Little is known about the prognostic value of ST-segment depression and/or T wave (ST-T abnormalities) with or without left high R waves on electrocardiogram recorded at rest for death from cardiovascular disease (CVD) in Asian populations. Japanese participants without a history of CVD and free of major electrocardiographic (ECG) abnormalities were followed for 24 years. Subjects were divided into 4 groups based on baseline ECG findings: isolated left high R waves, isolated ST-T abnormalities, ST-T abnormalities with left high R waves, and normal electrocardiogram. Cox proportional hazard model was used to estimate risk of CVD mortality in groups with ECG abnormalities compared to the normal group. Of 8,572 participants (44.4% men, mean age 49.5 years; 55.6% women, mean age 49.4 years), 1,142 had isolated left high R waves, 292 had isolated ST-T abnormalities, and 128 had ST-T abnormalities with left high R waves at baseline. Multivariable-adjusted hazard ratios of ST-T abnormalities with left high R waves for CVD mortality were 1.95 (95% confidence interval 1.25 to 3.04) in men and 2.68 (95% confidence interval 1.81 to 3.97) in women. Isolated ST-T abnormalities increased the risk for CVD death by 1.66 times (95% confidence interval 1.01 to 2.71) in men and 1.62 times (95% confidence interval 1.18 to 2.24) in women. Association of ECG abnormalities with CVD mortality was independent of age, body mass index, systolic blood pressure, serum cholesterol, blood glucose, smoking and drinking, and antihypertensive medication. In conclusion, ST-T abnormalities with or without left high R waves on electrocardiogram recorded at rest constitute an independent predictor of CVD mortality in Japanese men and women.
The standard electrocardiogram recorded at rest is the most widely used noninvasive tool for assessing cardiovascular risk in epidemiologic studies and clinical practice. ST-segment depression and/or an inverse or flat T wave (ST-T abnormalities) are the most sensitive changes on electrocardiogram. In addition, left high R-wave electrocardiographic (ECG) manifestation of left ventricular hypertrophy (LVH) is often seen in association with ST-T abnormalities. Several epidemiologic studies have reported that LVH with ST-T abnormalities increase cardiovascular disease (CVD) risk. However, these studies investigating the prognostic value of ST-T abnormalities and left high R waves were performed predominantly in Western populations. Information about the prognostic value of ST-T abnormalities in the presence or absence of left high R waves is meager in Asian populations that have a higher stroke rate and lower incidence of coronary heart disease (CHD). In a population with a markedly lower coronary mortality, such as the Japanese, the benefit of ECG screening may be different from Western populations. The aim of the present study was to assess the independent prognostic value of ST-T abnormalities with or without left high R waves for mortality from CVD and its subtypes in a large cohort of participants selected randomly from the overall Japanese population.
Methods
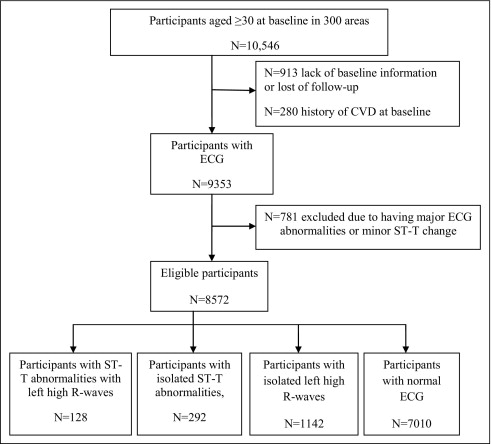
The dataset of the cohort study of the National Survey on Circulatory Disorders comprising the National Integrated Project for Prospective Observation of Non-Communicable Disease and its Trends in the Aged (NIPPON DATA) was used. The present study analyzed data from NIPPON DATA80, in which a baseline survey was performed in 1980. Details of this cohort have been reported elsewhere. In brief, 300 areas were selected by stratified random sampling and all residents ≥30 years old in these areas were invited to participate. In total 10,546 residents (4,639 men and 5,907 women) participated in the survey (response rate 76.6%). Baseline surveys were carried out at local public health centers. Participants were followed for 24 years until November 2004.
