|
▪ ARTERIAL PATTERNS |
▪ DESCRIPTION |
▪ INCIDENCE |
Arm |
1 artery |
Brachial (Normal) |
|
76.06% |
|
Superficial brachial |
Brachial artery is superficial to the nerve |
4.9 |
2 arteries |
Brachial and accessory brachial |
Brachial artery branches in the upper arm and rejoins above the elbow |
0.26 |
|
Brachial and brachioradial |
Radial artery with high origin |
13.8 |
|
Brachial and superficial brachioradial |
Radial with high origin and superficial to the nerve |
<0.26 |
|
Brachial and brachioulnar |
Ulnar artery with a high origin |
0.26 |
|
Brachial and superficial brachioulnar |
Ulnar with high origin and superficial to the nerve |
4.2 |
|
Brachial and superficial brachioulnoradial |
Brachial has radial and ulnar branches but continues into interosseus |
0.52 |
|
Brachial and superficial brachiomedian |
High origin of the median artery, which is superficial to muscles |
<0.26 |
|
Brachial and brachiointerosseus |
High origin of the interosseus artery coexisting with brachial artery |
<0.26 |
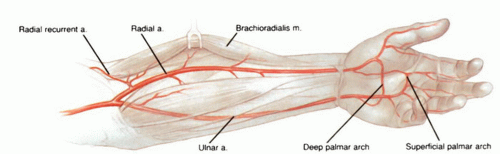
Forearm |
1 artery |
Ulnar and radial absent |
|
<0.26 |
|
Radial and ulnar absent |
|
<0.26 |
2 arteries |
Ulnar and radial (Normal) |
|
81.22% |
|
Ulnar and brachioradial |
High origin of the radial artery |
13.8 |
|
Ulnar and superficial brachioradial |
High origin of the radial artery and superficial to muscle/tendons |
<0.26 |
|
Ulnar and superficial radial |
Radial artery superficial to muscle |
0.52 |
|
Radial and brachioulnar |
High origin of the ulnar artery |
0.26 |
|
Radial and superficial brachioulnar |
Ulnar has a high origin and is superficial to muscle |
4.2 |
|
3 arteries |
Ulnar and radial and brachiomedian |
High origin of the median artery |
<0.26 |
|
Ulnar, radial, and superficial brachioradial |
Radial duplication |
<0.26 |
|
Radial, ulnar, and superficial brachioulnar |
Ulnar duplication |
<0.26 |
Adapted from Rodriguez-Niedenfuhr M, Vazquez T, Nearn L, et al. Variations of the arterial pattern in the upper limb revisited: A morphological and statistical study, with a review of the literature. J Anat 2001;199:547-566. |