Coronary computed tomographic angiography can detect nonobstructive atherosclerotic lesions that would not otherwise have been detected with functional cardiac imaging. Currently, limited data exist regarding the clinical significance of these lesions in patients with acute chest pain. The aim of our study was to examine the prognostic significance of these nonobstructive findings in a patient population presenting with acute chest pain. We evaluated 959 consecutive patients who underwent coronary computed tomographic angiography for investigation of acute chest pain. The patients were classified as having normal (n = 545), nonobstructive coronary artery disease (CAD; defined as any narrowing <50% diameter stenosis; n = 312), or obstructive CAD (narrowing of ≥50% diameter stenosis; n = 65). Follow-up data for a minimum of 12 months (mean 27 ± 11) was obtained for any major adverse coronary events consisting of death, nonfatal acute coronary syndrome, and coronary revascularization. Compared to patients with normal coronary arteries, those with nonobstructive CAD were older and had a greater prevalence of CAD risk factors. The incidence of major adverse coronary events was equally low among both these groups (0.6% vs 1.3%, for the normal and nonobstructive groups, respectively, p = 0.2). In conclusion, patients with either nonobstructive CAD or normal findings, as evaluated by coronary computed tomographic angiography, for acute chest pain during an intermediate-term follow-up period had equally benign clinical outcomes.
Coronary computed tomographic angiography (CCTA) has emerged as an excellent noninvasive diagnostic modality to assess coronary artery disease (CAD) in low- to moderate-risk patients. Because of its high negative predictive value, CCTA is particularly useful in excluding significant coronary artery stenosis in patients with acute chest pain who have an atypical presentation. Patients found to have obstructive CAD using CCTA, defined as coronary plaques causing a ≥50% reduction in the luminal diameter, are known to have a worse prognosis than those with normal or nonobstructive (<50% luminal stenosis) CAD. However, when evaluating patients presenting with acute chest pain, CCTA can identify nonobstructive, atherosclerotic plaques, that might or might not be related to patient symptoms, and probably would not have been detected using functional cardiac imaging. Currently, few data exist regarding the long-term prognostic significance of nonobstructive CAD found using CCTA, especially in patients presenting with acute chest pain. The aim of our study was to examine the prognostic significance of nonobstructive CAD detected using CCTA in a large cohort of consecutive, nonselective, real-world patients presenting with acute chest pain and undergoing evaluation by a dedicated chest pain unit (CPU) team using a strict protocol.
Methods
The study cohort included 959 consecutive patients who presented with acute chest pain and were admitted to the CPU. All patients were referred for CCTA within 24 hours of admission after acute coronary syndrome (ACS) had been ruled out. The patients underwent CCTA, after a ≥12-hour observation period to rule out ACS, when a repeat electrocardiogram was done, with findings unchanged from baseline, and the findings from a repeat cardiac biomarker evaluation were negative. The inclusion criteria for undergoing evaluation by CCTA included no previous history of CAD; age ≤70 years; weight ≤120 kg; sinus rhythm; no known contraindication to iodine contrast administration; and serum creatinine <1.4 mg/dl.
All findings from CCTA were interpreted by staff cardiologists and roentgenologists. Coronary computed tomographic angiographic studies were classified as showing normal coronary arteries (no evidence of coronary atherosclerosis); nonobstructive CAD (any evidence of coronary atherosclerosis with <50% luminal narrowing); obstructive CAD (evidence of coronary atherosclerosis with ≥50% luminal narrowing); or inconclusive test results because of technical difficulties.
Patients with obstructive CAD by CCTA were referred for invasive coronary angiography and treated accordingly. Patients with normal findings or nonobstructive CAD were discharged with adequate recommendations for lifestyle modifications (i.e., smoking cessation, dietary changes, and physical activity). In patients with nonobstructive CAD, lipid-lowering therapy (statin) was initiated, regardless of the low-density lipoprotein levels with a target low-density lipoprotein cholesterol goal of <70 mg/dl, plus aspirin. Follow-up data for ≥1 year, with a mean follow-up period of 27 ± 11 months, was obtained for the entire study population. The follow-up data were obtained by 2 study investigators, who were unaware of the coronary computed tomographic angiographic findings, from either an outpatient clinic visit or a telephone interview using a prespecified questionnaire. The prespecified clinical end points during follow-up were recurrent episodes of chest pain, additional diagnostic tests (both noninvasive and invasive) performed because of chest pain, repeated hospitalizations for chest pain suspected as ACS, ACS (consisting of chest pain in the presence of either electrocardiographic changes suggestive of myocardial ischemia or infarction and/or troponin elevation), coronary revascularization (either percutaneous or bypass grafting), and death. The primary study end points were prespecified major adverse coronary events (MACE), coronary revascularization (urgent and nonurgent), ACS, and death. The number of events was counted as 1 per patient (counted as the first event) even if that patient experienced several events. The secondary end points included cardiovascular MACE consisting of ACS and/or cardiovascular death. For patients without available follow-up data, we reviewed the medical records and used the national population registry of the Ministry of Interior to evaluate whether the outcome of death had occurred. The results of the first 444 patients included in the present analysis have been previously reported.
