From Rao S, Kaul P, Liao L, et al. Association between bleeding, blood transfusion, and costs among patients with non–ST-segment elevation acute coronary syndromes. Am Heart J. 2008;155:369–374.
A German group randomly assigned patients to radial or femoral access and tracked the amount of time staff spent caring for these patients. In diagnostic cases, nursing care was needed for 13 minutes less with radial cases as compared to femoral cases (P < 0.02), primarily related to the time it took to perform MC of the access site. For PCI procedures, the difference was much larger, with the radial cases requiring 34 minutes less of nursing care (P < 0.01). They estimated that in their laboratory, where 3,000 procedures are performed annually, including 1,000 PCIs, radial cases would save them 1,383 hours of staff time.25
An Italian group looked at a cohort of 260 consecutive patients (52 femoral and 208 radial).26 Catheterization laboratory nurses required less effort to care for patients who underwent TR access (86 minutes vs 174 minutes, P < 0.001) than for TF access patients. The ward nurses provide the bulk of postprocedure care. The investigators noted that the workload for ward nurses was 720 minutes and 386 minutes for femoral and radial procedures, respectively (P < 0.001). These smaller studies seem to reinforce what many radial operators, nurse managers, and hospital administrators have observed in everyday practice, namely, caring for TR patients is easier than for TF patients. In order to realize an economic benefit, the medical center or practice needs to tailor its care processes and adjust staffing ratios to account for the improved efficiency of radial access cases.
Length of Stay
In the economic substudy of GUSTO IIb, prolonged LOS was the primary driver for the increase in costs that were observed.21 In the EASY (EArly discharge after transradial Stenting of coronarY arteries) trial (covered later in this section), the primary driver of the cost differential between the overnight observation group and the same-day discharge group was the costs related to spending the night in the hospital.27 A group of investigators from Mexico noted that nearly 90% of the cost savings found with the radial approach were related to LOS.28 The association between complications and LOS is complex. It stands to reason that a prolonged LOS is often a consequence of complications, but it should be clear that there are intrinsic costs to occupying a hospital bed, including the cost of the room and staff utilization. This does not take into consideration the “opportunity cost” or the ability to use that room for another patient admission. In the United States, health-care systems are just beginning to identify hospital admissions where minimal patient care is occurring, the hospital admission is primarily for observation, or the overnight stay is based on historical standards. Government payers and private insurers are encouraging care providers to shift these admissions to same-day visits. Facilitating early discharge for low-risk, outpatient PCI patients is an opportunity to decrease LOS and costs.
TR versus TF Access: Economic Substudies of Clinical Trials
Diagnostic Catheterization
A group of French operators randomized patients to right radial, left radial, or femoral access for diagnostic angiography. Overall costs were lower for the left radial versus both the right radial and femoral access groups (French franc (FF) 4,508 ± 991, FF 4,745 ± 1,332, FF 5,213 ± 2,672, P < 0.05).29 A group of US investigators conducted a retrospective analysis of patients undergoing a diagnostic catheterization procedure at a Veteran’s Administration hospital. They included all equipment and procedure time that was utilized for either radial or femoral approach. Radial access cases cost less money than both femoral access with MC and femoral access when a VCD was used ($369.5 ± $74.6 vs $446.9 ± $60.2, and $553.4 ± $81.0 [both P < 0.001]).30 The primary drivers of incremental cost included LOS and the cost of the VCD.
A large, single-center analysis showed that diagnostic radial procedures tended to cost about $10 more (related to costs of hemostatic bands versus MC for femoral procedures), but PCI procedures were $732 less when done from the radial route. The investigators concluded that there was $1,265 in cost savings per complication avoided in the TR group. With lower cost and less complications for the TR-PCI procedures, the radial approach was considered dominant (improved quality at a lower cost).31
TR-PCI
In a single-center clinical trial published in 2000, investigators collected cost data on patients undergoing PCI from both access routes. They assessed the relationship between TF-PCI with the use of a VCD and TR-PCI. In this nonrandomized study of 213 patients, they noted approximately $205 in savings favoring TR-PCI patients. Interestingly, about $122 of this difference was related to delayed discharge and complications, with the remaining $83 from differences in supply costs.32
In a retrospective analysis from a large database representing nearly 20% of all US hospitals, 609 TR-PCI cases were matched with over 60,000 TF cases.33 There was a savings of $553 (P = 0.033) favoring TR-PCI (total costs for TR-PCI were $11,736 ± $6,748 vs $12, 288 ± $23,418 for TF-PCI). As the patient’s risk of bleeding increased, there was a stronger economic argument in favor of the radial approach. Costs of care during the procedure day were similar; however, costs following the PCI until discharge were less in the radial patients, with 95% of the savings attributable to a shorter LOS (Fig. 26-1). In another study, Amin et al.34 also compared the costs and clinical outcomes between TR-PCI and TF-PCI at five US hospitals. They found that the radial approach was associated with a cost savings exceeding $800 per patient relative to the femoral approach.
Although these studies are limited by their nonrandomized and retrospective nature, they provide a current, real-life assessment of PCI practices in the United States.
