10 Pulmonary Atresia and Intact Ventricular Septum
I. CASE
A. Fetal echocardiography findings
1. The fetal echo reveals situs solitus of the atria, levocardia, left aortic arch, and heart rate of 142 bpm.
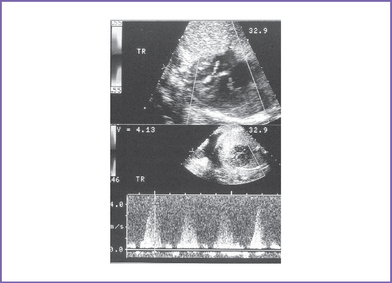
2. The four-chamber view is abnormal, with a small right ventricle (RV), which is hypertrophied and has reduced systolic function, and a dilated right atrium (RA) (Fig. 10-1).
3. Cardiac axis and position are normal.
4. Cardiac size is increased (cardiothoracic ratio = 0.40).
5. The outflow assessment reveals normally related great arteries with significant asymmetry (aorta–to–pulmonary artery diameter ratio = 1:0.5).
6. The pulmonary valve is atretic, with no antegrade flow in systole and no pulmonary insufficiency.
7. There are good-sized confluent branch pulmonary arteries.
8. The tricuspid valve diameter is small (0.24 cm) (z score = −3), with normal inflow waves (E/A waves).
9. A narrow jet of tricuspid regurgitation (4 m/s) and a dP/dt (change in pressure per change in time) of 600 mm Hg per second.
10. There are possible RV coronary sinusoids.
11. The aortic arch is leftward, with normal antegrade flow.
12. The ductal arch shows flow reversal in systole.
13. There is unrestricted flow through the foramen ovale, with a right- to-left shunt.
14. The pulmonary venous flow pattern is normal. There is also normal flow in the inferior vena cava (IVC), ductus venosus, and umbilical vein.
15. The left ventricular (LV) Tei index (myocardial performance index) is normal to mildly increased (0.48). The RV Tei index could not be calculated due to the pulmonary atresia.
D. Fetal management and counseling
1. Amniocentesis should be offered, although chromosomal anomalies are unlikely with pulmonary atresia with intact ventricular septum.
2. Follow-up includes serial antenatal studies at 4-week intervals.
a. Assess RV size and function and endocardial fibroelastosis.
b. Look for congestive heart failure (CHF), which can develop if there is:
d. Assess the growth of pulmonary arteries and branches. Ductal flow has already been shown to be reverse of normal due to the atretic pulmonary valve.
a. Conditions for vaginal delivery.
b. Conditions for cesarean delivery.
c. Cesarean section practice varies with institution preference.
E. Neonatal management
a. Administer prostaglandin E1 (PGE1) infusion to keep the ductus open to increase pulmonary blood flow and raise arterial oxygen saturation.
b. Oxygen administration can increase oxygen saturation by decreasing pulmonary venous regurgitation and increasing blood flow.
c. Therapeutic balloon atrial septostomy should be performed in the rare situation of restrictive patent foramen ovale.
d. Cardiac catheterization and angiography are recommended to demonstrate coronary sinusoids (by RV angiogram) and rule out coronary artery anomalies such as stenosis. In many pediatric cardiac centers, radiofrequency perforation of the RV outflow tract (RVOT) is possible at cardiac catheterization, eliminating the need for surgery when the RV can otherwise sustain sufficient pulmonary circulation.
F. Follow-up
None of the surgical procedures is curative.
1. Patients who had a Fontan operation.
a. Arrhythmia, reduced heart function, and neurodevelopmental problems are possible sequelae.
b. Women who have undergone the Fontan procedure can become pregnant.
c. Transplantation is a possibility in young adult life if LV dysfunction develops.
2. For patients who had RVOT reconstruction and two-ventricle repair, surgery might be necessary for recurrent RV outflow obstruction or conduit replacement.
G. Risk of recurrence
1. When there is a previous baby with the same condition, this rare congenital heart defect may be an autosomal recessive trait.
2. In the absence of positive family history and normal karyotype, including FISH for 22q11.2, we assume a multifactorial inheritance, and hence the estimated recurrence risk is around 2%.
H. Outcome of this case
1. The baby was born at term with good Apgar scores and good weight.
2. Moderate cyanosis was noted at birth (pulse oximeter reading was 76%-82%).
3. Prostaglandin E1 (PGE1) infusion was started.
4. Postnatal echocardiography confirmed the diagnosis of pulmonary atresia, moderate tricuspid regurgitation, and intact ventricular septum.
5. The pulmonary arteries were of good size and had confluent pulmonary artery branches.
6. The foramen ovale and ductus arteriosus were patent and good sized, with left-to-right shunting.
7. There was retrograde flow in the left anterior descending artery and the left main coronary artery, and there was evidence of a proximal left main coronary artery stenosis.
8. Cardiac catheterization confirmed the presence of RV-dependant coronary circulation. The presence of RV-dependant coronary circulation made a univentricular repair the only surgical option.
9. The infant had a palliative A-P shunt at day 5 of postnatal life.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree