It has been reported that increased levels of C-reactive protein are related to adverse long-term prognosis in the setting of ST-segment elevation acute myocardial infarction (MI). In previous studies, the timing of C-reactive protein determination has varied widely. In the present study, serial high-sensitivity C-reactive protein (hsCRP) measurements were performed to investigate if any of the measurements is superior regarding long-term prognosis. A total of 861 consecutive patients admitted for ST-segment elevation MI and treated with intravenous thrombolysis within the first 6 hours from the index pain were included. HsCRP levels were determined at presentation and at 24, 48, and 72 hours. The median follow-up time was 3.5 years. New nonfatal MI and cardiac death were the study end points. By the end of follow-up, cardiac death was observed in 22.4% and nonfatal MI in 16.1% of the patients. HsCRP levels were found to be increasing during the first 72 hours. Multivariate Cox regression analysis demonstrated that hsCRP levels at presentation were an independent predictor of the 2 end points (relative risk [RR] 2.8, p = 0.002, and RR 2.1, p = 0.03, for MI and cardiac death, respectively), while hsCRP levels at 24 hours did not yield statistically significant results (RR 1.4, p = 0.40, and RR 1.1, p = 0.80, for MI and cardiac death, respectively). The corresponding RRs at 48 hours were 1.2 (p = 0.5) for MI and 3.2 (p = 0.007) for cardiac death and at 72 hours were 1.6 (p = 0.30) for MI and 3.9 (p <0.001) for cardiac death. In conclusion, hsCRP levels at presentation represent an independent predictor for fatal and nonfatal events during long-term follow-up. HsCRP levels at 48 and 72 hours, which are close to peak hsCRP levels, independently predict only cardiac death.
It seems that elevated levels of circulating inflammatory markers, especially C-reactive protein (CRP), bear prognostic information and may contribute to the long-term risk stratification of patients with acute coronary syndromes (ACS). However, there is now considerable evidence suggesting that it may not be possible to address ACS collectively. Because they constitute a heterogenous group, they also may demonstrate different CRP kinetics. This observation appears reasonable, as CRP might represent ≥2 different inflammatory components that vary within the spectrum of acute ischemia: the preexisting low-grade vascular inflammation and the acute phase response to myocardial injury and/or necrosis. The former is measurable at the beginning and the latter builds up as ischemic injury evolves, while interventions such as reperfusion may also alter the course of CRP. In this context, we attempted in the present study to investigate CRP kinetics as well as to prospectively evaluate the long-term prognostic significance of high-sensitivity CRP (hsCRP) measured at different prespecified time points through the course of ST-segment elevation acute myocardial infarction (STEMI) in a relatively large and homogenous cohort of patients treated with thrombolysis.
Methods
Consecutive eligible patients admitted to our hospital for STEMI and treated with thrombolytic therapy from September 2000 to December 2003 were included in the present study. Eligible patients required to have (1) continuous chest pain upon presentation, refractory to nitrates, lasting ≥30 minutes, (2) ST-segment elevation ≥0.2 mV in ≥2 contiguous precordial leads or ≥0.1 mV in ≥2 contiguous limb leads or new (or presumably new) left bundle branch block on admission electrocardiography, and (3) presentation and thrombolytic regimen administration within the first 6 hours of index pain. Patients with (1) angina of secondary origin, (2) active infection or chronic inflammatory diseases, (3) significant hepatic or renal dysfunction, (4) malignancy, and (5) history of myocardial infarction (MI), coronary revascularization, or major surgery within the previous month were excluded. The study complied with the Declaration of Helsinki, the ethics committee of the hospital approved the research protocol, and informed consent was obtained from all participants.
Either streptokinase or a fibrin-specific fibrinolytic agent (alteplase, reteplase, or tenecteplase) was used. All patients received chewed aspirin in a dose of 500 mg on presentation, and it was continued orally in a dose of 100 to 325 mg/day indefinitely. Heparin was given in a bolus dose of 5,000 U on admission in all patients, followed by intravenous infusion titrated to a therapeutic activated partial thromboplastin time. Heparin was continued in uncomplicated cases for 48 hours, followed by subcutaneous administration of enoxaparin (1 mg/kg/12 hours). Clopidogrel was not routinely administered at the time the study began. Further medical therapy, including β blockers, nitrates, angiotensin-converting enzyme inhibitors, glycoprotein IIb/IIIa inhibitors, and statins, was left at the discretion of the attending physician, who was unaware of the study protocol. Before discharge, all patients were advised for smoking cessation, body weight reduction, regular exercise, and lipid monitoring.
The Eagle 4,000 monitor (GE Marquette Medical Systems, Milwaukee, Wisconsin) was connected to each patient immediately after admission to the coronary care unit. ST-segment recording was started with the first acquired electrocardiogram and continued for ≥24 hours using the ST Guard system (GE Marquette Medical Systems). The operation of this system has been described previously. In the present study, the absence of abrupt and sustained >50% ST-segment recovery from the last updated reference electrocardiogram in the first 90 minutes after the start of intravenous thrombolysis was used to define failed reperfusion. All ST-segment trends were analyzed off-line by a well-trained investigator blinded to the patients’ clinical and biochemical data.
