FIGURE 18-1 Angiography demonstrating acute bifurcation angle between left anterior descending and diagonal branch arteries; this anatomy is unlikely to be adequately treated with T-stent technique, with a provisional stent technique preferred, given the small caliber of the side branch and the minimal extent of disease into the side-branch vessel.
A technique that in the drug-eluting stent era has found much better success is the culotte technique. The technique has been validated in the Nordic-2 trial, a randomized comparison of the culotte and crush techniques.25 Of 424 patients enrolled in the trial, 209 patients were randomized to crush and 215 to culotte. MACE occurred in 4.3% of the patients in the crush group and 3.7% of those in the culotte group (P = 0.87). In-stent restenosis in the side branch occurred less frequently in the culotte group (9.8% vs 3.8%, P = 0.04).
Given the complexities acknowledged with the use of standard stent therapies in the treatment of bifurcation lesions, interest in novel, dedicated stent platforms to treat both main vessel and side branch subsequently emerged. The initially available platforms were designed to treat the main vessel and to simultaneously allow ongoing access to the side branch through an aperture in the main vessel stent, thus maintaining access to the side branch without the need to rewire through stent struts. The first dedicated stent platform using this approach was the Frontier stent (Guidant Medical, Indianapolis, IN), which, although initially demonstrated to be safe and feasible in clinical trials,26 including from the radial approach,27 was limited by difficulties with device delivery and complexity of use. Although several dedicated bifurcation stents have been evaluated in clinical trials, none has clearly demonstrated superiority. The AXXESS self-expanding biolimus-coated stent (Biosensors International, Switzerland) is specifically designed to be placed in the proximal main vessel precisely at the carina before implanting a further two stents into each of the main vessel and side branch. The concept of this device is for the AXXESS stent to conform to the proximal vessel, ensuring stent coverage to the point of the bifurcation carina, with stents then placed in the side branch to cover the ongoing vessels. These dedicated bifurcation stents can be used from the radial approach, as the majority of those in development may be used through a 6F or 7F guide catheter. An inherent limitation in the development of such technology is the variability in bifurcation anatomy, with differences in vessel caliber, extent of disease, and bifurcation angle, meaning a single device type is unlikely to be able to meet the requirements of every anatomical variant.
As the two-stent techniques proliferated, many operators questioned the two-stent approach as a default strategy for patients needing intervention of bifurcation lesions. The Nordic Bifurcation Study randomized 413 patients to the simple or two-stent approach.21 The crush and culotte techniques were utilized in the majority of patients randomized to the two-stent approach. No difference between the groups was observed in the occurrence of MACE at 6 months, while the two-stent technique was associated with significantly longer procedural and fluoroscopy times, as well as larger volumes of contrast used. The authors concluded that the provisional strategy should remain the preferred method for the majority of patients undergoing bifurcation stenting. In 2010, the British Bifurcation Coronary (BBC) Study investigators reported similar results.20 In a patient-level pooled analysis that included all 910 patients enrolled in these two studies, Behan et al.28 found a highly significant difference between the simple and complex approaches in the occurrence of MACE at 9 months (10.1% vs 17.3%, P = 0.001). Subgroup analyses of patients with true bifurcations only, those with large side branches, at least 2.75 mm in diameter, side-branch lesions at least 5 mm long, similarly revealed better outcomes with the simple, provisional stenting technique. While Nordic and BBC-1 thus appear to provide strong support for the preferential use of the provisional approach in most bifurcation procedures, the techniques utilized in the complex group of both studies resulted in suboptimal treatment in that treatment group. The final kissing balloon inflation, the key final step in any two-stent bifurcation technique, was performed in only 75% of patients, undoubtedly as a result of the inherent difficulty in performing this step with the original single-step crush technique, noting the subsequent advent of techniques designed to optimize the likelihood of final kissing inflation.
Nonetheless, the preferred approach for the majority of bifurcation interventions remains the provisional approach.29,30 Considerable research has been done to optimize the results of the provisional or planned one-stent approach. As a result, outcomes associated with this simple approach have improved considerably over the years. These refinements are discussed in subsequent sections.
