Radiographic Examinations
PLEURAL EFFUSIONS
Typical Arrangement of Free Pleural Fluid
Two main factors influence the distribution of free fluid in the pleural space. First, the pleural fluid accumulates in the most dependent part of the thoracic cavity because the lung is less dense than pleural fluid. In essence, the lung floats in the pleural fluid. Second, the lobes of the lung maintain their traditional shape at all stages of collapse owing to their elastic recoil (1). The shape of a lobe when it is partially or completely collapsed is a miniature replica of its shape when fully distended.
Bearing in mind that the distribution of fluid within the free pleural space obeys the law of gravity and that the lung maintains its shape when compressed, it is easy to predict the distribution of excess pleural fluid. The fluid first gravitates to the base of the hemithorax and comes to rest between the inferior surface of the lung and the diaphragm, particularly posteriorly, where the pleural sinus is the most inferior. As more fluid accumulates, the fluid spills out into the costophrenic sinuses posteriorly, laterally, and anteriorly. Additional fluid spreads upward in a mantle-like manner around the convexity of the lung and gradually tapers as it assumes a higher position in the thorax.
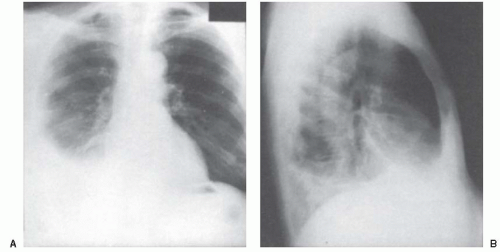
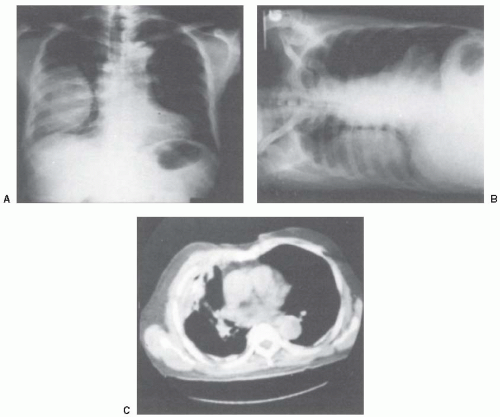
On the basis of this pattern of fluid accumulation, the typical radiographic appearance of a pleural effusion of moderate size (1,000 mL) is as follows. In the posteroanterior projection (Fig. 6.1A), the lateral costophrenic angle is obliterated. The density of the fluid is high laterally and curves gently downward and medially with a smooth, meniscus-shaped upper border to terminate at the mediastinum. The layer of fluid is narrower at the mediastinal border than at the costal border; the reason for this difference is that the mediastinal surface of the lower lobe of the lung possesses less elastic recoil because it is fixed at the hilum and pulmonary ligament (1). In the lateral projection (Fig. 6.1B), the upper surface of the fluid density is semicircular, high anteriorly and posteriorly, and curving smoothly downward to its lowest point approximately midway between the sternum and the posterior chest wall.
Frequently, a “middle lobe step” is observed on the lateral radiograph (Fig. 6.1B). The explanation for the middle lobe step is that as pleural fluid accumulates, the first affected lobe is the lower lobe because it is the most dependent. Therefore, it starts to shrink and float but maintains its shape. The middle lobe is unaffected and maintains its full volume. Accordingly, the result is a shrunken lower lobe with a middle lobe that retains its usual size. Radiographically, the fluid is mostly in the posterior part of the chest (Fig. 6.1B).
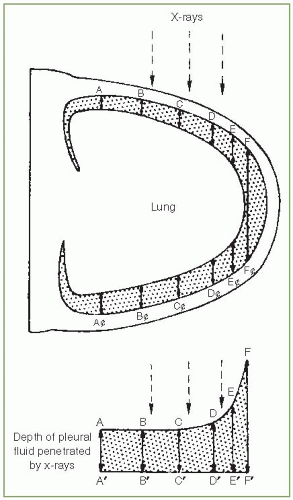
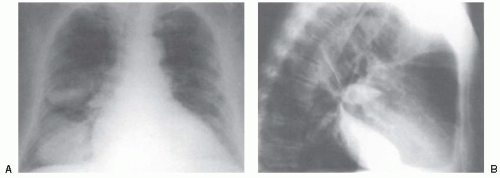
On the basis of the radiologic appearance, one might surmise that the height of the pleural fluid is greater laterally. The true upper limit of pleural fluid, however, is usually the same throughout the hemithorax (2). The meniscus shape is seen because the layer of fluid is of insufficient depth to cast a discernible shadow when viewed en face (Fig. 6.2).