In this present study, we excluded participants who had a history of CHD or stroke at baseline (n = 280), missing information at baseline, or were lost to follow-up (n = 913). In addition, participants with baseline ECG abnormalities (n = 781) including third-degree atrioventricular block (Minnesota Code [MC] 6.1), second-degree atrioventricular block (MC 6.2), Wolf-Parkinson-White syndrome (MC 6.4), complete left bundle branch block (MC 7.1), complete right bundle branch block (MC 7.2), minor ST segment (MC 4.4), nonspecific T-wave abnormalities (MCs 5.4 to 5.5), atrial fibrillation (MC 8.3), Q-wave evidence of myocardial infarction (MC 1.1), ventricular tachycardia (MC 8.2), supraventricular tachycardia (MC 8.4), and atrioventricular nodal delay (MC 8.6) were excluded. Consequently, the remaining 8,572 participants (3,808 men and 4,764 women) were included in the analysis ( Figure 1 ).
Information on a history of CVD and diabetes, baseline use of antihypertensive medications, and smoking and drinking habits were obtained from interviews by public health nurses. Nonfasting blood samples were drawn and centrifuged within 60 minutes of collection. Casual glucose concentration was measured by the cupric-neocuproine method. The glucose concentration obtained by the cupric-neocuproine method was corrected by an equation to the value that would have been measured by the glucose-oxidase method, which is the correct standard. Serum total cholesterol was measured by an auto analyzer (SMA 12/60; Technicon, Tarrytown, New York) in 1 specific laboratory (Osaka Medical Center for Health Science and Promotion, Osaka, Japan). Since 1975, the laboratory has been certified by the Centers for Disease Control and Prevention/National Heart, Lung, and Blood Institute Lipid Standardization Program by Center for Disease Control and Prevention (Centers for Disease Control and Prevention, Atlanta, Georgia) for precision and accuracy of cholesterol measurements. Baseline blood pressure was measured in each subject after 5 minutes of rest in a seated position. The measurement was performed by trained public health nurses at each public health center using a standard mercury sphygmomanometer placed on the right arm. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, use of antihypertensive agents, or any combination of these. Body height in stocking feet and body weight in light clothing were measured and body mass index was calculated as body weight (kilograms) divided by square of body height (meters). Frequency of drinking per week and average number of cigarettes per day were assessed using questionnaires.
During the baseline survey, a standard 12-lead electrocardiogram was recorded in the supine position. Each electrocardiogram was read 2 times by 2 different researchers according to MC criteria, which was developed to document significant ECG pattern changes using objective criteria. Codes in agreement were accepted, whereas inconsistent codes were decided by a panel of study epidemiologists and cardiologists. Participants were categorized into 4 groups according to ECG findings: (1) isolated left high R waves (MCs 3.1 and 3.3); (2) isolated ST-T abnormalities (MCs 4.1 to 4.3 and/or MCs 5.1 to 5.3); (3) ST-T abnormalities with left high R waves (MCs 3.1 and 3.3 with MCs 4.1 to 4.3 and/or MCs 5.1 to 5.3); and (4) normal ECG findings. Electrocardiogram was classified as normal in the absence of left high R waves and ST-T abnormalities.
During the 24-year follow-up, we used the National Vital Statistics database of Japan to identify underlying causes of deaths of participants who died during follow-up by date of birth, gender, date of death, and area code of place of death with permission from the Management and Coordination Agency, Government of Japan. Underlying causes of death were coded according to the International Classification of Disease, Ninth Revision through the end of 1994 and the International Classification of Disease, 10th Revision from the beginning of 1995. Details of classification used in the present study are described elsewhere. CVD (ninth revision codes 393 to 459 and 10th revision codes I00 to I99), CHD (ninth revision codes 410 to 414 and 10th revision codes I20 to I25), and stroke (ninth revision codes 430 to 438 and 10th revision codes I60 to I69) were identified. Approval for the study was obtained from the institutional review board of Shiga University of Medical Science (No. 12-18, 2000).
We used analysis of variance for continuous variables and chi-square test for categorical variables to compare baseline characteristics among the 4 participant groups. Outcome events studied were CVD, CHD, and stroke mortality. We used Cox proportional hazards models to estimate hazard ratios (HRs) with 95% confidence intervals of mortality for presence of isolated left high R waves, isolated ST-T abnormalities, and ST-T abnormalities with left high R waves compared to normal ECG findings, which served as the reference category. Separate analyses were carried out for CVD, CHD, and stroke. In multivariable models, we included traditional cardiovascular risk factors as potential confounding factors, namely age at study entry, body mass index, systolic blood pressure, serum total cholesterol, blood glucose, history of smoking (never, current, ex-smoker) and alcohol drinking (never, current, ex-drinker), and antihypertensive medication (yes, no) as confounding factors. These covariates were considered in multivariable models based on clinical judgment and statistical significance based on univariate analysis. Models in which gender was combined were also adjusted for gender. Performance of multivariable models was quantified by Harrell concordance statistics (c-index), a generalization of the area under the receiver operating characteristic curve that allows for censored data. Calibration was assessed graphically by plotting the predicted probability (using the full model) against actual probability (observed in our cohort) across 10 decile categories based on predicted risk.