Adaptation of Bifurcation Techniques to the Transradial Approach
Greater operator familiarity with the radial artery approach now allows for the performance of complex bifurcation PCI. It is now possible to perform bifurcation PCI from the radial artery access site using provisional strategy, as well as the various complex, two-stent procedures. The radial artery approach is ideally suited for complex bifurcation PCI, given the need to balance the risks of bleeding complications and associated deleterious effects on outcome and the need for aggressive antiplatelet therapy, often using glycoprotein IIb/IIIa inhibitors, especially when employing a two-stent strategy.31 Today, it is imperative that the bifurcation strategy be planned in advance considering all details of the anatomy of the bifurcation lesions.
Bifurcation PCI, particularly when utilizing a complex, two-stent strategy, is associated with longer procedural duration, higher volumes of contrast, and prolonged radiation exposure.21,32–34 As previous data have demonstrated that radial artery access may be associated with similar adverse characteristics in terms of procedural duration, contrast dose, and radiation exposure,33,35 the cumulative effects of these issues should be an important consideration before proceeding to bifurcation PCI from the radial access site. Consideration of a staged procedure is appropriate when a complex intervention is planned after diagnostic angiography, given the potential for contrast nephropathy.
An important limitation of the radial artery approach is the radial artery size, which is more problematic in the older, female population.36 While the use of smaller-caliber guide catheters, such as 5F guides (see Chapter 8), has improved the feasibility of PCI from the radial approach, the use of smaller-caliber guide catheters may have important implications in terms of procedural ease and success. The smaller internal diameter precludes simultaneous delivery of intravascular devices when performing complex bifurcation PCI. This may involve delivery of multiple stents or balloons to both the main vessel and the side branch, with final kissing inflation imperative when using complex techniques such as the crush or culotte technique. Rewiring of the side branch in order to complete final kissing inflation may be problematic in any bifurcation strategy and result in excess contrast exposure; the use of dedicated microcatheters designed to facilitate side-branch access, such as the Crusade microcatheter (Kaneka Medical Products, Osaka, Japan), may be beneficial in these situations.37 When using a simple strategy of main vessel stenting alone, the presence of disease within the side branch may also require final kissing balloon inflation in order to optimize results and reduce the risk of restenosis at the side-branch ostium.38 With current guiding catheters available outside Japan, if the operator considers performing kissing techniques, then a ≥6F is required.
The use of smaller-caliber guide catheters may also result in inadequate backup, which may be critical in terms of the ability to deliver devices to the target lesion. Such difficulties may be minimized by the use of guide catheters that provide optimal support, such as Amplatz curve and extra backup (e.g., XB [Cordis, Bridgewater, NJ], EBU [Medtronic, Minneapolis, MN]) guides. Additional support may be provided by the use of larger-caliber guides, noting the importance of guide caliber in providing adequate support. Standard large-caliber guide catheters, such as 7F and 8F guides, may be used from the radial approach in selected patients in centers with considerable radial artery access experience.39 The development of sheathless guide catheters (such as the Eaucath [Asahi Intecc, Tokyo, Japan]) has further improved the ability of operators to utilize large-caliber guide catheters40 (see Chapter 20). These devices may improve procedural success, without increasing the risk of radial artery injury; however, larger-caliber guides may predispose to ostial vessel dissection and increased contrast volumes.41 The use of traditional guide catheters without a standard introducing vascular sheath has recently been described and may also overcome the limitations of radial artery size in allowing larger-caliber guides.42 Additional techniques to improve backup and ensure delivery of devices in complex procedures include the use of anchor balloons, buddy wires, and internal guide catheter extension tools such as the Guideliner (Vascular Solutions, Minneapolis, MN) and Heartrail (Terumo, Somerset, NJ) systems.43–45
Complex strategies in bifurcation PCI amplify the limitations seen in PCI from the radial approach. Randomized data have confirmed the additional contrast load, radiation exposure, and increased periprocedural complications in complex strategies compared to main vessel stenting alone21,34 without offering clinical advantages.46,47 As outlined, the extent of disease in, and the vessel caliber of, the side branch may, however, necessitate a two-stent strategy. The decision as to which complex approach to utilize may depend on the relative size of the side branch compared to the proximal and distal main vessel. An important caveat when considering a two-stent strategy is the inferior results seen when performing left main PCI. While left main PCI is feasible from the radial approach, complex strategies when applied to left main lesions are consistently disappointing.9,48,49 Additional factors influencing the technique used will include appreciation of the bifurcation angle, which is an important predictor of outcome when using complex bifurcation PCI techniques; this may influence the type of approach should a two-stent strategy be considered.1,50
The Single-Stent or Provisional Approach
As we discussed earlier, the single or provisional approach is widely regarded as the preferred approach for the majority of bifurcation lesions. The provisional stenting approach is ideally suited to the transradial approach. In terms of guide catheter size, it is possible to perform a simple bifurcation intervention with a 5F guide catheter, deploying devices with a second wire in the side branch. Smaller guide catheters, however, may not be suitable in cases requiring more complex side-branch management should this vessel become compromised. This should be kept in mind if the operator plans to use a 5F guide catheter.