Radiologic Signs
With the patient in the upright position, fluid first accumulates between the inferior surface of the lower lobe and the diaphragm. If the amount of fluid is small (approximately 75 mL), it may occupy only this position without spilling into the costophrenic sinuses. With this small amount of fluid, the normal configuration of the diaphragm is maintained, and the
chest radiograph does not indicate that pleural fluid is present. When more fluid accumulates, it spills over into the posterior costophrenic angle and obliterates that sinus as viewed in the lateral projection (Fig. 6.1B). The normally sharp posterior costophrenic angle is obliterated by a shallow, homogeneous shadow whose upper surface is meniscus shaped. The pleural line up the posterior thoracic wall is also widened. Anytime the posterior costophrenic angle is obliterated or the posterior part of one or both diaphragms is obscured, the presence of pleural fluid is suggested and further diagnostic efforts should be made. Moreover, if both posterior costophrenic angles are clear and sharp, the presence of clinically significant amounts of free pleural fluid can be nearly excluded.
chest radiograph does not indicate that pleural fluid is present. When more fluid accumulates, it spills over into the posterior costophrenic angle and obliterates that sinus as viewed in the lateral projection (Fig. 6.1B). The normally sharp posterior costophrenic angle is obliterated by a shallow, homogeneous shadow whose upper surface is meniscus shaped. The pleural line up the posterior thoracic wall is also widened. Anytime the posterior costophrenic angle is obliterated or the posterior part of one or both diaphragms is obscured, the presence of pleural fluid is suggested and further diagnostic efforts should be made. Moreover, if both posterior costophrenic angles are clear and sharp, the presence of clinically significant amounts of free pleural fluid can be nearly excluded.
Increasing amounts of fluid blunt the lateral costophrenic angle of the posteroanterior (PA) radiograph. Collins et al. (3) injected fluid into the pleural spaces of upright cadavers. They demonstrated that at least 175 mL pleural fluid had to be injected before the lateral costophrenic angle was blunted and, in some cases, more than 500 mL pleural fluid could be present without blunting the lateral costophrenic angle. As more fluid accumulates, the entire outline of the diaphragm on the affected side is lost, and the fluid extends upward around the anterior, lateral, and posterior thoracic walls. This fluid produces opacification of the lung base and the typical meniscus shape of the fluid, as demonstrated in Figure 6.1.
Subpulmonic or Infrapulmonary Effusions
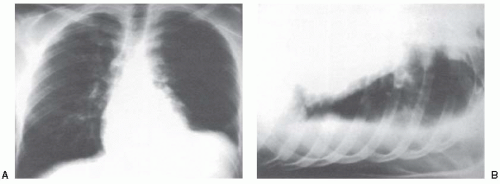
At times, for unknown reasons, substantial amounts of pleural fluid (more than 1,000 mL) can be present and may remain in an infrapulmonary location without spilling into the costophrenic sulci or extending up the chest wall. Such pleural fluid accumulations are called subpulmonic or infrapulmonary pleural effusions (Fig. 6.3). Although the posterior costophrenic angle is usually blunted, at times it is perfectly clear (1).
The following radiologic characteristics are common to most cases of subpulmonic effusions (1), and the presence of one or more of these characteristics should serve as an indication for decubitus examinations to rule out the possibility of a subpulmonic pleural effusion: (a) apparent elevation of one or both diaphragms; (b) in the posteroanterior projection with subpulmonic effusions, the apex of the apparent diaphragm is more lateral than usual, near the junction of the middle third and the lateral third of the diaphragm, rather than at the center of the diaphragm; (c) the apparent diaphragm slopes much more sharply toward the lateral costophrenic angle (Fig. 6.4); (d) if the subpulmonic effusion is on the left side, the lower border of the lung is separated farther
from the gastric air bubble than usual; normally, the top of the left diaphragm on the posteroanterior view is less than 2 cm above the stomach air bubble (4); a separation greater than 2 cm suggests a subpulmonic effusion, but, of course, it can also be due to subdiaphragmatic fluid accumulation; if no gastric air bubble is present, the ingestion of a carbonated beverage by the patient will allow evaluation of this sign; (e) in the lateral projection, the major fissure often bows anteriorly where it meets the convex upper margin of the fluid; a small amount of fluid is usually apparent in the lower end of the major fissure at its junction with the infrapulmonary effusion; and (f) the lower lobe vessels may not be seen below the apparent diaphragmatic border.
