where ΔP is the pressure gradient and V is the peak Doppler flow velocity in the main pulmonary artery. However, the peak instantaneous Doppler gradient may overestimate the peak-to-peak catheter gradient, presumably related to a pressure recovery phenomenon.
18.5 Technique (Step-by-Step)
1.
Candidates selection
The diagnosis and assessment of pulmonary valve stenosis are made by the usual clinical, radiographic, and echocardiographic data. An informed consent is obtained from the parents or the patients.
2.
Sedation and anesthesia
The procedure is usually performed under sedation. General anesthesia with endotracheal ventilation is needed in newborns, while it can be avoided beyond the neonatal period.
Heart rate, blood pressure, respiration, and pulse oximetry are continuously monitored throughout the procedure.
3.
Vascular access
The most preferred entry site for balloon dilation is the percutaneous femoral venous route. A sheath is inserted into the vein depending on the age and size of the patient (in newborns usually a 5-F sheath). In some high-risk patients an arterial line may be used to continuously monitor the arterial blood pressure. After sheath placement, heparin is given in the dose of 100 IU/kg, to keep the activated clotting time above 200 s.
4.
Right ventricular angiography
Hemodynamic assessment is done routinely, and the peak-to-peak catheter gradient across the pulmonary valve is assessed. Biplane right ventricular cineangiograms (posterior-anterior with cranial angulation and lateral views) are performed using Berman angiographic catheters or pigtail catheters to confirm the site of obstruction, to measure the pulmonary valve annulus, and to evaluate the function of right ventricle. The annulus is measured as the distance between the hinge points of the valve in both views in systole (Fig. 18.1).


Fig. 18.1
Right ventriculogram in left lateral view showing pulmonary valve stenosis; thickened, domed pulmonary valve; and poststenotic dilatation of the main pulmonary artery. The white line shows the length of the pulmonary valve annulus
5.
Positioning of the guidewire
An end-hole catheter is advanced across the pulmonary valve and the tip of the catheter positioned into the distal left (preferable) or right pulmonary artery.
Usually a Judkins right coronary or a cobra catheter is used. To allow the catheter to enter the RV, usually a pre-shaped stiff end of a straight standard guidewire is needed to guide the catheter across the tricuspid valve.
Alternatively a 4- or 5-F end-hole multipurpose catheter can be used. It is advanced up to the right atrium. Then a loop is created over the free wall of the right atrium with a gentle push. The next step is to rotate clockwise in order to direct the end of the catheter toward the tricuspid valve. Finally a gentle pull is applied in order to allow the catheter to slip in the right ventricle.
Then the catheter is oriented toward the RVOT with a clockwise rotation and a gentle pull. The catheter is passed through the valve.
Usually, this part of the procedure is not easy because of hypertrophy of the RV.
Floppy- and soft-tipped guidewires can be used to assist the catheter crossing of the pulmonary valve. Great attention is to be paid when using hydrophilic wires. In fact even a floppy-tipped wire can perforate.
In newborns a 0.014″ coronary wire or a 0.018″ hydrophilic wire can be used and positioned either distal in the pulmonary artery or in the descending aorta through the ductus arteriosus.
In older children 0.035″ wire can be chosen and placed distally in the pulmonary artery bed.
Wire position is crucial for the procedure!
A J-tipped, exchange length, stiff guidewire is advanced through the catheter already in place, and the catheter is removed. The selection of the exchange wire diameter is dependent upon the selected balloon catheter.
In newborns when the passage through the valve is a pinhole, predilation using a coronary balloon (diameter 2.5–3 mm; length 15–20 mm) may be needed.
6.
Selection of balloon catheter
The inflated diameter of the balloon is selected in accordance with the diameter of the pulmonary valve annulus. Usually a balloon diameter 1.0–1.2 times the annulus is chosen. The length of the balloon should be 20 in newborns and infants, 30 mm in children, and 40 mm in adolescents and adults. Longer balloons may impinge upon the tricuspid valve, causing heart block or tricuspid valve regurgitation. An adequately sized femoral sheath must be inserted for the introduction of the balloon catheter.
7.




Balloon dilation
The selected balloon angioplasty catheter is advanced over the guidewire and positioned across the pulmonary valve. The body landmarks, such as the ribs, sternum, or other fixed landmarks, are used for this purpose. A frozen video frame of the right ventricular cineangiogram displayed on the screen is used as a road map.
The balloon is quickly inflated with diluted contrast material (1 in 4) (Fig. 18.2). The inflation pressure is gradually increased up to the manufacturer’s recommendation (Fig. 18.3), and then the balloon is quickly deflated. The duration of inflation is kept as short as possible, usually just until after the waist disappears.

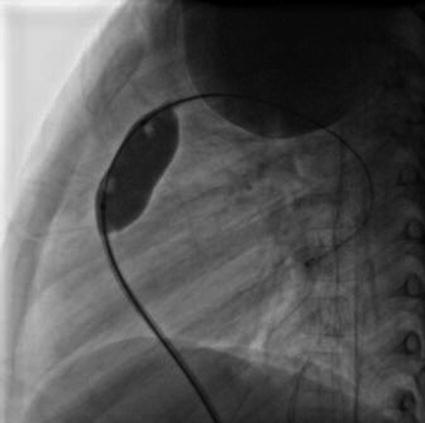

Fig. 18.2
Left lateral view of a partially inflated balloon catheter positioned across the pulmonary valve. As the balloon is inflated, a waist appears at the site of the pulmonary valve
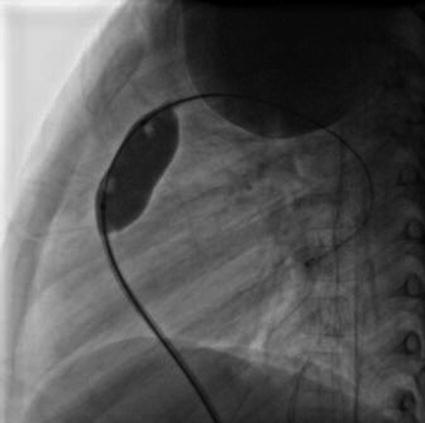
Fig. 18.3
Left lateral view of the balloon waist completely disappeared
If the balloon is not appropriately centered across the pulmonary valve or moves during the inflation, the position of the catheter is readjusted and balloon inflation repeated. Usually a gentle pull can be applied during full inflation in order to counteract the push forces of the right ventricle systole.
One additional balloon inflation may be performed after satisfactory balloon inflation has been achieved, to ensure adequate valvuloplasty.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


