Chapter 32
Prosthetic Heart Valves
1. What are important considerations in the preoperative evaluation and planning of patients who are to undergo valve repair or replacement?
2. What types of prosthetic valves are used for valve replacement, and which ones are most commonly used in current practice?
Representative bioprosthetic and mechanical heart valve types are shown in Figure 32-1 and discussed here.
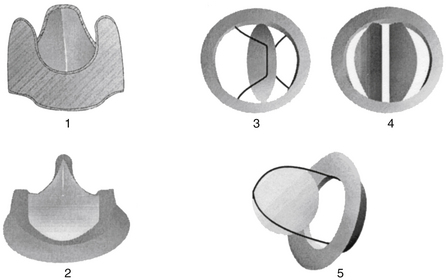
Figure 32-1 Bioprosthetic and mechanical heart valves. (1) Biologic nonstented and (2) stented valves; (3) mechanical single tilting disc valve, (4) mechanical bileaflet valve, and (5) ball-in-cage valve.
A stentless bioprosthesis is a bovine or porcine heart valve implanted without a frame. In the aortic position, the aortic root is used to attach the valve. The major advantage is that the size of the implanted valve can be larger, because no space is required for a supporting frame. Data suggest that left ventricular function is better protected by nonstented compared with stented valves. Anticoagulation is recommended for the first 3 months after implantation.
Transcatheter aortic valve implantation (TAVI) or transcatheter aortic valve replacement (TAVR) has been performed at investigational sites for nearly 10 years, mostly commonly in Europe. In the United States, it has recently been approved, though programs that can implant such valves must meet strict standards. It is intended for patients with severe aortic stenosis who are not good surgical candidates for conventional valve replacement. The valve is implanted via a transarterial (femoral or axillary) or transapical approach. In Europe, the valve may also be implanted by a direct aortic approach. Significant risks of serious adverse events, such as valve displacement, cardiac tamponade, myocardial infarction, stroke, or injury of the aorta or femoral or axillary artery, are associated with this procedure. The procedure is illustrated in Figure 32-2.

Figure 32-2 Transcatheter aortic valve replacement. After balloon valvuloplasty of the stenotic aortic valve, the prosthetic valve is positioned at the level of the aortic annulus. The balloon is inflated, deploying the stented valve in position.
3. What is a heterograft, and what is an allograft (homograft), and what is a Ross procedure?
A heterograft is a biologic valve derived from an animal. An allograft (also called a homograft) is a heart valve taken from a human cadaver. Allografts have the advantage of natural configuration and the fact that they include a portion of the aortic root that can be incorporated in the valve replacement procedure if necessary (e.g., aortic root abscess). Careful matching of allograft size to the patient is critical to the performance and durability of the valve. The Ross procedure uses the patient’s own pulmonic valve to replace their aortic valve. The pulmonic valve is then replaced with a bioprosthesis. Advantages are a lack of antigenicity and the potential for growth of the valve over time, as required in children.
4. How does one choose between bioprosthetic and mechanical valves?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