from the gastric air bubble than usual; normally, the top of the left diaphragm on the posteroanterior view is less than 2 cm above the stomach air bubble (4); a separation greater than 2 cm suggests a subpulmonic effusion, but, of course, it can also be due to subdiaphragmatic fluid accumulation; if no gastric air bubble is present, the ingestion of a carbonated beverage by the patient will allow evaluation of this sign; (e) in the lateral projection, the major fissure often bows anteriorly where it meets the convex upper margin of the fluid; a small amount of fluid is usually apparent in the lower end of the major fissure at its junction with the infrapulmonary effusion; and (f) the lower lobe vessels may not be seen below the apparent diaphragmatic border.
Diaphragmatic Inversion
At times, the weight of the fluid may cause the diaphragm to become inverted such that its normally convex superior border becomes concave. This inversion occurs much more commonly with effusions on the left, but it can occur with effusions on the right (5). Radiologically, the gastric air bubble is pushed inferiorly, and the superior border of the diaphragm is concave upward rather than convex. When viewed under fluoroscopy, such inverted diaphragms move paradoxically with respiration, rising on inspiration and descending on expiration (6). At times, patients with large left pleural effusions suddenly become dyspneic coincidentally with the development of inversion of the left diaphragm. In such instances, therapeutic thoracentesis is indicated (see Chapter 28). The removal of some of the pleural fluid restores the normal configuration to the diaphragm and rapidly relieves the patient’s symptoms (6).
Supine Position
Until this time, I have only discussed the radiologic characteristics of pleural effusions with the patient in the upright position. Many chest radiographs, however, particularly those in acutely ill patients, are obtained with the patient in the supine position. When the patient is in this position, pleural fluid gravitates to the posterior parts of the thoracic cavity. Because the pleural fluid is spread over a large area, considerable quantities must be present before any radiographic changes are seen. In one study of 117 pleural effusions documented by CT scan, the portable anteroposterior radiograph demonstrated only 66% of the effusions including 57% of small, 71% of moderate, and 91% of large-sized effusions (7). However, in a recent study (8) of 61 patients with parapneumonic effusions, the portable chest radiograph identified 76% of the effusions correctly while the later radiograph identified 87% and the PA identified 81% correctly compared with the CT scan. Most of the patients in whom the pleural effusions were missed had lower lobe infiltrates (8).
The presence of free pleural fluid elicits several signs on the supine radiograph. These signs include blunting of the costophrenic angle, increased homogeneous density superimposed over the lung, loss of the hemidiaphragm silhouette, apical capping, elevation of the hemidiaphragm, decreased visibility of lower lobe vasculature, and accentuation of the minor fissure
(9,10). Some patients with a small-to-moderate-sized pleural effusion have none of these signs. In one study (9), none of these radiologic signs were present in 9 of 16 patients with small effusions (defined as measuring <1.5 cm on the decubitus radiograph) and in 3 of 13 patients with moderate effusions (defined as measuring 1.5-4.5 cm on the decubitus radiograph). In a second study, the supine chest radiograph suggested the presence of pleural fluid in 29 of 30 patients (97%) who had more than 300 mL pleural fluid (11). In this study, increased homogeneous density, blunted costophrenic angle, and loss of a diaphragm silhouette were the most accurate signs in diagnosing a pleural effusion with an accuracy of approximately 80% (11). The increased homogeneous density in most cases with a pleural effusion was limited to the lower one- or two-thirds of the lung field or was more pronounced there (11).