In general, a side branch that we would consider as supplying significant myocardial territory should be protected with a wire. The exception to this recommendation might be a side branch without ostial disease in a T-bifurcation (bifurcation angle <70°) that is very unlikely to be occluded after main vessel stenting and may be problematic to wire, exposing the risk of ostial vessel dissection. There is little downside to protecting any other type of side branch and much to be gained in case of significant narrowing after deployment of the main vessel stent that could result in occlusion of the branch. In such cases, the wire will serve two important purposes. First, it will serve as a directional guide to recrossing with another wire. Second, it will serve as a scaffold to maintain some degree of patency in the side-branch origin. If the side-branch ostium is compromised, the side branch should be recrossed and dilated, expanding the struts to open the cell and thus side-branch ostium. The recrossing of the side branch is facilitated by first performing the proximal optimization technique (POT).51 This is accomplished by inflating a balloon in the proximal main vessel with a balloon, the distal tip of which is positioned at the bifurcation. Inflation of this larger balloon in this position results in an angled approach to the side branch that will facilitate reentry through the struts into the side branch (Fig. 18-2) and will minimize the possibility of the new guidewire advancing underneath the proximal stent struts. The recrossing of the side branch should be at the level of the distal-most struts overlying the side-branch ostium. Distal recrossing results in the least stent distortion in the main vessel, and creates a “flap” of stent material that can serve as a scaffold for the proximal wall of the side-branch ostium (Fig. 18-3). Once the side branch is recrossed, a noncompliant balloon of a diameter appropriate for the branch should be positioned covering the diseased ostial tissue and into a normal segment. A second noncompliant balloon should be positioned in the main vessel, and the proximal markers of the two balloons should then be aligned, ensuring that they are within the stented segment. The side branch should be dilated first to ensure optimal opening of the stent struts at the side-branch ostium. A kissing balloon inflation should then be performed. If the flow is TIMI 3 and no significant dissection is observed, the procedure is then completed. Interestingly, Sgueglia et al.52 have recently shown that kissing balloon techniques could be performed with drug-eluting balloons using the transradial approach.
If side-branch compromise persists, a suitable two-stent technique should then be performed. The techniques that can be utilized are T-stent, TAP (T and protrude), or culotte, depending on the bifurcation angle and size of the side branch relative to the proximal main vessel.29 All of these techniques are easily suited to the transradial approach utilizing 6F guides. We will discuss them further with respect to considerations specific to this access in upcoming sections.
The Culotte Technique
The culotte technique is an elegant bifurcation strategy when the side branch is considered to require stent implantation, with documented superiority when compared to the crush and other two-stent techniques.1,25 This technique ensures that complete coverage of the side-branch ostium, however, is limited by two layers of stent in the proximal main vessel. As this technique requires sequential delivery of (drug-eluting) stents, it is ideally suited to the radial approach, with the final kissing balloon inflation the only component requiring simultaneous delivery of multiple devices. In terms of preprocedural evaluation, the culotte technique may be considered when the side branch is similar in caliber to the proximal and distal main vessel with significant disease in the side branch beyond the ostium. A low bifurcation angle and moderate distal vessel size (<3 mm diameter) will favor an optimal outcome in terms of subsequent events.1
Following predilatation of the main vessel and side branch, the first stent is positioned, typically in the distal vessel with the greatest angulation (usually the side branch). As difficulty is usually encountered when positioning the second stent through the stent struts of the previously deployed stent, reducing the degree of angulation may facilitate the delivery of the second stent. After the first stent is deployed, jailing the main vessel wire (which may act as a guide for subsequent rewiring through the struts of the first stent into the distal vessel), the side-branch wire is removed. After opening the stent struts using a small-diameter compliant balloon following rewiring, the second stent is placed distally in the main vessel and deployed after removal of both the jailed and side-branch wire, resulting in the two layers of stent in the proximal, main vessel. The side branch is then rewired with the aim of completing the procedure with a final kissing balloon inflation.