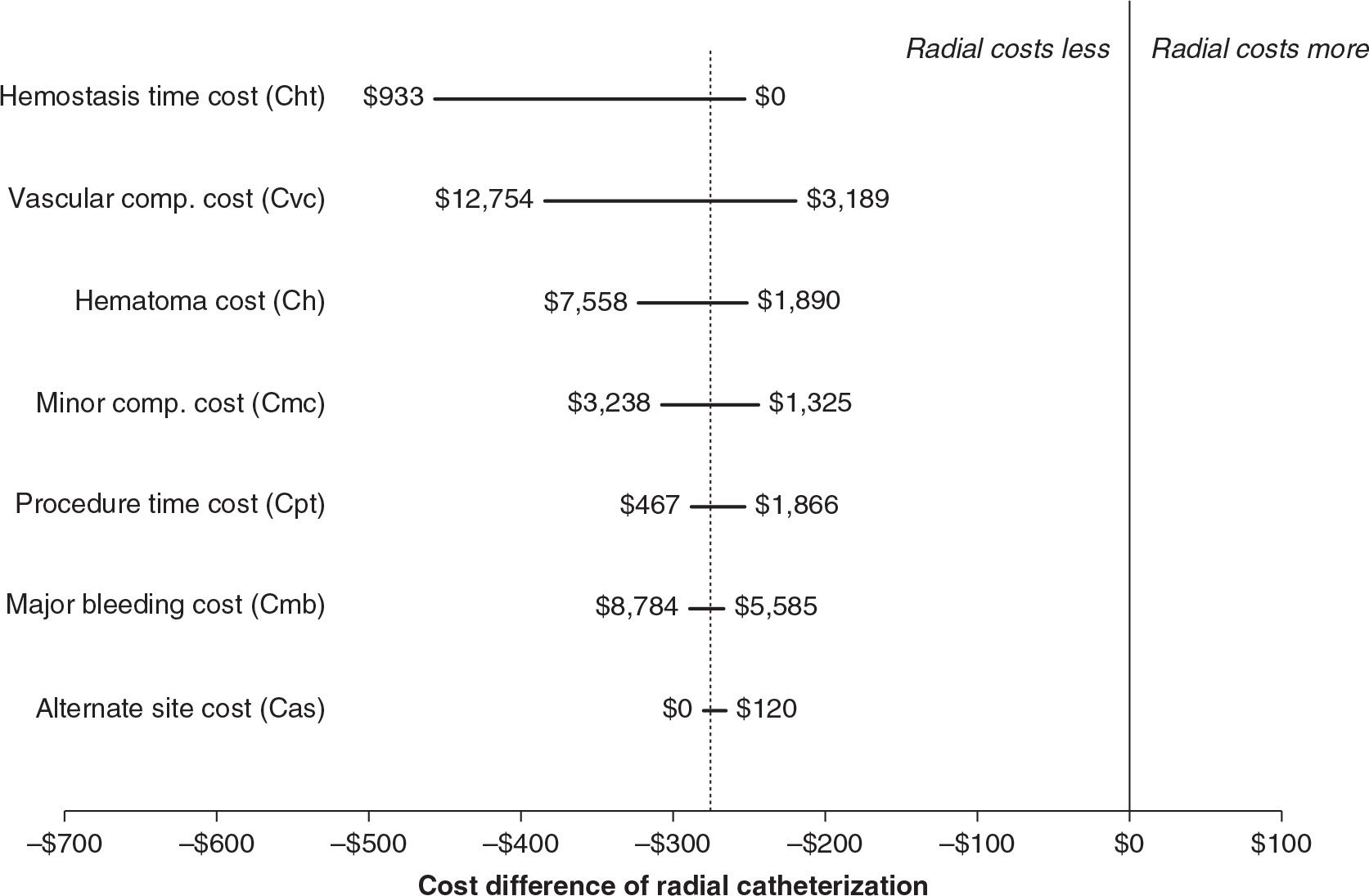
A systematic review of 14 randomized trials comparing radial and femoral accesses for diagnostic and therapeutic catheterizations employed a model to characterize the cost–benefit relationship. They included the cost of incremental procedure time and per-case costs of major complications. They noted that despite costing $1.52 more in procedure costs, radial catheterization led to an overall cost savings of $275 by decreasing the costs of complications as compared to TF procedures.35 In their sensitivity analyses, there were no scenarios where radial cost more than femoral catheterization (Fig. 26-2). On the basis of their model, the cost advantage of radial access would disappear only if radial procedures took 20 minutes longer than femoral or if femoral complications were reduced by 60%.
Ambulatory PCI Procedures
From these earlier studies, a consistent message emerged: LOS is a major driver of cost for elective PCI. Strategies that can safely reduce LOS will lead to decreased costs. From a historical perspective, PCI had been considered an inpatient procedure. Owing to the technological, pharmacologic, and technical advances, PCI has become much safer. In the United States, the majority of elective PCI procedures require a 1-day LOS.36 Several published studies have demonstrated the clinical efficacy and safety of same-day discharge in a selected group of low-risk, elective PCI patients.16,37,38
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


