcomes |
Procedural Success Rate/Crossover | TRA → TFA: 3; TFA → TRA: 2 |
Main Results (Fig. 28-12) | • Similar PCI success rates (95% vs 94%) • Similar total procedural times (56.2 ± 12.1 min vs 54.8 ± 15.1 min; P 5 NS) • Vascular access site and postprocedure complications occurred less in the TRA group (local hematoma: 4% vs 1%, P < 0.05; vagus reflex: 8% vs 0%, P < 0.01; low back pain: 4% vs 0%, P < 0.05) |
Conclusion | TRA, compared to TFA, may represent a safer technique for AMI, with similar results and a trend toward fewer local vascular complications |
Reference | Li WM, Li Y, Zhao JY, et al. Safety and feasibility of emergent percutaneous coronary intervention with the transradial access in patients with acute myocardial infarction. Chin Med J (Engl). 2007;120(7):598–600. |
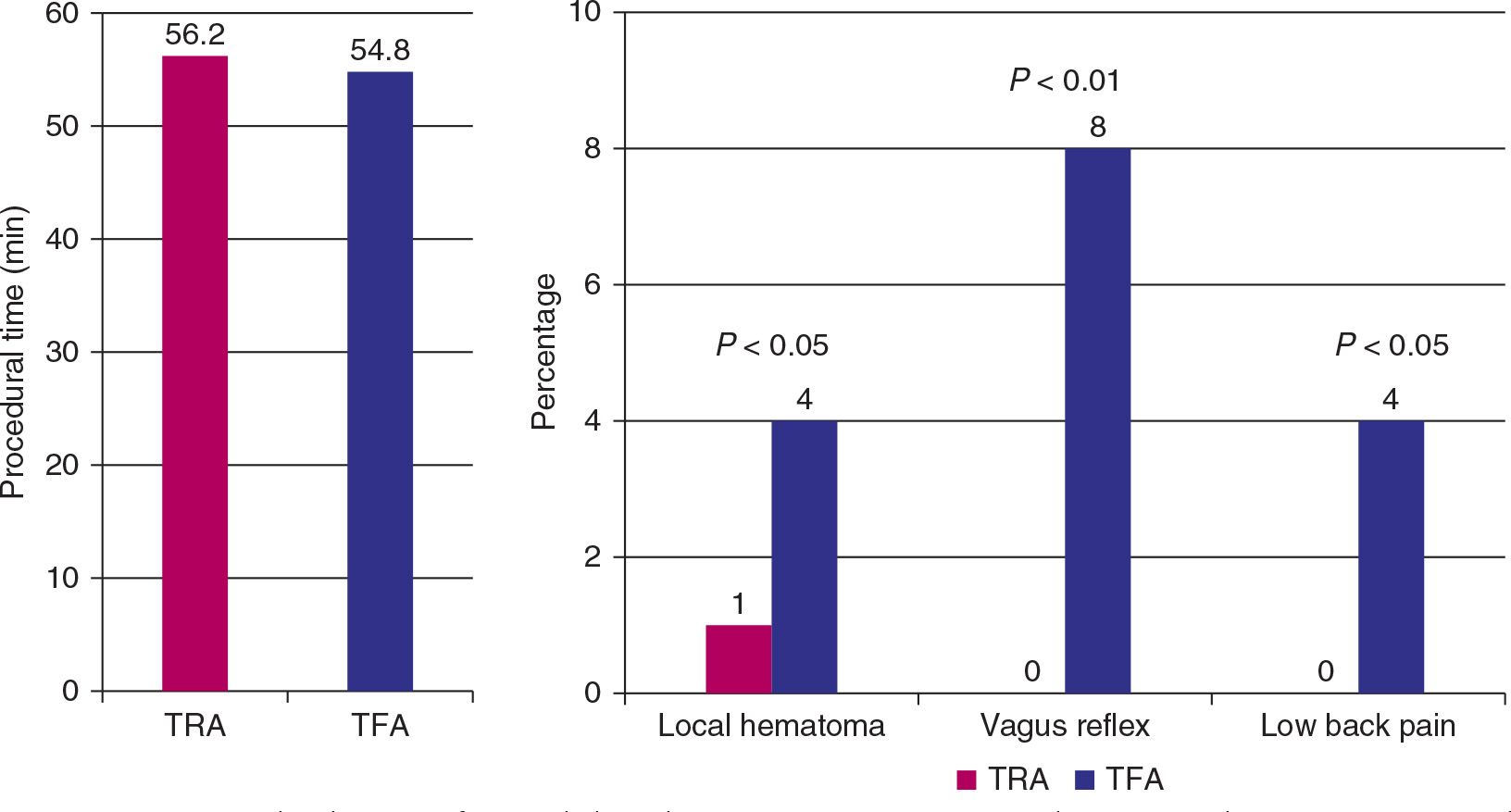
FIGURE 28-12 Procedural time, safety and clinical parameters, in patients with STEMI undergoing PCI, using the transradial and transfemoral access.