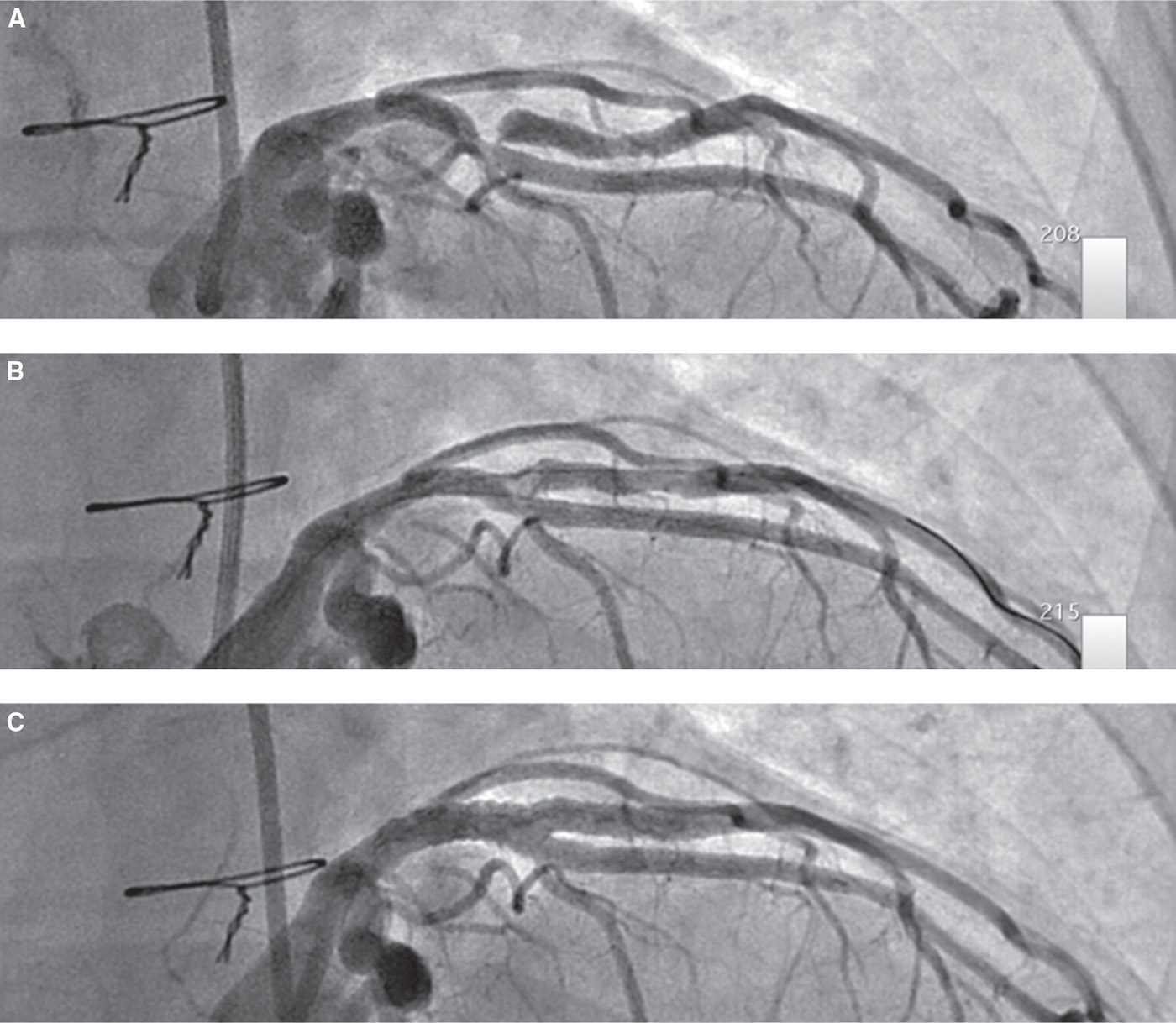
FIGURE 18-2 A:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