(9,10). Some patients with a small-to-moderate-sized pleural effusion have none of these signs. In one study (9), none of these radiologic signs were present in 9 of 16 patients with small effusions (defined as measuring <1.5 cm on the decubitus radiograph) and in 3 of 13 patients with moderate effusions (defined as measuring 1.5-4.5 cm on the decubitus radiograph). In a second study, the supine chest radiograph suggested the presence of pleural fluid in 29 of 30 patients (97%) who had more than 300 mL pleural fluid (11). In this study, increased homogeneous density, blunted costophrenic angle, and loss of a diaphragm silhouette were the most accurate signs in diagnosing a pleural effusion with an accuracy of approximately 80% (11). The increased homogeneous density in most cases with a pleural effusion was limited to the lower one- or two-thirds of the lung field or was more pronounced there (11).
The earliest sign is blunting of the costophrenic angle (9). Subsequently, increased density of the hemithorax, loss of the hemidiaphragm, and decreased visibility of the lower lobe vasculature occur. Apical capping does occur with pleural effusion, but it does not appear to be related to the size of the pleural effusion (9). Elevation of the hemidiaphragm and accentuation of the minor fissure are insensitive signs in that they occur in a minority of patients and are not related to the size of the effusion (9).
Three characteristics serve to differentiate the increased density due to pleural fluid from that due to a parenchymal infiltrate. First, if the density is caused by pleural fluid, the vascular structures of the lung will be readily visible through the density in a properly exposed film. Any intrapulmonary process that produces a similar density, however, obliterates the vascular structure by the “silhouette effect.” Second, if the density is due to pleural fluid, it is usually completely homogeneous. In contrast, infiltrates caused by intrapulmonary processes are usually less homogeneous. Third, air bronchograms are present only if the increased density is due to a parenchymal infiltrate.
Atypical Effusion
The typical arrangement of fluid in the pleural space depends on an underlying lung free of disease and thereby having uniform elastic recoil. If the lung
underlying the effusion is diseased, the elastic recoil of the diseased portion is frequently different from that of the remainder of the lung, and fluid accumulates most where the elastic recoil is greatest. Therefore, an atypical collection of pleural fluid is an indication of underlying parenchymal as well as pleural disease. For example, if disease in a lower lobe increases its elastic recoil, fluid will collect posteromedially. Accordingly, in the posteroanterior projection, the opacity is higher on the mediastinal than on the axillary border, in contrast to the typical appearance in which the opacity is higher at the axillary border. Moreover, the upper surface curves downward and laterally toward the lateral costophrenic sulcus and thereby simulates atelectasis and consolidation of the middle and lower lobes. In the lateral projection, the upper border of the density roughly parallels the major fissure, beginning high in the thorax posteriorly and running downward and anteriorly to the anterior costophrenic sulcus. For the interested reader, Fleischner (12) has detailed the radiographic appearance of atypical pleural fluid accumulation in disease affecting all the individual lobes.
underlying the effusion is diseased, the elastic recoil of the diseased portion is frequently different from that of the remainder of the lung, and fluid accumulates most where the elastic recoil is greatest. Therefore, an atypical collection of pleural fluid is an indication of underlying parenchymal as well as pleural disease. For example, if disease in a lower lobe increases its elastic recoil, fluid will collect posteromedially. Accordingly, in the posteroanterior projection, the opacity is higher on the mediastinal than on the axillary border, in contrast to the typical appearance in which the opacity is higher at the axillary border. Moreover, the upper surface curves downward and laterally toward the lateral costophrenic sulcus and thereby simulates atelectasis and consolidation of the middle and lower lobes. In the lateral projection, the upper border of the density roughly parallels the major fissure, beginning high in the thorax posteriorly and running downward and anteriorly to the anterior costophrenic sulcus. For the interested reader, Fleischner (12) has detailed the radiographic appearance of atypical pleural fluid accumulation in disease affecting all the individual lobes.
