FIGURE 23-1 Extension tubing connecting the manifold and catheter reduces radiation exposure to operators.
Filtration and Collimation
X-ray tubes produce photons with a spectrum of energy levels. Lower energy photons, which would not penetrate through the patient’s skin to contribute to image formation, are filtered out of the beam by aluminium and copper filters that are usually fitted as standard. Operators who are in tune with their machines can make further use of additional wedge filters, which can be employed when bordering lung tissue is exposed to the beam, resulting in lower doses and improved image quality.
Collimation, via either multiple blades or an iris diaphragm, can greatly reduce the image field of view to the region of interest. This will result in a reduced DAP as well as the dose scattered to around the laboratory.
Shielding
Most readers will be familiar with the need to religiously wear lead aprons when in the catheter laboratory. The operator’s exposed areas receive about 0.05% of the patient dose; doses received beneath lead aprons are reduced to about 10% of exposed areas. Wearing leaded thyroid shields and shin guards confers further reduction in doses received by scatter. Cataract formation is another example of a deterministic injury, and this may be commoner among catheter laboratory workers.24 The wearing of leaded glasses has been promoted to reduce ocular doses. Interventional cardiologists may be further concerned by case reports of left-sided cerebral tumors.25 One operator had previously advocated the use of a 0.5-mm lead cap in order to reduce the doses scattered to the head.26
Mobile lead shielding fitted to the couch and suspended from the laboratory ceiling is commonplace, and successfully employed to reduce scattered radiation exposure to operators and staff. Additional lead flaps have been shown to augment the reduction in operator exposure,27 principally by protecting against radiation that is scattered to the operators’ midriff between the shields. The authors frequently note that the usage of these shields, particularly among trainees, can be inconsistent; the benefits of shielding should be emphasized to trainees at induction, and reiterated regularly.
Angulations
The ideal angulations are those that provide sufficient diagnostic data, but reduce doses delivered to the patient and scattered to the operator and laboratory staff.
Studies subjecting phantom patients28 to fluoroscopic doses have reported steeper left or right anterior oblique projections (≥60°) to be particularly dose intensive (Fig. 23-2). There are likely to be benefits in changing habitual use of steep left anterior oblique (LAO) caudal views to posteroanterior (PA) caudal angulations when studying the distal left main stem. Likewise, dose reductions may be achieved by switching from the LAO cranial to a PA cranial view to study left anterior descending (LAD)/diagonal artery bifurcations. Of course, individual anatomy will dictate whether these advocated views provide complete information, but over the course of an interventional career, such altered practice may prove valuable in reducing exposure to patients and staff alike.
Operator Experience and the Transradial Learning Curve
The preceding paragraphs summarized factors that influence radiation dose delivery to patients and catheter laboratory staff. These factors, and some protective measures such as using shielding and avoiding certain angiographic projections, are applicable to all coronary procedures, and irrespective of the access site chosen. Furthermore, providing short tutorials promoting measures designed to reduce doses may well achieve these goals for operators with a wide range of experience.29 For this subsection, we focus on operator experience in transradial access procedures, highlighting the concept of a specific learning curve.