All coronary computed tomographic angiographic scans were performed using a 64-slice scanner (Brilliance 64, Philips Medical Systems, Cleveland, Ohio), with retrospective electrocardiographic gating. Heart rate control was achieved by oral β-blocker administration (propranolol 20 to 50 mg) 1 hour before scanning. Intravenous β-blocker administration (metoprolol 5 to 15 mg) was added if heart rate increased to >70 beats/min. The first scan was acquired with prospective gating for calcium score evaluation, with the scan volume starting at the lung apices and ending at the level of the diaphragm. Per protocol, patients with a high calcium score (Agatson score ≥800) were excluded from additional analysis; however, none of the patients who were referred for CCTA in our cohort had a high calcium score (>800). The contrast-enhanced scan was acquired with retrospective gating. A mean bolus of 80 ml (range 70 to 110) of nonionic contrast medium (Iomeron [iomeprol]) was injected into an antecubital vein at a flow rate of 4 to 6 ml/s. The scanning parameters included voltage, 120 kV (increased to 140 kV in patients weighing >100 kg); effective tube current, 800 to 1,235 mA; slice collimation, 64 × 0.625 mm; gantry rotation time, 400 ms; pitch, 0.2 (reduced to 0.17 in patients weighing >100 kg). Dose modulation (full radiation dose only during 40% to 80% of the RR interval) was applied whenever possible to decrease radiation exposure. Diastolic phases (70% to 80% of the RR interval) were used for data reconstruction as the default. Systolic phases (35% to 45% of the RR interval) were used if heart rate increased to >70 beats/min. Each vessel was reconstructed using curved multiplanar reformats (extended workspace, Philips Medical Systems). All studies were analyzed and interpreted by experienced radiologists and cardiologists specializing in cardiovascular imaging. As previously stated, the patients were divided into 4 groups: (1) normal coronary arteries, (2) nonobstructive CAD, (3) obstructive CAD, and (4) inconclusive test owing to technical difficulties. The institutional ethics committee approved the present study.
Statistical analysis was performed using SPSS, version 12 (SPSS, Chicago, Illinois). Continuous variables are presented as mean ± SD or median and interquartile range and categorical variables as percentages. Continuous variables were compared using the Student t test if data followed a normal distribution and using the Wilcoxon rank sum test, if the data were skewed. Categorical variables were compared using the chi-square test or Fisher’s exact test when indicated. All tests were 2-sided, and p values <0.05 were considered statistically significant.
Results
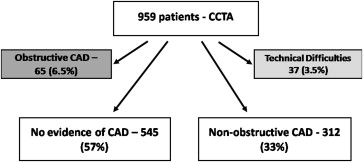
The study included 959 consecutive patients who presented to the emergency department with acute chest pain, were admitted to the CPU, and were further evaluated by CCTA. As per protocol, CCTA was performed only after ruling out ACS, which was determined from the repeat cardiac biomarker evaluation findings, an absence of recurrent ischemic changes on the ST-T analyzer during an observation period of ≥12 hours, and/or repeat electrocardiography. Figure 1 illustrates the patient distribution: of the 959 consecutive patients who underwent CCTA after ruling out ACS. Of these patients, 37 (3.5%) had a noninterpretable scan because of technical difficulties, 65 patients (6.5%) had obstructive CAD and, per protocol, were referred for invasive coronary angiography, 545 patients (57%) had normal coronary arteries, and 312 patients (33%) had nonobstructive CAD. Thus, 857 patients with a technically adequate study and either normal findings or nonobstructive CAD were the focus of the present evaluation. The patient baseline characteristics are listed in Table 1 . Patients with nonobstructive CAD were older (age 52 ± 9 vs 48 ± 9 years, p <0.01), more likely be men (72% vs 60%, p = 0.05), with a higher risk profile for coronary disease, including an unfavorable lipid profile, compared to those who with normal coronary arteries. The C-reactive protein levels did not differ between the 2 groups.