Loculated Effusion
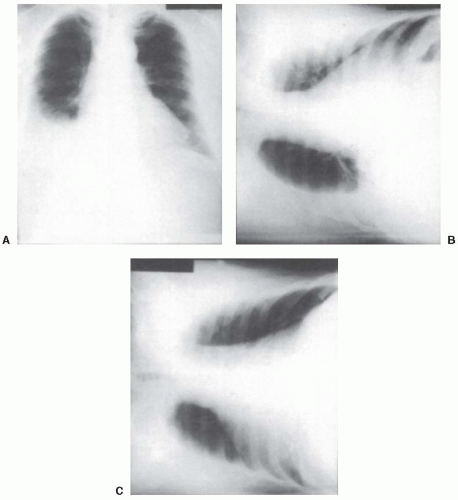
Pleural fluid may become encapsulated by adhesions anywhere between the parietal and the visceral pleura or in the interlobar fissures. Because the encapsulation is caused by adhesions between contiguous pleural surfaces, it occurs most frequently in association with conditions that cause intense pleural inflammation, such as empyema, hemothorax, or tuberculous pleuritis. Loculations occurring between the lung and the chest wall produce a characteristic radiographic picture. When viewed in profile (Fig. 6.5), the loculation is D-shaped, with the base of the D against the chest wall and the smooth convexity protruding inward toward the lung because of the compressibility of the lung parenchyma. If the loculation is in the lower part of the thoracic cavity, its lower border may not be visible. Loculation may be differentiated from parenchymal infiltrates by the absence of air bronchograms. A definitive diagnosis of loculated pleural effusion is best established by ultrasound (see the discussion on ultrasound). Because multiple locules are common, the demonstration of one locule should serve as an indication to search for additional locules.
Loculation in the Fissures
The plane of the lung fissures is such that fluid encapsulated in the fissure is usually seen in profile in the lateral view. Fluid encapsulated in a fissure has a profile similar to a biconvex lens. Its margins are sharply defined and blend imperceptibly into interlobar fissures (Fig. 6.6). In some situations, the loculated effusion may simulate a mass on the posteroanterior radiograph. This situation is most frequently seen in patients with congestive heart failure, and because the fluid absorbs spontaneously when the congestive heart failure is treated, these fluid collections have been termed vanishing tumors or pseudotumors. The most common location of these “tumors” is in the right horizontal fissure (13). These pseudotumors are usually less than 4 cm in diameter, but pseudotumors as large as 10 cm in their largest diameter have been reported (14). The distinctive configuration of the loculated interlobar effusion should establish the diagnosis. The disappearance of the apparent mass as the effusion resolves definitely establishes the diagnosis.
At times, it is difficult to differentiate encapsulated fluid in the lower half of a major fissure from atelectasis or combined atelectasis and consolidation of the right middle lobe. The following three points help make the distinction (1). First, if the minor fissure is visible as a separate shadow, the diagnosis of encapsulated fluid is certain. Second, encapsulated fluid does not usually obscure the border of the right side of the heart; in contrast, middle lobe atelectasis almost invariably does. Third, in the lateral projection, loculated effusions usually have a convex border on one or both sides. When the right middle lobe is diseased, the borders of the shadow are either straight or slightly concave.
RADIOLOGIC DOCUMENTATION
Most of the changes discussed in the previous sections are suggestive rather than diagnostic of the presence of pleural fluid. For example, blunting of the posterior or lateral costophrenic angles can be due to pleural effusion, but it can also be caused by pleural thickening or hyperinflation of the lung. Pleural effusion can obliterate one or both diaphragms on the lateral radiograph, but so can atelectasis or parenchymal infiltrates. Therefore, when the posteroanterior or the lateral chest radiograph suggests a pleural effusion, further radiographic studies are usually needed to document the presence of pleural fluid. Currently, ultrasound is used most frequently to document the presence of a pleural effusion, but lateral decubitus radiographs and computed tomography (CT) scans are useful in this situation.
Lateral Decubitus Radiographs
The basis for the use of the lateral decubitus view is that free fluid gravitates to the most dependent part of the pleural space. The patient is placed in the lateral recumbent position, with the suspect side dependent. Sufficient radiolucent padding should be placed between the tabletop and the patient such that an unobstructed tangential view of the dependent chest wall can be obtained. The x-ray film should be exposed with a high voltage to ensure that the interface between the fluid and the lung can be identified.