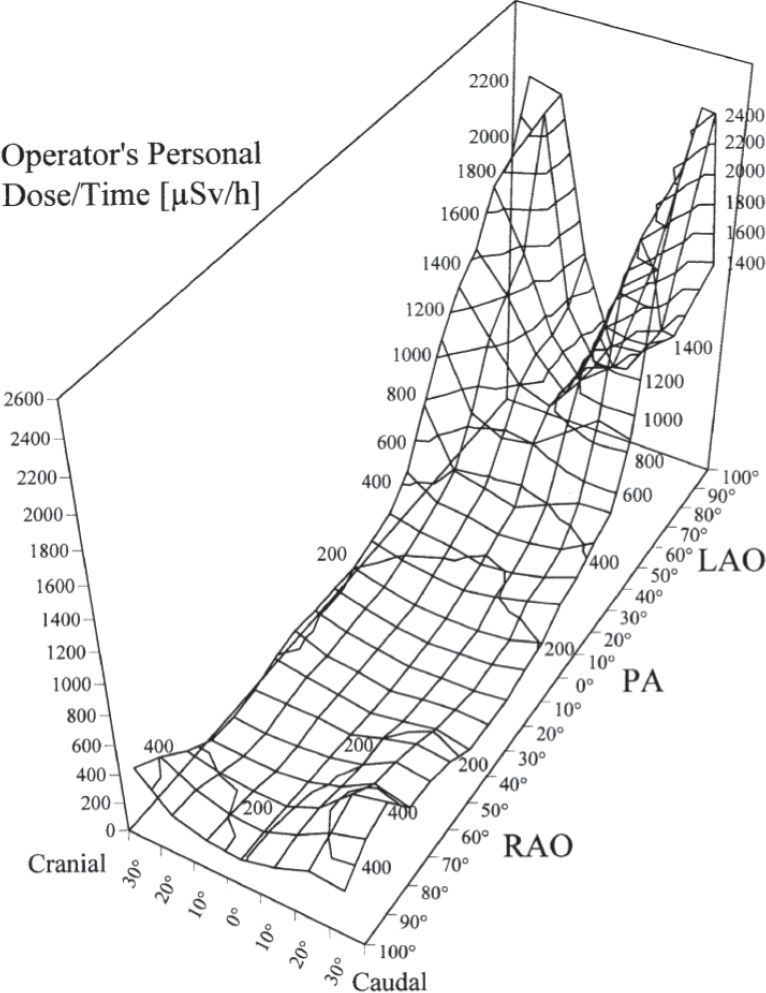
FIGURE 23-2 Calculated isodose lines in a three-dimensional graph of the operator’s mean personal dose per time (µSv/h), as a function of tube angulation. LAO, left anterior oblique; PA, posteroanterior; RAO, right anterior oblique. (From Kuon E, et al. Identification of less-irradiating tube angulations in invasive cardiology. J Am Coll Cardiol. 2004;44(7):1420–1428.)
Early insights into the transradial learning curve came from operators assessing success rates for diagnostic angiography in the 1990s. For example, Spaulding et al.30 described a learning curve for a single operator performing coronary angiography via (left) radial artery access in over 400 patients. Procedure failure occurred in 14% of the first 80 cases, but the failure rate diminished with experience, and was as low as 2% for the last 100 cases performed. Another French group31 reported on the experiences of a single operator who performed angiography in 800 subjects. Among the first 50 cases, the failure rate was 10%, but thereafter dropped to 4% for the cohort volume between 50 and 500. After 500 cases had been performed, the failure rate settled at 1%.
For transradial PCI, a recent study has attempted to illustrate the corresponding curve for interventional rather than diagnostic procedures.32 All nonurgent, single-vessel interventions performed with transradial access in a single Canadian institution between 1999 and 2008 (n = 1,672) were analyzed according to operator experience. Cohorts were stratified according to operator experience by volume: the control group was made up of operators who had performed more than 300 transradial interventions. The study groups were divided into four categories according to volumes: 1 to 50 cases, 51 to 100 cases, 101 to 150 cases, and 151 to 300 cases. Failure rates were significantly higher in the least experienced operators cohort compared to the cohort with 50 to 100 cases under their belts (7% vs 3%, P = 0.007). The failure rate for the experienced control group was 2%. The reasons for failure were the usual banes of the transradial operator: radial artery spasm, subclavian artery tortuosity, unsupportive guide catheters, inability to gain radial access, and radial artery loops. Nevertheless, the authors noted the positive effects of experience, recording a reduction in odds of failure of 32% for each 50 increments in procedure volume.
These studies have indicated that transradial learning curves for diagnostic and simple interventional procedures are steep, with aptitude increasing quickly with case volumes, that need to be augmented by regular practice—of course, this is also the case for transfemoral access. Traditionally, getting to grips with transradial access has been felt to be more difficult than that for the transfemoral route; many of the inherent hurdles led to procedural failures in the study described above.32 Typically, expertise develops after a case volume of over 200 has been recorded. However, it should be noted that the case series reported by Spaulding et al.30 and Louvard et al.31 commenced their studies almost two decades ago, since when the transradial community has benefitted from numerous advantages in equipment and knowledge facilitating performance. When taken together with the fact that trainees are now being taught by experienced radial operators, it could be argued that the learning curve for future trainees should be a good deal smoother. Nonetheless, it is important to recognize that transradial access has its own vagaries that require experience to deal with. An appreciation of this fact is useful when evaluating studies comparing radiation doses delivered by transradial and transfemoral procedures.
Radiation in Transradial versus Transfemoral Studies
Over the last decade or so, a number of studies have evaluated compared radiation doses for transradial and transfemoral procedures. The majority of such studies have been observational in design, although there is now a sprinkling of data derived from some randomized studies.