Results
Baseline characteristics of participants (men and women) who had ST-T abnormalities with left high R waves, isolated ST-T abnormalities, isolated left high R waves, and normal electrocardiogram are listed in Table 1 . Age, systolic and diastolic blood pressures, blood glucose, serum cholesterol, drinking habit, and use of antihypertensive medication were significantly different among the 4 groups for women and men.
| Normal Electrocardiogram | ST-T Abnormalities With Left High R Waves | Isolated ST-T Abnormalities | Isolated Left High R Waves | p Value | |
|---|---|---|---|---|---|
| Men | |||||
| Number | 2,854 | 68 | 58 | 828 | |
| Age (years) | 48.5 ± 12.6 | 62.03 ± 12.8 | 60.9 ± 15.6 | 48.7 ± 12.2 | <0.001 |
| Systolic blood pressure (mm Hg) | 134.7 ± 18.6 | 167.9 ± 27.1 | 154.2 ± 25.7 | 142.7 ± 21.3 | <0.001 |
| Diastolic blood pressure (mm Hg) | 82.1 ± 11.6 | 90.7 ± 15.6 | 87.9 ± 14.3 | 86.1 ± 12.7 | <0.001 |
| Body mass index (kg/m 2 ) | 22.9 ± 2.5 | 23.8 ± 2.8 | 22.3 ± 3.5 | 23.6 ± 3.1 | 0.874 |
| Serum total cholesterol (mg/dl) | 185.9 ± 32.6 | 180.3 ± 30.9 | 192.1 ± 27.5 | 185.7 ± 32.7 | 0.024 |
| Blood glucose (mg/dl) | 129.5 ± 37.6 | 157.1 ± 61.5 | 150.02 ± 49.4 | 128.2 ± 33.6 | <0.001 |
| Current smoker | 62.6% | 63.2% | 69.0% | 65.1% | 0.239 |
| Current drinker | 72.8% | 64.7% | 63.8% | 83.3% | <0.001 |
| Antihypertensive drug | 7.0% | 44.1% | 32.8% | 10.4% | <0.001 |
| Women | |||||
| Number | 4,156 | 60 | 234 | 314 | |
| Age (years) | 48.4 ± 12.6 | 64.6 ± 12.2 | 57.8 ± 14.1 | 53.6 ± 12.5 | <0.001 |
| Systolic blood pressure (mm Hg) | 131.04 ± 20.1 | 161.6 ± 29.1 | 144.2 ± 22.4 | 142.0 ± 21.4 | <0.001 |
| Diastolic blood pressure (mm Hg) | 78.6 ± 11.4 | 88.6 ± 16.0 | 83.3 ± 12.7 | 82.2 ± 12.5 | <0.001 |
| Body mass index (kg/m 2 ) | 22.8 ± 3.3 | 22.9 ± 4.2 | 23.9 ± 3.7 | 22.1 ± 3.01 | 0.005 |
| Serum total cholesterol (mg/dl) | 189.6 ± 33.6 | 196.4 ± 37.6 | 200.6 ± 33.8 | 188.8 ± 35.2 | 0.041 |
| Blood glucose (mg/dl) | 127.5 ± 33.5 | 162.1 ± 78.3 | 141.03 ± 40.2 | 130.2 ± 32.4 | <0.001 |
| Current smoker | 8.8% | 16.7% | 9.0% | 8.9% | 0.445 |
| Current drinker | 20.6% | 15% | 14.1% | 21.3% | 0.042 |
| Antihypertensive drug | 8.3% | 43.3% | 23.1% | 18.2% | <0.001 |
During a total follow-up period of 181,545 person-years (average 21.2 years), there were 2,244 deaths among participants including 750 deaths from all CVDs, 149 deaths from CHD, and 353 deaths from stroke.