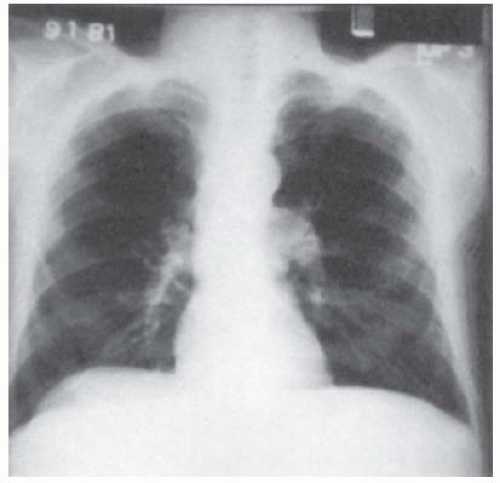
In the decubitus view, free pleural fluid is evidenced by a homogeneous density with a straight horizontal superior border between the dependent chest wall and the lower border of the lung (Fig. 6.7). This appearance is due to the lung floating in the fluid. By injecting fluid into the pleural space of cadavers, Moskowitz et al. have demonstrated that as little as 5 mL pleural fluid can be seen on properly exposed decubitus radiographs (15). Fluid is more easily demonstrated if the decubitus radiographs are obtained at full expiration rather than at full inspiration (16). The amount of free pleural fluid can be semiquantitated by measuring the distance between the inner border of the chest wall and the outer border of the lung (Fig. 6.7); the greater this distance, the more free pleural fluid. Empirically, I have found that when this distance is less than 10 mm, diagnostic thoracentesis is difficult because the amount of pleural fluid is small. Accordingly, I rarely attempt a diagnostic thoracentesis when the thickness of the pleural fluid on the decubitus radiograph is less than 10 mm.
Many patients suspected of having pleural effusions have apparent pleural thickening on the posteroanterior chest radiograph. When decubitus views are obtained in such patients, one must compare the distance between the lung and chest wall on the decubitus view to that on the posteroanterior view. If the distance between the lung and the chest wall is not at least 10 mm greater on the decubitus view, the patient does not have a significant amount of free pleural fluid.
In general, bilateral decubitus chest radiographs should be ordered. The film with the suspect side superior is informative because, in this view, the fluid gravitates toward the mediastinum. With the fluid shifted away from the chest wall and the lung, one can more readily assess the underlying lung for infiltrates or atelectasis (Fig. 6.7C). In addition, if the lateral costophrenic angle is blunted on the posteroanterior view and is clear on the decubitus view with the suspect side superior, one can be certain that the blunting is caused by free pleural fluid.
Frequently, when decubitus radiographs are obtained, confusion exists as to which side is down. An arrow is usually seen on the x-ray film, but whether the arrow is pointing up or down in relation to the patient’s position is the question. Four radiologic characteristics allow the interpreter to ascertain the position of the patient when the radiograph is obtained. First, the dependent lung receives a greater percentage of the perfusion and is therefore more radiodense. Second, with the patient in the decubitus position, the abdominal pressure is greater on the dependent side; therefore, the diaphragm on the dependent side is pushed higher in the thoracic cavity than the contralateral diaphragm. Third, the radiolucent padding or the examination table is often evident outside the thoracic cavity on the dependent side (Fig. 6.7). Fourth, if air-fluid levels are present in the stomach or the intestines, the air will always be on the superior side.
ULTRASOUND
Ultrasound is very useful in the study of pleural disease (17,18,19). Koh et al. (19) and Koenig et al. (20) have produced excellent reviews with several different movies demonstrating various ultrasound findings with pleural disease. Ultrasound can be used in several different situations, including the following: (a) determining whether pleural fluid is present; (b) identification of the appropriate location for an attempted thoracentesis, pleural biopsy, or chest tube placement; (c) identification of pleural fluid loculations; (d) distinction of pleural fluid from pleural thickening; (e) semiquantitation of the amount of pleural fluid; (f) differentiation of a pyopneumothorax from a lung abscess; (g) assessment as to whether a pleurodesis is present; and (h) evaluation of the trauma patient for the presence of a hemothorax or a pneumothorax. The advantages of ultrasound over CT are the ease and speed with which the examination can be performed, the availability of portable units that can be brought to the bedside of seriously ill patients, the lack of ionizing radiation, the relatively low cost, and the capacity to diagnose and distinguish an associated subphrenic process (18,21). With ultrasound, one can also assess the thickness of the parietal pleura and identify pleural nodules and focal pleural thickening (22). Given these advantages, there is no doubt that ultrasound has been underused in the assessment of pleural disease in the United States, but its use has increased dramatically in the past few years. Pulmonologist are utilizing ultrasound themselves more and more extensively (23).
