FIGURE 6-1 Normal anatomy of the forearm arteries.
Although the deep palmar arch is found to be angiographically complete in 95% of subjects, a complete superficial palmar arch is seen in only 40% to 80% of individuals, depending on the mode of study.21 This probably explains the relatively high incidence of abnormal Allen test results,24 an indication that ulnar collateral support to the hand is inadequate in a significant proportion of individuals. The high prevalence of a complete deep palmar arch suggests that radial collateral support is more frequently present, and that cannulation of the ulnar artery should be relatively safe (Fig. 6-4).14

FIGURE 6-2 Superficial and deep palmar arch.

FIGURE 6-3 Superficial palmar arch—primarily ulnar.
Slogoff et al.,25 reporting on the safety of radial and ulnar artery cannulation, described a subset of 22 patients who underwent ipsilateral ulnar artery cannulation after numerous failed attempts at radial artery cannulation. No patient experienced ulnar artery occlusion or signs and symptoms of hand ischemia. For the vast majority of patients, the smaller-caliber, more superficial radial artery is easier to palpate at the wrist than the ulnar artery; the radial artery is properly the target for access in these individuals.26 However, in a small number of patients, the ulnar artery is palpably the larger vessel at the wrist and is the reasonable choice for cannulation (Figs. 6-5 and 6-6).
Similar to the radial artery, the ulnar artery can also have anatomical variation. The most common cases of ulnar artery variations (7.7%) are ulnar artery with high takeoff from the brachial or axillary artery. The brachial artery is the more frequent site of the ulnar artery takeoff, with the lower portion being more common than the upper portion.27,28 The superficial ulnar artery is a rare variation of the upper limb arterial system that arises from the brachial or axillary artery and runs superficial to the muscles arising from the medial epicondyle. The variable incidence is about 0.7% to 7% (Figs. 6-7 and 6-8).18

FIGURE 6-4 Incomplete superficial palmar arch: retrograde ulnar arteriography with cannula.

FIGURE 6-5 Hypoplastic radial artery and larger-size ulnar artery.

FIGURE 6-6 Very complex 360° loop of the radial artery distal to the bifurcation of the brachial artery.
Loops and curvatures of the ulnar artery are very rarely encountered in comparison to the radial artery equivalents.
Furthermore, the radial artery and the ulnar artery atherosclerosis and calcifications may be an important marker for extensive extracardiac vascular disease. Many such patients were found to have severe brachiocephalic tortuosity that could not be navigated, leading to procedural failure, especially during the initial learning phase.29

FIGURE 6-7 Radial artery loop and high takeoff of the ulnar artery.

FIGURE 6-8 TUA with high takeoff of the ulnar artery from the midbrachial artery, after failed radial artery cannulation (left arrow sign).
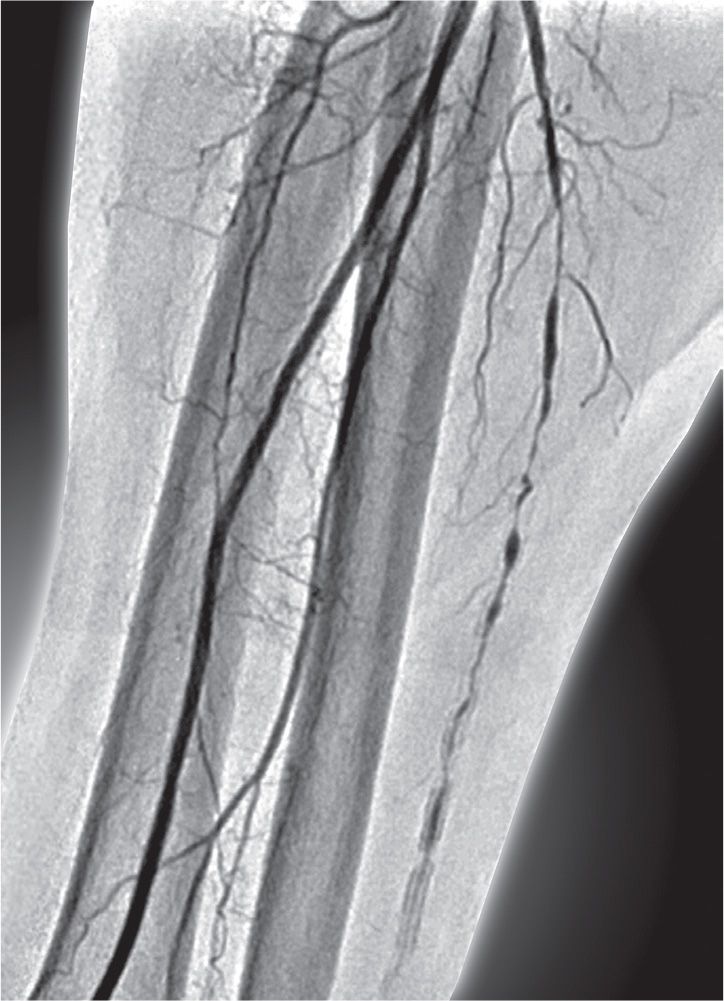
FIGURE 6-9 Severely atheromatous and calcified right ulnar artery.