Table 2 lists age-adjusted and multivariable-adjusted HRs for deaths from all CVDs in the 4 groups that were stratified based on ECG abnormalities. Participants who had ST-T abnormalities with left high R waves and those with isolated ST-T abnormalities had a higher risk for CVD mortality compared to the normal ECG group in men and women. In participants who had ST-T abnormalities with left high R waves, multivariable-adjusted HRs for CVD mortality were 1.95 in men and 2.68 in women. In participants who had isolated ST-T abnormalities, multivariable-adjusted HRs for deaths from CVD were 1.66 in men and 1.62 in women.
| All CVD Mortalities | ||||
|---|---|---|---|---|
| Normal Electrocardiogram | ST-T Abnormalities With Left High R Waves | Isolated ST-T Abnormalities | Isolated Left High R Waves | |
| Men | ||||
| Number | 2,854 | 68 | 58 | 828 |
| Cardiovascular disease death | 254 | 25 | 19 | 77 |
| Mortality (per 1,000 person-years) | 4.3 | 27.4 | 24.4 | 4.5 |
| Age-adjusted hazard ratio | 1.00 | 2.99 (1.97–4.53) | 2.49 (1.55–3.98) | 1.14 (0.88–1.46) |
| Multivariable-adjusted hazard ratio | 1.00 | 1.95 (1.25–3.04) | 1.66 (1.01–2.71) | 1.02 (0.78–1.33) |
| Women | ||||
| Number | 4,156 | 60 | 234 | 314 |
| Cardiovascular disease death | 268 | 30 | 46 | 31 |
| Mortality (per 1,000 person-years) | 2.9 | 37.5 | 10.4 | 4.7 |
| Age-adjusted hazard ratio | 1.00 | 3.09 (2.10–4.55) | 1.66 (1.21–2.28) | 1.12 (0.77–1.62) |
| Multivariable-adjusted hazard ratio | 1.00 | 2.68 (1.81–3.97) | 1.62 (1.18–2.24) | 0.997 (0.68–1.46) |
| Total participants | ||||
| Number | 7,010 | 128 | 292 | 1,142 |
| Cardiovascular disease death | 522 | 55 | 65 | 108 |
| Mortality(per 1,000 person-years) | 3.5 | 32.1 | 12.5 | 4.6 |
| Age- and gender-adjusted hazard ratio | 1.00 | 3.07 (2.32–4.08) | 1.89 (1.45–2.45) | 1.14 (0.92–1.40) |
| Multivariable-adjusted hazard ratio | 1.00 | 2.27 (1.69–3.04) | 1.59 (1.23–2.08) | 1.04 (0.84–1.29) |
For all participants, multivariable-adjusted HRs of CHD mortality for presence of ST-T abnormalities with left high R waves and of isolated ST-T abnormalities were significantly higher compared to the normal ECG group ( Table 3 ). In men, age-adjusted HR of CHD mortality was significantly higher in participants who had ST-T abnormalities with left high R waves and in those who had isolated ST-T abnormalities; however, multivariable adjustment attenuated the significance. In women, multivariable-adjusted HR of CHD mortality for ST-T abnormalities with left high R waves was 2.62 and that for isolated ST-T abnormalities was 2.39.
| CHD Mortality | ||||
|---|---|---|---|---|
| Normal Electrocardiogram | ST-T Abnormalities With Left High R Waves | Isolated ST-T Abnormalities | Isolated Left High R Waves | |
| Men | ||||
| Number | 2,854 | 68 | 58 | 828 |
| Coronary heart disease death | 50 | 5 | 4 | 16 |
| Mortality (per 1,000 person-years) | 0.8 | 5.5 | 5.1 | 0.9 |
| Age-adjusted hazard ratio | 1.00 | 3.64 (1.43–9.27) | 3.14 (1.12–8.82) | 1.17 (0.67–2.06) |
| Multivariable-adjusted hazard ratio | 1.00 | 2.40 (0.89–6.44) | 1.80 (0.61–5.29) | 1.05 (0.59–1.88) |
| Women | ||||
| Number | 4,156 | 60 | 234 | 314 |
| Coronary heart disease death | 51 | 5 | 12 | 6 |
| Mortality (per 1,000 person-years) | 0.6 | 6.3 | 2.7 | 0.9 |
| Age-adjusted hazard ratio | 1.00 | 2.93 (1.15–7.49) | 2.42 (1.28–4.58) | 1.15 (0.49–2.68) |
| Multivariable-adjusted hazard ratio | 1.00 | 2.62 (1.02–6.76) | 2.39 (1.25–4.59) | 1.03 (0.44–2.43) |
| All participants | ||||
| Number | 7,010 | 128 | 292 | 1,142 |
| Coronary heart disease death | 101 | 10 | 16 | 22 |
| Mortality (per 1,000 person-years) | 0.7 | 5.8 | 3.1 | 0.9 |
| Age- and gender-adjusted hazard ratio | 1.00 | 3.36 (1.74–6.52) | 2.66 (1.55–4.58) | 1.19 (0.74–1.89) |
| Multivariable-adjusted hazard ratio | 1.00 | 2.48 (1.26–4.91) | 2.10 (1.20–3.66) | 1.10 (0.69–1.77) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