FARMI
Objective | To compare bleeding complications and PCI results in patients treated by TRA and TFA for STEMI (primary, facilitated, and rescue) using abciximab |
Study Population | 114 patients (57 in each) with STEMI undergoing PCI |
Follow-up | In-hospital |
End Point | Bleeding and PCI outcomes |
Procedural Success Rate/Crossover | TRA → TFA: 7; TFA → TRA: 1 |
Main Results | • Similar PCI success rates (TRA: 91% vs TFA: 97%) • TRA group had longer mean fluoroscopy times (13 ± 9 min vs 8 ± 6 min; P < 0.01), but no difference was seen in mean PCI times (28 ± 14 min vs 26 ± 18 min; P 5 0.72) • The delay between PCI and ambulation was lower in TRA group (22 ± 9 h vs 42 ± 27 h; P < 0.001), but this did not affect duration of hospitalization (7.2 ± 0.5 d vs 7.5 ± 0.4 d; P 5 0.59) • Similar in-hospital death, TIMI minor/major bleeding, and transfusion rates • Fewer peripheral artery complications (hematoma and ecchymosis) in TRA group (14% vs 35%; P 5 0.014) |
Conclusion (Fig. 28-13) | TRA lowered peripheral arterial complication rates and allowed earlier ambulation in patients with STEMI treated with abciximab |
Reference | Brasselet C, Tassan S, Nazeyrollas P, et al. Randomized comparison of femoral versus radial approach for percutaneous coronary intervention using abciximab in acute myocardial infarction: results of the FARMI trial. Heart. 2007;93(12):1556–1561. |
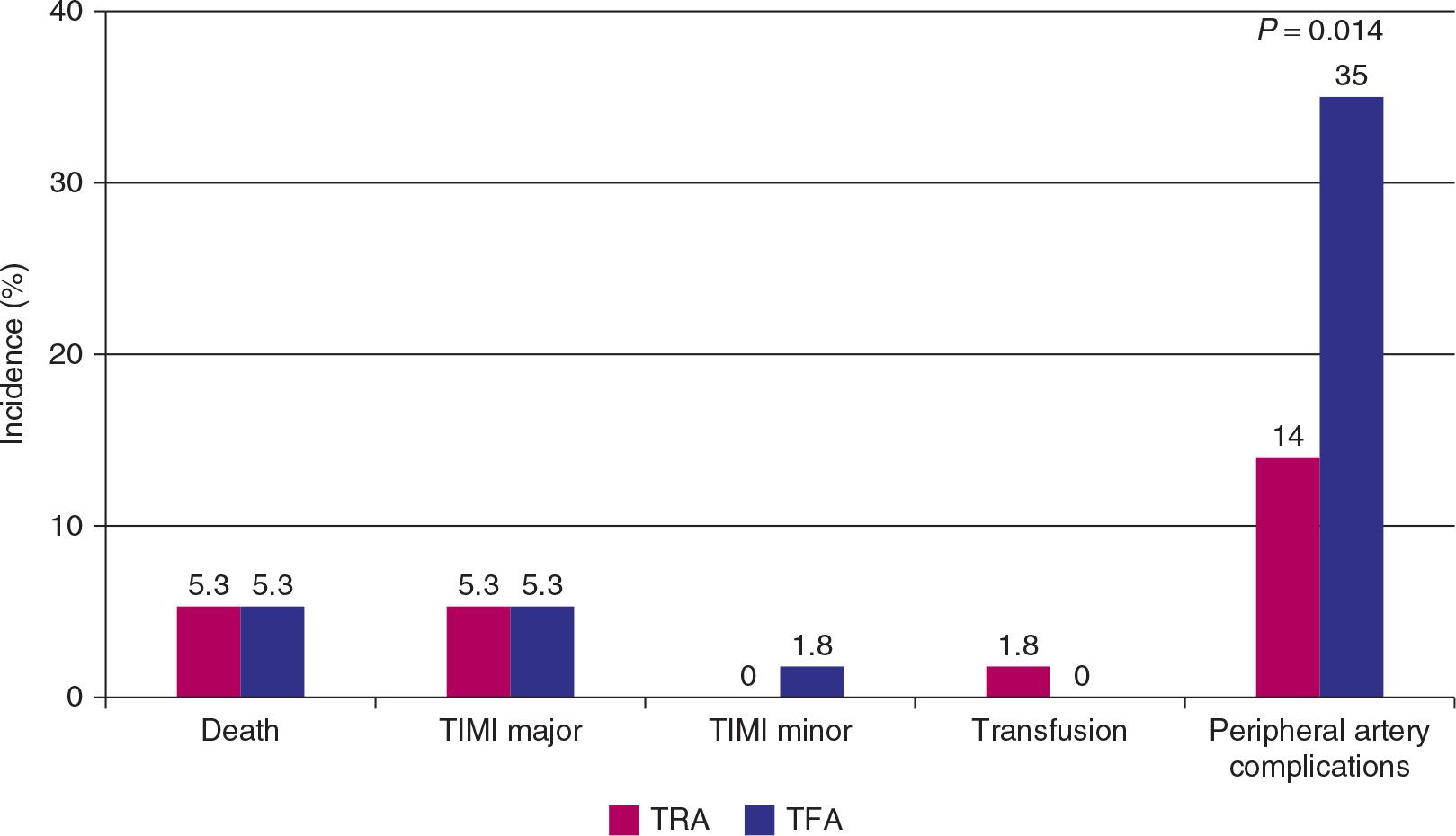
FIGURE 28-13 Death, bleeding and safety outcomes, in STEMI patients undergoing PCI, using the transradial and transfemoral access.
Transradial versus Transfemoral Approach for Coronary Angiography and Intervention in Patients Older Than 75 years
Objective | To determine success rates, procedural data, and complication rates of TRA vs TFA in patients .75 yr |
Study Population | 307 patients (TRA: 152 vs TFA: 155) with ACS undergoing PCI |
Follow-up | In-hospital |
End Point | Success rate, major adverse events (death, periprocedural MI, stroke, or vascular access complications [bleeding, aneurysms, arteriovenous fistulae] requiring intervention), and minor adverse events (symptomatic bleeding requiring no intervention) |