In-hospital and postdischarge follow-up data were prospectively collected on predesigned case report forms. After discharge, patients were followed up at 30 days and subsequently every 6 months for a period of ≥3 years, on an outpatient basis or by telephone interview. The prespecified end points of the present study were new nonfatal MI and cardiac death within the follow-up period. New nonfatal MI was defined as a new episode of chest pain ≥30 minutes in duration, resulting in rehospitalization, with new electrocardiographic changes (ST-T changes or new Q waves, or both, in ≥2 contiguous leads) and an increase in plasma levels of either creatine kinase-MB (≥2 times normal) or cardiac troponin I or T (>99th percentile of normal). Cardiac death was defined as sudden unexplained death, death due to fatal MI, or death after rehospitalization because of heart failure or possible acute myocardial ischemia. The diagnosis of clinical outcomes was verified by review of death certificates, discharge medical reports, hospital records, or contact with the attending physicians. Events were adjudicated by a committee blinded to other patient information.
Venous blood samples were obtained at prespecified time points: at presentation and at 24, 48, and 72 hours from presentation. Coded serum samples were stored at −80°C until batch analysis at the end of the study. Hs-CRP was measured using a highly sensitive nephelometric method (BNII; Dade Behring, Inc., Marburg, Germany) with a lower detection limit of 0.1 mg/L.
Normally distributed continuous variables are expressed as mean ± SD and categorical variables as percentages. Normal distribution was evaluated using the Kolmogorov-Smirnov test. Continuous variables were compared using Student’s t test or the Mann-Whitney U test as appropriate. Associations of dichotomous variables were tested using chi-square or Fisher’s exact tests as appropriate. The predictive effect of hsCRP was evaluated with univariate and multivariate Cox regression models. All hsCRP values were log transformed. All tests were 2 tailed, and p values <0.05 were considered significant. Statistical analysis was performed using SPSS release 17.0 (SPSS, Inc., Chicago, Illinois).
Results
A total of 902 patients with STEMIs were treated during the period of enrollment, and 872 received intravenous thrombolysis. Eleven were excluded (4 patients with active infection, 4 with known chronic inflammatory disease, 2 with renal failure under hemodialysis, and 1 with diagnosed malignancy). Thus, 861 patients with STEMI treated with thrombolysis were included in the present analysis. Baseline characteristics by means of medical history and status on presentation are listed in Table 1 . Therapeutic interventions during the follow-up period are listed in Table 2 .
| Variable | Value |
|---|---|
| Age (yrs), mean ± SD | 60.3 ± 9.7 |
| Men | 663 (77.0%) |
| Arterial hypertension | 394 (45.8%) |
| Current smoking | 513 (59.6%) |
| Diabetes mellitus | 255 (29.6%) |
| Hypercholesterolemia | 549 (63.8%) |
| Familial coronary artery disease | 383 (44.5%) |
| Previous stable angina pectoris | 119 (13.8%) |
| Previous myocardial infarction | 143 (16.6%) |
| Previous percutaneous coronary intervention | 108 (12.5%) |
| Previous coronary bypass | 87 (10.1%) |
| Time from symptom onset to fibrinolysis >4 h | 313 (36.4%) |
| Anterior wall myocardial infarction | 451 (52.4%) |
| Killip class II–IV | 126 (14.6%) |
| Heart rate >100 beats/min | 97 (11.3%) |
| Systolic blood pressure <100 mm Hg | 38 (4.4%) |
| Body weight <67 kg | 76 (8.8%) |
| Therapy | n (%) |
|---|---|
| Coronary revascularization | 623 (72.4%) |
| Aspirin | 840 (97.6%) |
| Statins | 638 (74.1%) |
| β blockers | 743 (86.3%) |
| Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers | 732 (85.0%) |
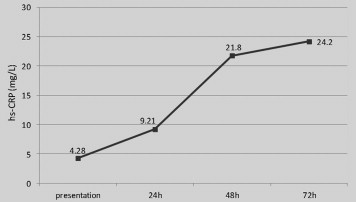
Hs-CRP was found to increase, as expected, at a lower rate for the first 24 hours and then in a steeper way for the next day. The levels of hs-CRP continued increasing until at least the 72-hour measurement ( Figure 1 ).
The median follow-up duration was 3.5 years. Data regarding clinical outcomes were obtained for all patients. By the end of the follow-up period, nonfatal MI was observed in 16.1% of the study patients, and cardiac death was reached by 22.4%.
Univariate analysis was performed for all baseline variables, therapeutic interventions, and the different measurements of hsCRP levels to investigate their significance as univariate predictors. Variables that reached statistical significance in univariate analysis were included in the multivariate model. Thus, age, gender, hypertension, diabetes mellitus, previous MI, previous revascularization, delay until fibrinolysis >4 h, anterior wall MI, Killip class II to IV, heart rate >100 beats/min, and systolic blood pressure <100 mm Hg were the adjusting variables. Multivariate Cox regression analysis demonstrated that hsCRP level at presentation was an independent predictor of the 2 end points, while CRP level at 24 hours did not yield statistically significant results. HsCRP levels at 48 and 72 hours were found to be an independent predictor only of cardiac death ( Table 3 ).