FIGURE 6-10 Calcifications of both right radial and ulnar arteries.

FIGURE 6-11 Left ulnar artery calcifications in the same patient.
The early recognition of such anatomy at procedure outset is important for avoiding potential complications (Figs. 6-9 to 6-11).30
Allen Tests, Pulse Oximetry, and Doppler Plethysmography
Allen test is done on the right or left wrist, and its purpose is to determine the ulnar artery patency and adequate radial–ulnar collaterals to the hand.
A reverse Allen test is performed by compressing both the radial and ulnar arteries and having the patient make fist clenches several times. In contrast to the Allen test, in which pressure on the ulnar artery is released, for the reverse Allen test, occlusion of the ulnar artery is maintained while pressure on the radial artery is released. If there is return of blush to the palm within 10 seconds, the test is considered positive and indicates adequate collateral supply to the hand.
The modified Allen test should be performed in order to assess the adequacy of the ulnar artery supply to the palmar arch. It can be conducted with the pulse oximeter sensor placed over the index finger. A normal waveform should be observed before arterial compression. The test is conducted in the same manner, but instead of observing hand color when releasing the ulnar artery, the pulse oximetry tracing is examined. The tracing is initially blunted or flat when both the radial and ulnar arteries are occluded. The tracing should return to the baseline within 10 seconds after releasing the ulnar artery for the test to be considered normal. The presence of an arterial waveform (even if delayed or with reduced amplitude) and a hemoglobin oxygen saturation >90% confirm the adequacy of the ulnar artery supply to the palmar arch.31 The pulse oximetry method is preferred, because it is not as subjective as the traditional Allen test. For the Doppler plethysmography test, the radial and ulnar arteries are compressed sequentially while confirming normal audible signal intensity over the palmar arch. Doppler plethysmography and pulse oximetry are of particular importance for ensuring “patent hemostasis” after sheath removal.