Pleural fluid on ultrasound appears echo free (anechoic), or hypoechoic (reduced echogenicity relative to the liver) (20). For simplicity, pleural fluid collections with ultrasound can be characterized as echo free (anechoic), complex septated if there are fibrin strands or septa floating inside the hypoechoic pleural effusions, complex nonseptated if heterogeneous echogenic material is inside the hypoechoic pleural effusion, and homogeneously echogenic if homogeneously echogenic spaces are present between the visceral and parietal pleura. In one series of 320 patients with pleural effusions, 172 (54%) were anechoic, 50 (16%) were complex nonseptated, 76 (24%) were complex septated, and 22 (7%) were homogeneously echogenic (22). Interestingly, all the patients who had complex-nonseptated, complex-septated, or homogeneously echogenic results had exudative pleural effusions. Patients who had anechoic effusions could have either transudative or exudative pleural effusions (22). However, in a more
recent study 70 of 127 patients (55%) with transudative effusions had a complex nonseptated pattern (24).
recent study 70 of 127 patients (55%) with transudative effusions had a complex nonseptated pattern (24).
Transthoracic chest ultrasonography can be performed with any modern ultrasound unit. A 3.5 to 5.0 MHz with a small footprint allows visualization of the deeper structures, and the sector scan field allows a wider field of view through a small acoustic window. Once an abnormality has been identified, a high-resolution 7.5 to 10 MHz linear probe can be used to provide detailed depiction of any chest wall, pleural, or peripheral lung abnormality (19,20). The high-frequency transducer improves resolution in the near field so that internal echoes in a solid lesion are easier to image, which helps the examiner distinguish solid lesions from cystic lesions. In addition, nearfield reverberation artifacts, which might otherwise obscure fluid close to the skin, are reduced. Real-time scanning is preferred to conventional static scanning because it allows one to assess the changing configuration of pleural fluid with respiration, is easier to use in the intercostal spaces, and requires less time to scan large areas (21). The best distinguishing characteristic of a pleural fluid collection on ultrasound is that it changes its shape with respiration (25).
The posterior chest is best imaged with the patient sitting upright, whereas the anterior and lateral chest are best assessed in the lateral decubitus position. If the patient’s arm is raised above his head, the distance between the rib spaces is increased and this facilitates scanning the patient in the erect or recumbent position (19).
Identifying the Presence of Pleural Fluid
Ultrasound is accurate in identifying the presence of pleural fluid. In one recent study of 60 patients with congestive heart failure, CT scans demonstrated pleural effusions in 52 of the 60 (87%) (26). Ultrasound demonstrated pleural fluid in more than 90% of the patients in whom the fluid was identified by CT scans (26). In another study, lateral decubitus radiographs were able to identify the presence of pleural fluid in 92% of 52 patients who had small amounts of pleural fluid demonstrated by ultrasound (27). Moreover, there was a close correlation between the thickness of the fluid on the ultrasound examination and the decubitus radiograph (27). In a recent study, pulmonologists were able to correctly identify the presence or absence of pleural fluid in 951 of 955 patients (99.6%) (23).
It has been suggested that color Doppler ultrasound is superior to real-time gray-scale ultrasound in the identification of pleural fluid (28). With the color Doppler ultrasound, pleural fluid is identified because it provides a color signal. In one report of 51 patients with minimal pleural effusions, color Doppler ultrasound correctly demonstrated color in 33 of 35 (94%) patients with pleural fluid but was negative in the 16 patients without pleural fluid. In contrast, real-time gray-scale ultrasound identified fluid in all 35 patients with fluid but also in 5 of 16 patients without fluid (28). Another study recently confirmed that color Doppler ultrasound was superior to gray-scale ultrasound in demonstrating the presence of pleural effusion (29).
Ultrasound can demonstrate pleural fluid in normal individuals. Kocijancic et al. (30) performed ultrasonography on a group of 106 healthy volunteers in the lateral decubitus position and then leaning on the elbow. They reported that a layer of pleural fluid greater than 2 mm in thickness was found in 28 of the 106 volunteers (26%). The effusion was bilateral in 17 volunteers and unilateral in 11 (30). When the ultrasonography was repeated 2 to 4 months later, 21 of the original volunteers with fluid still had it, whereas an additional 11 patients had fluid which was not present initially (30).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree