Depressed baroreflex sensitivity (BRS) is associated with an increased risk of mortality in patients with a known cardiac disease. The prognostic significance of BRS in subjects without history of major cardiovascular (CV) events is unknown. The present study tested the hypothesis that impaired BRS predicts the CV mortality in a population-based sample of middle-aged subjects. The present study is a part of the Oulu Project Elucidating Risk of Atherosclerosis study, where middle-aged hypertensive and age- and gender-matched control subjects were randomly selected. Along with clinical and laboratory assessments, BRS was measured from the blood pressure overshoot of Valsalva maneuver in 559 subjects (age 51 ± 6 years; 300 men). The causes of death (n = 72) were registered during a follow-up of up to 19 years. CV death (n = 23) was defined as the primary end point. CV death was predicted by smoking status, alcohol consumption, high-sensitivity C-reactive protein, use of diuretics, waist circumference, and fasting glucose. Among all measured risk factors, impaired Valsalva BRS (<3 ms/mm Hg) was the most potent predictor of CV death (hazard ratio 9.1, 95% confidence interval 3.8 to 21.7, p <0.001) and remained so after adjustments for the other significant predictors (hazard ratio 5.3, 95% confidence interval 2.1 to 13.3, p <0.001). In conclusion, impaired Valsalva BRS is a potent and independent predictor of CV death in a population-based sample of middle-aged subjects without history of major CV complications and may have important clinical implications in early risk stratification.
Impaired baroreflex sensitivity (BRS) is an important risk factor in patients with cardiac and renal diseases. The prognostic significance of depressed BRS in population without previous major cardiovascular (CV) complications is unclear. Schwartz et al documented that depressed BRS is a powerful risk factor also in healthy animals, raising an important hypothesis on predictive power of BRS in subjects without history of severe CV events. Therefore, the aim of the present study was to assess the long-term prognostic significance of impaired BRS, as assessed by Valsalva method, in a population-based sample of middle-aged subjects. We hypothesized that impaired Valsalva BRS is a significant and independent predictor of CV death and may serve as a potent a risk marker in early prevention.
Methods
The present study is a part of the Oulu Project Elucidating Risk of Atherosclerosis (OPERA) study, where middle-aged hypertensive subjects and age- and gender-matched control subjects were randomly selected in the early 1990s from the national registry for reimbursement of medications for the purpose of assessing the prognostic significance of risk factors in predicting atherosclerotic CV diseases. Subjects with previous myocardial infarction or stroke were excluded. A total of 559 subjects (227 with treated hypertension and 332 controls, Table 1 ) completed the study. The study was performed according to the Declaration of Helsinki and approved by the Ethics Committee of the Medical Department of the University of Oulu, and all the subjects gave their written informed consent.
| Variable | Survivors (n = 487) | Cardiovascular Death (n = 23) | Non-cardiovascular Death (n = 49) |
|---|---|---|---|
| Men | 251 (52%) | 18 (78%)* | 31 (63%) |
| Age (years) | 51 ± 6 | 51 ± 6 | 52 ± 6 |
| Body mass index (kg/m 2 ) | 27 ± 4 | 28 ± 3 | 28 ± 4 |
| Current smoker | 123 (25%) | 13 (57%) † | 17 (35%) |
| Alcohol consumption ≥100 g/week | 97 (20%) | 12 (52%) † | 13 (27%) |
| Hypertension | 196 (40%) | 13 (57%) | 27 (55%) |
| Coronary artery disease | 24 (5%) | 3 (13%) | 5 (10%) |
| General cardiovascular risk ≥15% | 196 (40%) | 16 (70%) † | 25 (51%) |
| Laboratory assessments | |||
| Systolic blood pressure (mm Hg) | 145 ± 21 | 158 ± 26∗ | 152 ± 25 |
| Diastolic blood pressure (mm Hg) | 88 ± 12 | 92 ± 12 | 91 ± 15 |
| Heart rate (bpm) | 72 ± 12 | 72 ± 17 | 74 ± 13 |
| Valsalva baroreflex sensitivity (ms/mm Hg) | 8.9 ± 4.6 | 7.3 ± 5.1 | 7.8 ± 4.5 |