Puncture Technique
Preprocedure evaluation of the wrist includes palpation of both the radial and the ulnar arteries, with access attempted of the more superficial vessel, provided there is demonstrated competent palmar collateral support to the hand by the ipsilateral complementary vessel.9
A large enough area should be prepared to cover both the radial and ulnar arteries, and to place the sterile drape so that it need not be moved in the event the ulnar artery is used.
The wrist is hyperextended and the skin is prepared with local anesthesia (1-mL lidocaine 2%) at the site where the pulse is strongest, usually 0.5 to 3 cm proximal to the pisiform bone for ulnar artery and 1 to 2 cm proximal from the styloid process for radial artery access. Compression of the ipsilateral radial artery could improve weak or hardly palpable ulnar artery pulsations and facilitate ulnar artery cannulation. The ideal ulnar artery puncture site is approximately 0.5 to 3 cm proximal to the flexor crease skinfold along the axis with the most powerful pulsation of the artery. The needle should be inserted at a 45° to 60° angle along the vessel axis and from lateral to medial, avoiding the ulnar nerve. The ulnar artery is preferentially punctured with a 20G plastic cannula using the Seldinger technique. When a good arterial “back bleed” is obtained, the 0.025” hydrophilic wire guidewire should be gently advanced and the hydrophilic sheath should be introduced over the guidewire (Fig. 6-12).
An intra-arterial vasodilator (most frequently 5-mg verapamil) is injected via the cannula or through the sidearm of the sheath to reduce ulnar artery spasm. In order to prevent the painful and burning sensations, blood is mixed with verapamil before injection. Immediately after sheath insertion, intravenous unfractionated heparin should be administered (50–70 U/kg, up to 5,000 units) to reduce the risk of radial artery thrombosis (Fig. 6-13).
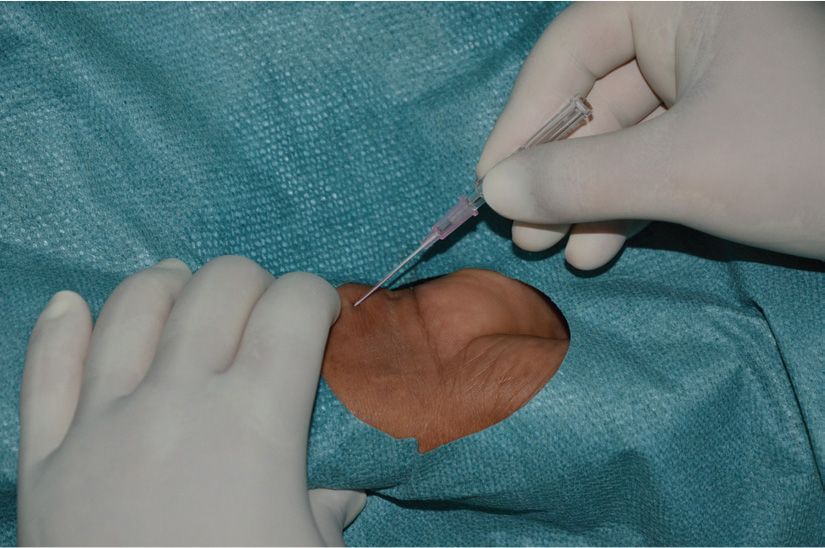
FIGURE 6-12 Puncture of the right ulnar artery with a 20G plastic cannula by the Seldinger technique.
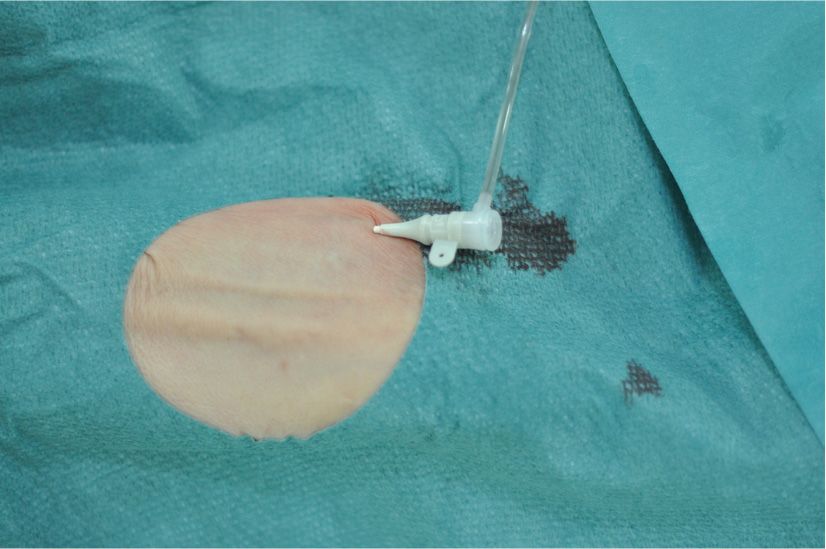
FIGURE 6-13 Short 5F sheath in the right ulnar artery.

