Chapter 57
Pulmonary Embolism
1. Who first described pulmonary embolism?
3. What percentage of patients with acute PE have clinical evidence of lower extremity deep vein thrombosis (DVT)?
4. What percentage of patients with proximal DVT will develop PE?
Approximately 50% of patients with proximal DVT will develop PE.
5. What is the usual cause of death in subjects with PE?
6. What are the major risk factors for venous thromboembolism (VTE)?
Risk factors are crucial in raising suspicion for acute VTE, although the disease may be idiopathic. Previous thromboembolism, immobility, cancer, advanced age, major surgery, trauma, acute medical illness, and certain thrombophilias impart significant risk. A list of risk factors for VTE is shown in Box 57-1.
7. How commonly are recommended VTE prevention measures used?
8. How should a patient with suspected DVT be initially evaluated?
The symptoms and signs of DVT are nonspecific, and although clinical prediction rules can be useful, there should be a low threshold to proceed to compression ultrasonography. D-dimer testing may be useful; the diagnosis of DVT can be excluded without the need for ultrasound if the patient has a combination of a low or moderate clinical probability estimate and a negative D-dimer result. If the patient falls into the moderate or high clinical pretest probability or has a positive D-dimer test, further evaluation with ultrasound is advised. The enzyme-linked immunosorbent assay (ELISA)–based D-dimer tests have superior sensitivity (96% to 98%). DVT is discussed further in Chapter 50.
9. What are the symptoms and signs of acute PE?
 Dyspnea (either sudden in onset or evolving over days)
Dyspnea (either sudden in onset or evolving over days)
 Chest pain, often pleuritic (such chest pain may be associated with chest wall tenderness and generally occurs with pulmonary infarct)
Chest pain, often pleuritic (such chest pain may be associated with chest wall tenderness and generally occurs with pulmonary infarct)
 Hemoptysis (generally occurs with pulmonary infarct)
Hemoptysis (generally occurs with pulmonary infarct)
10. What are four clinical syndromes seen with acute PE?
 Massive PE with acute cor pulmonale: Not all patients with acute cor pulmonale will go on to develop hypotension (which defines massive PE), but such a presentation should raise concern.
Massive PE with acute cor pulmonale: Not all patients with acute cor pulmonale will go on to develop hypotension (which defines massive PE), but such a presentation should raise concern.
 Submassive PE: This is defined as acute PE which causes RV dysfunction. Of note, based upon the Pulmonary Embolism Severity Index (see Question 19), low-risk and intermediate-risk categories have been referred to as “nonmassive PE.”
Submassive PE: This is defined as acute PE which causes RV dysfunction. Of note, based upon the Pulmonary Embolism Severity Index (see Question 19), low-risk and intermediate-risk categories have been referred to as “nonmassive PE.”
 Pulmonary infarction and/or pulmonary hemorrhage: Because of dual blood supply and free anastomosis between the pulmonary capillaries, emboli usually don’t cause infarction in a healthy lung. Pulmonary infarction is uncommon when emboli obstruct central arteries but much more common when distal arteries are occluded. Obstruction of distal arteries can result in pulmonary hemorrhage as a result of an influx of bronchial arterial blood at systemic pressure. Hemorrhage causes symptoms and radiographic changes usually attributed to pulmonary infarction.
Pulmonary infarction and/or pulmonary hemorrhage: Because of dual blood supply and free anastomosis between the pulmonary capillaries, emboli usually don’t cause infarction in a healthy lung. Pulmonary infarction is uncommon when emboli obstruct central arteries but much more common when distal arteries are occluded. Obstruction of distal arteries can result in pulmonary hemorrhage as a result of an influx of bronchial arterial blood at systemic pressure. Hemorrhage causes symptoms and radiographic changes usually attributed to pulmonary infarction.
 Acute unexplained dyspnea: A diagnosis of PE should be considered in patients with dyspnea of unclear cause and may merit consideration even when there is another potential explanation.
Acute unexplained dyspnea: A diagnosis of PE should be considered in patients with dyspnea of unclear cause and may merit consideration even when there is another potential explanation.
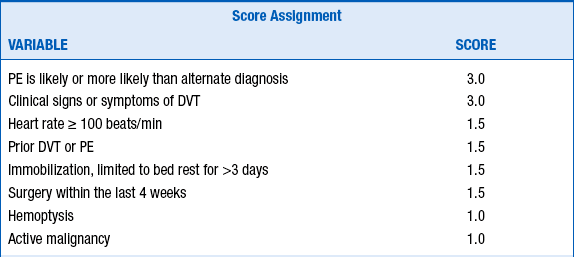
11. What is the Wells score for suspected acute PE?
First described in 1998, the Wells score is a clinical prediction score based on simple, noninvasive clinical parameters. It has evolved over the years, has been validated, and is useful in determining pretest probability for suspected acute PE. Pretest probability can be defined based on the calculated score from the modified Wells score (Table 57-1). PE has ultimately been classified as “unlikely” if the clinical decision score was 4 or less, and “likely” with a score of more than 4 points. This cutoff was chosen because it has been shown to give an acceptable VTE diagnostic failure rate of 1.7% to 2.2% when in combination with a normal D-dimer test result. Moreover, with a score of 4 or less and a negative D-dimer test, no further testing appears to be necessary. A score greater than 4 requires further evaluation, and computed tomographic angiography (CTA) is usually performed. High clinical suspicion, however, should always take precedence, even if the Wells score is low.