| Left ventricular mass index | 127 ± 47 | 143 ± 32∗ | 142 ± 40 † |
| Left ventricular fractional shortening (%) | 35 ± 6 | 36 ± 5 | 34 ± 5 |
| Fasting glucose | |||
| (mmol/L) | 4.4 ± 0.5 | 4.6 ± 0.6 | 4.6 ± 0.6 |
| (mg/dL) | 79 ± 9 | 83 ± 11 | 82 ± 11 |
| Total cholesterol | |||
| (mmol/L) | 5.7 ± 1.0 | 5.7 ± 1.0 | 5.5 ± 1.0 |
| (mg/dL) | 220 ± 39 | 221 ± 40 | 213 ± 40 |
| Low-density lipoprotein cholesterol | |||
| (mmol/L) | 3.6 ± 0.9 | 3.5 ± 1.0 | 3.3 ± 0.9 |
| (mg/dL) | 137 ± 36 | 135 ± 37 | 128 ± 36 |
| High-density lipoprotein cholesterol | |||
| (mmol/L) | 1.4 ± 0.9 | 1.3 ± 0.5 | 1.3 ± 0.3 |
| (mg/dL) | 53 ± 14 | 52 ± 18 | 51 ± 13 |
| Triglycerides | |||
| (mmol/L) | 1.4 ± 0.7 | 1.9 ± 1.3 | 1.5 ± 0.9 |
| (mg/dL) | 125 ± 60 | 165 ± 120 | 136 ± 78 |
| High-sensitivity C-reactive protein (mg/L) | 2.5 ± 4.4 | 3.9 ± 3.1 † | 5.2 ± 8.8 |
| Treatment | |||
| Beta-blockers | 88 (18%) | 4 (17%) | 15 (31%) |
| Angiotensin converting enzyme inhibitors | 88 (18%) | 7 (30%) | 10 (20%) |
| Calcium channel blockers | 35 (7%) | 4 (17%) | 6 (12%) |
| Diuretics | 50 (10%) | 7 (30%) † | 6 (12%) |
| Waist circumference ♀ ≥80, ♂ ≥94 cm | 239 (49%) | 19 (83%) † | 33 (67%)∗ |
| Triglycerides ≥1.7 mmol/L or treated | 123 (25%) | 10 (44%) | 16 (33%) |
| High-density lipoprotein cholesterol ♀ <1.3, ♂ <1.0 mmol/L or treated | 55 (11%) | 3 (13%) | 6 (12%) |
| Systolic blood pressure ≥130 or diastolic blood pressure ≥85 mm Hg or treated | 389 (80%) | 22 (96%) | 43 (88%) |
| Fasting glucose ≥5.0 mmol/L or treated | 55 (11%) | 7 (30%)∗ | 8 (16%) |
The subjects filled a questionnaire regarding their health status, including smoking status and alcohol consumption, and underwent a clinical examination where height, weight, body mass index, waist circumference, and seated blood pressure (BP) and heart rate (Dinamap, Critikon Ltd, Ascot, United Kingdom) at rest were measured. Coronary artery disease was defined according to history of angina pectoris and Minnesota code from electrocardiography at rest. A venous blood sample was drawn from an antecubital vein after overnight fasting. The concentrations of blood glucose, total cholesterol, high- and low-density lipoprotein cholesterol, triglycerides, and high-sensitivity C-reactive protein (hs-CRP; enzyme-linked immunosorbent assay kit by Diagnostics Systems Laboratories, Webster, Texas) were quantified. General CV risk (%) was then calculated. Left ventricular fractional shortening and mass index according to Devereux et al were measured by the same experienced cardiologist who was blinded to the patients’ clinical data (M-mode, Hewlett-Packard 77020A; Hewlett-Packard Company, Andover, Massachusetts).
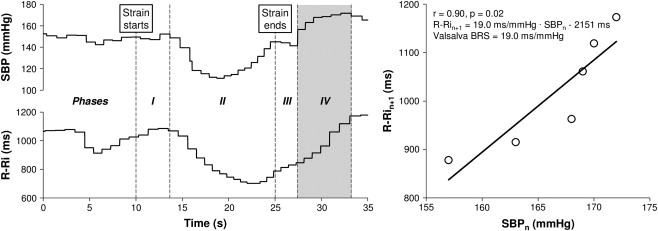
Valsalva BRS was assessed from cardiac vagal efferent responses in RR interval to BP overshoot (phase IV, Figure 1 ) of Valsalva maneuver. The Valsalva maneuver was conducted in a seated position by blowing into a rubber tube connected to an aneroid manometer and maintaining an expiratory strain of 40 mm Hg for 15 seconds. A small leak in the rubber tube was used to force the subjects to blow continuously with open glottis to maintain the pressure. After strain release, the subjects remained still and silent and breathed normally. The Valsalva maneuver was performed 3 times with 5-minute intervals. Electrocardiography and BP (Finapres, Ohmeda Monitoring Systems, Englewood, Colorado) were continuously recorded with sampling frequency of 200 Hz and analyzed with a software package (CAFTS; Medikro Oy, Kuopio, Finland). The Valsalva BRS was calculated as the linear regression slope between RR intervals and preceding systolic BP from phase IV. Data were visually verified, and test was rejected if phase IV could not be determined because of noise or ectopic beats. Regression slopes with r >0.7 or p <0.05 and an increase in systolic BP >15 mm Hg were accepted and averaged to obtain representative value for the Valsalva BRS (n = 401 and n = 158 for ≥2 and 1 accepted slopes, respectively).