| Variable | CCTA | p Value | |
|---|---|---|---|
| Normal (n = 545) | Nonobstructive CAD (n = 312) | ||
| Age | 48 ± 9.1 | 52 ± 8.6 | <0.01 |
| Men | 328 (60%) | 226 (72%) | 0.05 |
| Smoker | 171 (32%) | 124 (40%) | <0.001 |
| Diabetes mellitus | 42 (8%) | 28 (9%) | 0.5 |
| Hypertension ∗ | 123 (23%) | 109 (35%) | <0.001 |
| Hyperlipidemia † | 199 (37%) | 160 (51%) | <0.001 |
| Family history of coronary artery disease | 203 (37%) | 110 (35%) | 0.1 |
| Total cholesterol (mg/dl) | 182 ± 33 | 182 ± 33 | 0.8 |
| Low-density lipoprotein (mg/dl) | 113 ± 25 | 115 ± 26 | 0.2 |
| High-density lipoprotein (mg/dl) | 45 ± 12 | 41 ± 11 | <0.001 |
| Triglycerides (mg/dl) | 125 ± 62 | 144 ± 80 | <0.001 |
| Creatinine (mg/dl) | 0.96 ± 0.16 | 0.99 ± 0.15 | 0.4 |
| C-reactive protein (mg/L) | 5 ± 8.3 | 5.7 ± 18 | 0.8 |
∗ Defined as either a known medical history of hypertension and/or currently treated for hypertension.
† Defined as either a known medical history of hyperlipidemia and/or currently treated with low-density lipoprotein-lowering therapy.
Complete follow-up data were available at a mean duration of 28 ± 11 and 25 ± 11 months for the normal and nonobstructive groups, respectively (p = 0.1). For 54 patients (6%), for whom complete follow-up data were not obtainable, we screened the National Population Registry of the Ministry of Interior for the outcome of mortality for all who were alive. The clinical outcomes of the 2 study groups are listed in Table 2 . In both groups, the number of patients who had recurrent chest pain was similar, as was the number of those readmitted because of chest pain. Nevertheless, those with nonobstructive CAD underwent significantly more additional testing during the follow-up period, both noninvasive (21% vs 11%, p <0.001) and coronary angiography (2.4% vs 0.8%, p = 0.05). However, ultimately, no difference was seen in the number of patients who underwent coronary revascularization by either percutaneous coronary angiography or coronary artery bypass grafting (0.4% vs 0.9%, p = 0.2). The MACE rate was comparably low at 0.6% and 1.3% for the normal and nonobstructive groups, respectively (p = 0.2). One noncardiovascular death occurred in each group, of malignancy in both cases. The rate of cardiovascular MACE was also low and comparable, consisting of only 2 patients in each group (0.4% vs 0.6% for the normal and nonobstructive groups, respectively, p = 0.6), of whom only 1 patient in each group experienced a myocardial infarction.
| Variable | CCTA | p Value | |
|---|---|---|---|
| Normal | Nonobstructive CAD | ||
| Follow-up duration (mo) | 28 ± 11 | 25 ± 11 | 0.1 |
| Recurrent chest pain | 134 (26%) | 81 (28%) | 0.6 |
| Additional diagnostic tests | 57 (11%) | 60 (21%) | <0.001 |
| Invasive coronary angiography | 4 (0.8%) | 7 (2.4%) | 0.05 |
| Readmission for suspected acute coronary syndrome | 23 (4%) | 22 (7%) | 0.2 |
| Coronary revascularization | 2 (0.4%) | 3 (0.9%) | 0.2 |
| Acute coronary syndrome | 2 (0.4%) | 2 (0.6%) | 0.6 |
| Death | 1 (0.1%) | 1 (0.3%) | 0.86 |
| Cardiovascular death | 0 | 0 | |
| Major adverse coronary events (revascularization, acute coronary syndrome, death) | 3 (0.6%) | 4 (1.3%) | 0.2 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