FIGURE 6-14 Distal cannulation of the right ulnar artery with 90-cm-long 6F (inner lumen) guiding sheath for carotid artery stenting.
Procedure failure for ulnar artery access is almost always related to the puncture, which can be more difficult than the radial artery puncture, because of the deeper ulnar artery course and lower intensity of pulsations.
Distal puncture of the ulnar artery: In cases when ulnar artery pulsations are weak but palpable at the distal wrist, it is safe to puncture the ulnar artery more distally, at the level of skinfolds (over the carpal bones). The risk of postprocedural hematoma is lower when puncturing the ulnar artery near the wrist’s skinfolds (Fig. 6-14).
High puncture of the ulnar artery: Although the ideal site for puncture is 0.5 to 3 cm proximal to the pisiform bone, the ulnar artery can be punctured up to the midforearm as long as the pulsations can be felt. This approach may be useful for an experienced operator performing coronary or endovascular interventions requiring larger-bore devices. However, the ulnar nerve is very close to the ulnar artery in that region, and so the puncture has to be very accurate and the operator has to be very cautious, avoiding accidental nerve damage.18
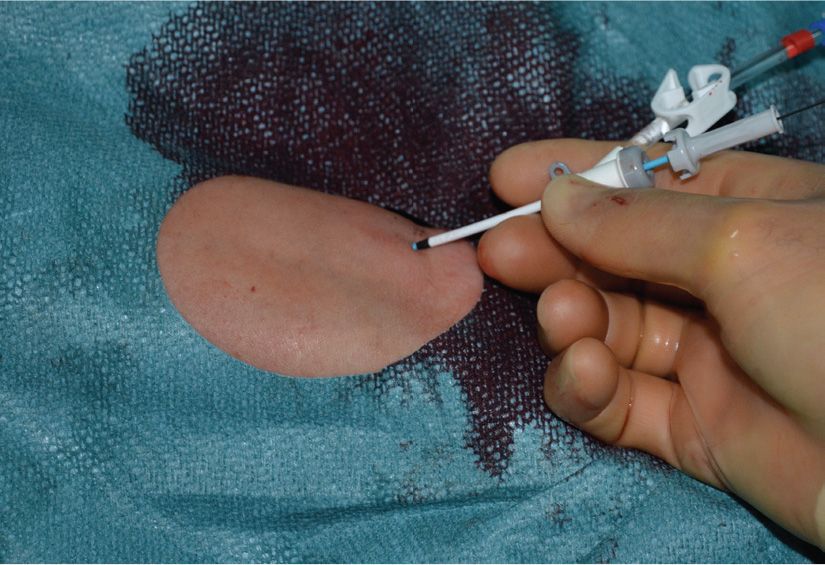
FIGURE 6-15 Initial ulnar artery cannulation with short 5F sheath, before exchanging with larger-bore dedicated sheathless guiding catheter.
Once the sheath is in place, the transulnar procedure is performed in the same manner as the transradial catheterization.
Particular care should be undertaken while exchanging and upgrading sheaths of different sizes with dedicated sheathless guiding catheters, in order to avoid local bleeding complications related to the inappropriately sized devices. For example, this could be the case when the initial 6F introducer sheath is exchanged with 7.5F dedicated sheathless guiding catheter that has smaller outer lumen diameter. Therefore, a short 4F or 5F introducer sheath is recommended initially when complex procedures with larger-bore devices and sheathless guiding catheter exchanges are considered (Figs. 6-15 and 6-16).
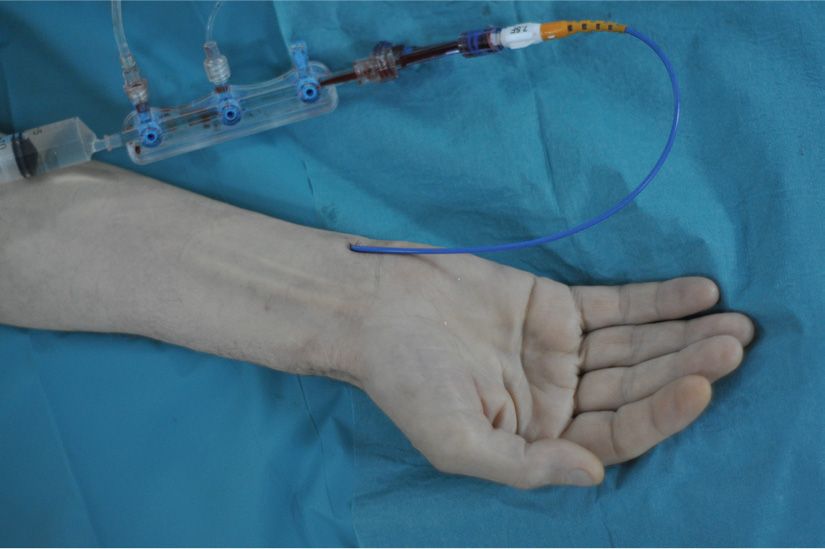
FIGURE 6-16 Right TUA for complex PCI with 7.5F (outer lumen) dedicated sheathless guiding catheter.
Retrograde Arteriography of the Wrist
Radial and ulnar artery anomalies are relatively common and a cause of procedural failure even for experienced radial operators. Retrograde radial and ulnar arteriography helps to assess the diameter of the arteries and delineate underlying anomalies. By identifying patients with unfavorable anatomy, the operator could plan a strategy to overcome the anomaly or change access route with the potential to save time and avoid vascular complications.29
After administration of the arterial vasodilatator, a solution of 3 mL of contrast mixed with 7 mL of blood is injected briskly through the cannula or through the side arm of the sheath under fluoroscopy in anterior–posterior (AP) position to define the anatomy of arteries from the distal forearm to the brachial anastomosis (Fig. 6-17).
When high-bifurcating radial or ulnar artery origin is detected, a further arteriography is needed to identify higher up the point of anastomosis to the brachial or to the axillary artery.
If anomalous anatomy, tortuosity, or loops are identified, the operator can further plan the procedure on that basis. In most cases, crossing with hydrophilic coronary guidewire under fluorography control is highly recommended (Fig. 6-18).