The follow-up started from the day of examination in 1990 to 1993 and lasted until 2009, or death. The records of mortality were followed up from the National Death Registry. The deaths (n = 72, 13%) were defined as CV (n = 23, 4%) or non-CV deaths (n = 49, 9%), the former being the primary end point of the present study. The mean follow-up times were 18 ± 1 years in survivors, 14 ± 4 years in CV death, and 11 ± 4 years in non-CV death. No other examinations, related to the present study, were conducted during the follow-up.
Values are expressed as the mean ± SD or the number of subjects (%). The Kruskal-Wallis or chi-square test was used to assess differences between the groups followed by post hoc tests by Mann-Whitney U test or chi-square test corrected for multiple comparisons. Stepwise binary logistic regression was used to determine factors underlying abnormal Valsalva BRS.
The prognostic significance of impaired Valsalva BRS was assessed according to recommendations. Hazard ratios (HR) with 95% confidence intervals were calculated by univariate Cox regression analysis for each risk marker. Predefined cut-off values were used for continuous variables (heart rate ≥84 beats/min ; alcohol consumption ≥100 g/week ; left ventricular mass index ≥122 for women and ≥149 for men ; left ventricular fractional shortening <32% ; hs-CRP ≥3.0 mg/L ; waist circumference ≥80 cm for women and ≥94 cm for men; triglycerides ≥1.7 mmol/L or drug-treated; high-density lipoprotein cholesterol <1.3 mmol/L for women and <1.0 mmol/L for men or drug-treated; fasting glucose ≥5.0 mmol/L or drug-treated ; total cholesterol ≥6.2 mmol/L; low-density lipoprotein ≥4.1 mmol/L ; and BRS <3 ms/mm Hg ). The cut-off value for the Valsalva BRS (<3.0 ms/mm Hg) was determined a priori based on the clinical studies with phenylephrine method and a good concordance between Valsalva and phenylephrine methods. For age and general CV risk, the optimal cut-off value was defined from receiver operating characteristic analysis as the maximum sum of sensitivity and specificity above the median, with sensitivity being at least 20% using CV death as the end point.
Stepwise multivariate Cox regression analysis was performed including gender, age, smoking, alcohol consumption, hypertension, coronary artery disease, heart rate at rest, hs-CRP, diuretics, waist circumference, fasting glucose, triglycerides, total cholesterol, and low-density and high-density lipoprotein cholesterol using CV death as the end point (block I). Thereafter, Valsalva BRS was entered into the model (block II). The proportional hazard and linearity assumptions were verified for each risk marker.
The discrimination of the risk markers was assessed by the C-index and Nagelkerke’s binary R 2 calculated for the final model and after removal of 1 variable at a time. The integrated discrimination index and net reclassification index (risk levels: 0 to <6, 6 to <10, 10 to <20, and ≥20% ) were also calculated. Hosmer-Lemeshow goodness-of-fit test was used to assess calibration of risk models. Additional value of Valsalva BRS to the general CV risk was similarly assessed. Kaplan-Meier analysis with log-rank analysis was used to describe CV death-free survival in low- and high-risk groups. Positive and negative predictive accuracies along with sensitivity and specificity of abnormal Valsalva BRS to predict CV death were calculated. The data were analyzed using SPSS software (IBM SPSS Statistics 21; IBM Corp., Armonk, New York) and R Statistics (2.15.3; The R Foundation for Statistical Computing, Vienna, Austria). A p value of <0.05 was considered statistically significant.
Results
Hypertension (p <0.001), current smoking (p = 0.001), female gender (p = 0.003), and advanced age (p = 0.019) were the most significant determinants of abnormal BRS. Impaired Valsalva BRS involved ninefold univariate risk for CV death ( Table 2 ; Figure 2 ), positive and negative predictive accuracies and sensitivity and specificity being 19% and 97%, and 35% and 94%, respectively. In multivariate analysis without impaired Valsalva BRS in the model, advanced age, current smoking, larger alcohol consumption, use of diuretics, and high hs-CRP level remained as significant predictors of CV death (HR 2.6 to 3.3, p value 0.007 to 0.025). The addition of impaired Valsalva BRS into the model improved the predictability of CV death (chi-square change: 10.8, p = 0.001), and depressed Valsalva BRS still predicted CV death (HR 5.3, 95% confidence interval 2.1 to 13.3, p <0.001). Abnormal Valsalva BRS predicted CV death also independently from general CV risk score (HR 7.1, 95% confidence interval 2.9 to 17.2, p <0.001). While binary R 2 improved most when impaired Valsalva BRS was included in the model (from 0.192 to 0.235), a modest improvement in the C-index was observed (from 0.810 to 0.820), the inclusion of smoking status improving the C-index most (from 0.786 to 0.820). In reclassification analyses, integrated discrimination index was significant, whereas net reclassification index only trended so ( Table 3 ). The predicted risk obtained by the final model was well calibrated (chi-square = 15.5, p = 0.008). The addition of abnormal Valsalva BRS to high general CV risk improved C-index from 0.650 to 0.714, integrated discrimination index and net reclassification index being 0.05 (p = 0.008) and 0.28 (p = 0.14), respectively.