Most observational studies that have set out to compare radiation exposure for the two access sites have been modest in size, and while many have pointed out an excess in X-ray doses to both patients and operators with transradial access, others have not. However, we believe that there are inherent methodological flaws in these studies that detract from their findings.
Observational Studies
As transradial practice was developing, early studies looking into this area were typically conducted in a single center, with varying experience between operators. It should not be forgotten that these investigators were ploughing a lone furrow in an area without the specific radial tools that have been developed to aid contemporary radial practitioners. Most studies were poorly controlled for the variables that were discussed in the previous section.
Brasselet et al.33 conducted their prospective study of over 400 subjects in a single center over a 6-month period in 2005 to 2006. Technicians compiled dose data for transradial and transfemoral procedures for four operators blinded to these data. Radiation exposure was reported to be higher for transradial procedures for both patients and operators; these findings were consistent for diagnostic angiography alone, as well as for ad hoc PCI after angiography. The authors advised that indications for using transradial access ought to be reconsidered. These results have been frequently cited in the long debate that has ensued. On closer inspection, however, there are a number of issues with this study. First, a number of relevant factors were uncontrolled. For example, while the four operators were well versed in radiation protection, and adhered to use of lead shielding, there was no standardization for radiographic angulations. In addition, there were important differences between the subjects in the transradial and transfemoral patient groups. First, the transradial group had a significantly higher mean mass than their counterparts, and it is likely that this would be reflected in higher doses. Second, complex coronary lesions occurred more frequently in the transradial group, and could have potentially accounted for more radiation. Of course, it is difficult to control for all factors in what may have been a “real-world” study, but the results were not adjusted for these potential confounders. Another key issue was that of operator experience. The transradial procedures comprised <60% of the overall cases for all four operators during the study period, and this fact was highlighted as a marker of a relative inexperience by observers34; it was posited that the operators may have participated in the study in the middle of their radial learning curve, whereas they were very experienced in transfemoral work. The authors had acknowledged not only that their transradial volumes were in the “mild-moderate” category, but also that this was representative for many European centers at that time.
Our center35 recently performed a prospective observational study with dual hypotheses to further characterize the effects of uncontrolled variables and operator experience: first, there would not be a disparity in dose measures between access sites when important variables were controlled for; second, operator experience would influence radiation exposure regardless of access site. One hundred consecutive patients undergoing their first diagnostic angiography were recruited. An experienced operator who used femoral access as his default route performed 25 cases, with a further 25 cases performed by a similarly experienced transradial counterpart. A trainee operator of intermediate experience with both modes of access performed the remaining cases, with 25 procedures by each route. Of note, imaging projections were standardized—the same views/angles were used to acquire five acquisition runs for the left coronary artery and three runs for the right coronary artery (left ventricular angiography was performed for all cases with the same projection). Furthermore, operators made similar use of available lead shielding in all cases. Among the patients, there were no differences in anthropometric measurements or comorbid conditions.
For the expert operators, there were no differences in ED, DAP, or FT. However, the operator (by 25%–30%) and patient (by 10%–15%) exposures were significantly higher for the intermediate operators than for the experts, for both the access routes. Interestingly, there were no significant differences for the trainees’ dose parameters when analyzed by access route. Thus, it is likely that inadequate controlling of pertinent factors and disparities in operator experience have contributed to observational data in the past.
A Dutch group36 has since further emphasized the need to take confounding factors into account. This team analyzed the procedural database at their high-volume unit: patient doses (as DAP) were recorded among 4,000 patients undergoing diagnostic and interventional procedures over the period 2004 to 2008. The authors constructed a predictive model in order to compare observed transradial doses with expected transfemoral doses once differences in, for example, lesion complexity were considered. From this model, diagnostic and therapeutic procedures performed transradially did not carry an increased radiation burden. In addition, when radial observed doses were stratified according to when the cases were performed, it was evident that there was a progressive fall in exposure with increasing experience. Of note, operator doses were not reported in this study.
A further single-center, retrospective study reported exposure between the two access sites for diagnostic and interventional procedures among experienced operators.37 While FTs and DAP were increased with transradial access in both types of procedure, it is noteworthy that the differences in radiation doses delivered did not reach significances once procedures involving either trainee fellows or surgically grafted patients were excluded.
Similarly, but on a larger scale, investigators for the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) conducted a study between 2008 and 2012.38
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