FIGURE 6-17 Retrograde ulnar arteriogram through a cannula.

FIGURE 6-18 Road map from retrograde radial arteriogram in a patient with radial artery loop and high takeoff of the ulnar artery.
The acquisition of a radial and ulnar arteriogram requires only a minimal contrast load, a small amount of additional radiation, and trivial extra procedural time. Retrograde angiogram of the wrist is of particular importance in patients with several previous transradial interventions. By providing important road map and estimating the artery dimension, it aids the operator to plan an optimal procedure with appropriately-sized catheters.

FIGURE 6-19 Right ulnar arteriogram showing larger-size ulnar artery eligible for large-bore 7F catheterization.
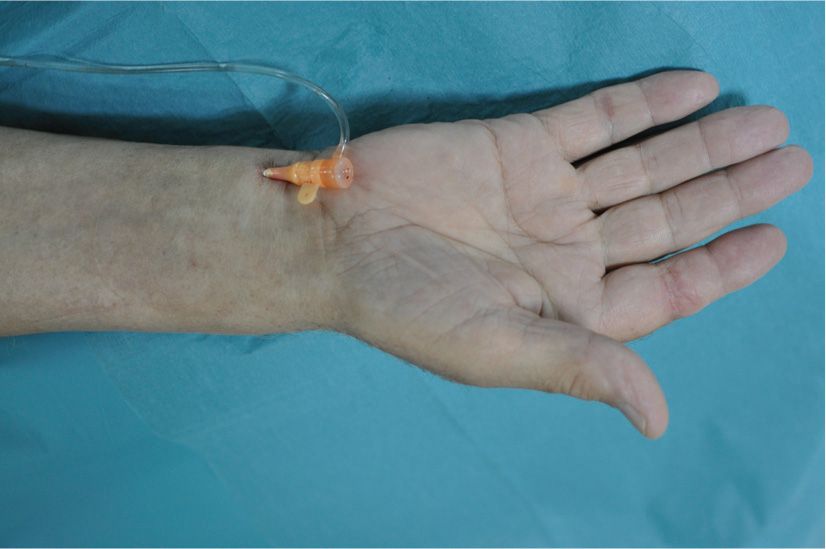
FIGURE 6-20 Right TUA with 7F sheath in place for complex PCI.
Moreover, an angiography of the wrist can be incorporated as a routine part of either transradial or transulnar catheterization, particularly in complex procedures requiring large-bore devices (Figs. 6-19 and 6-20).
Postprocedure Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


