Chapter 40 Procedures
In this chapter, the common and life-preserving procedures that are performed in the cardiothoracic intensive care unit (ICU) are described. For most procedures there are many acceptable techniques, but for the sake of simplicity and brevity a didactic description of one approach for each procedure is described. All of the procedures described have appreciable learning curves. Therefore, to increase the chance of success and minimize the likelihood of complications, experienced clinicians should always supervise novices.
CONSENT AND DOCUMENTATION
Consent
There is considerable heterogeneity among countries, states, and institutions and even within institutions regarding obtaining consent for procedures. Blanket consent may be obtained at the time of hospital admission or prior to surgery or, alternatively, specific consent may be obtained for individual procedures. Consent may be verbal or written. In a survey of North American practices, blanket consent was obtained in 64% of surgical ICUs but in only 22% of medical ICUs.1 Of the units that obtained consent for individual procedures, most (>80%) obtained consent for central venous and pulmonary arterial catheterization, thoracocentesis, bronchoscopy, gastrointestinal endoscopy, and blood transfusion; most (>80%) did not obtain consent for nasogastric or urinary catheterization. There are few national standards that address the issue of procedural consent. One that does is the U.S. Veterans Health Administration policy on informed consent for clinical treatments and procedures (available from www.publichealth.va.gov/documents/vha_handbook_ 1004.1.pdf), which makes explicit which procedures require signature consent.
SEDATION AND ANALGESIA FOR BEDSIDE PROCEDURES
Sedation and anesthesia are part of a continuum, and the point at which one becomes the other is indistinct. The goal of sedation is that the patient be relaxed and comfortable but remain conscious (“conscious sedation”), that the patient’s airway be maintained and protected, and that the patient breathe regularly. Anesthesia implies loss of consciousness and is commonly associated with airway obstruction and apnea. For patients who are mechanically ventilated via an endotracheal tube, this distinction may not be critical. However, in nonintubated, spontaneously breathing patients, inadvertent induction of anesthesia in the absence of the necessary skills or equipment for resuscitation is potentially fatal. Thus, whenever intravenous sedation is used, the equipment and skilled personnel necessary to secure and control the airway should be immediately available. Reversal agents (flumazenil for benzodiazepines and naloxone for opioids; see Chapter 4) should also be available. Patients should be monitored by electrocardiogram (ECG), blood pressure cuff, pulse oximeter, and capnograph. Prior to administering intravenous sedation, patients should fast for 6 hours. If this is not possible, rapid-sequence endotracheal intubation (see subsequent material) should be considered. If a nasogastric tube is in situ, it should be aspirated prior to administering sedative drugs. Patients with cardiac dysfunction may develop marked hypotension with intravenous sedation. Thus, secure intravenous access, along with fluids and a vasopressor, should be available. A clinician other than the proceduralist must be designated to perform sedation and monitor the patient. Only a suitably trained clinician, such as an anesthesiologist, intensivist, or nurse anesthetist, should perform general anesthesia.
Sedation for Patients who Are Extubated and Breathing Spontaneously
Supplemental oxygen should be administered by a face mask. For conscious sedation, small intravenous bolus doses of midazolam (1 to 2 mg) may be administered every 1 to 5 minutes until a satisfactory degree of sedation has been achieved. This may be supplemented with a small dose of fentanyl (0.25 to 0.5 μg/kg). Fentanyl is particularly helpful in facilitating instrumentation of the airway or upper gastrointestinal tract, but it substantially increases the risk for apnea. As sedation is established, the clinician should constantly assess the patient’s level of consciousness (see Chapter 4) and be prepared to support the airway and breathing.
BASIC AIRWAY MANAGEMENT
Basic airway management involves (1) maintaining a patent airway and (2) bag-mask ventilation.
Maintaining a Patent Airway
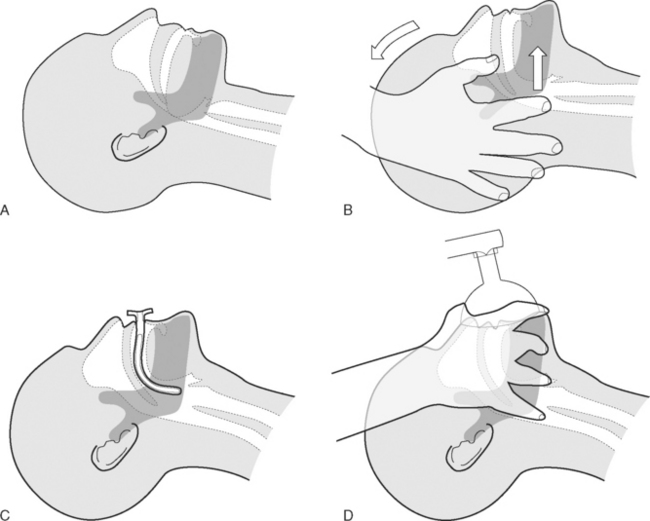
Patients who are unconscious (Glasgow Coma Score <8; see Chapter 37) or who have a reduced level of consciousness may develop partial or complete upper airway obstruction due to prolapse of the base of the tongue into the oropharynx (Fig. 40-1A). Treatment involves the head-tilt, chin-lift maneuver, in which the neck is extended at the atlantooccipital joint and the mandible is thrust forward (Fig. 40-1B). An oropharyngeal airway may also be inserted (Fig. 40-1C). A correctly sized oropharyngeal airway should extend from the patient’s lips to the ear; a size 3 (green) or 4 (orange) is suitable for most adults. If the patient is partially conscious, an oropharyngeal airway may precipitate coughing, vomiting, and laryngospasm.
Bag-Mask Ventilation
In patients who are apneic, bag-mask ventilation should be performed using a self-inflating manual resuscitator with an oxygen reservoir bag (see Fig. 28-1). To ensure that the reservoir bag remains filled, an oxygen flow of 15 l/min is typically required. Ventilation via mask requires a tight fit. The correct position of the operator’s hand is shown in Figure 40-1D. It may be possible to achieve a patent airway and a good mask seal with a single hand; if not, two hands should be used, and an assistant should perform the bag compressions. The bag should be inflated 12 to 16 times per minute, and the chest should be seen to rise and fall, while using the lowest effective pressure to minimize the risk of gas insufflation of the stomach.
ENDOTRACHEAL INTUBATION
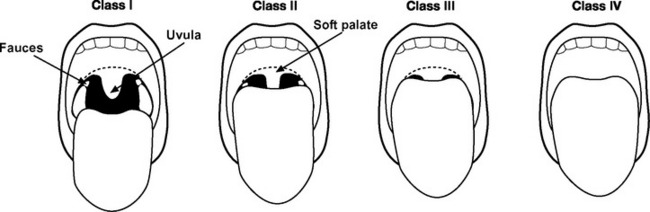
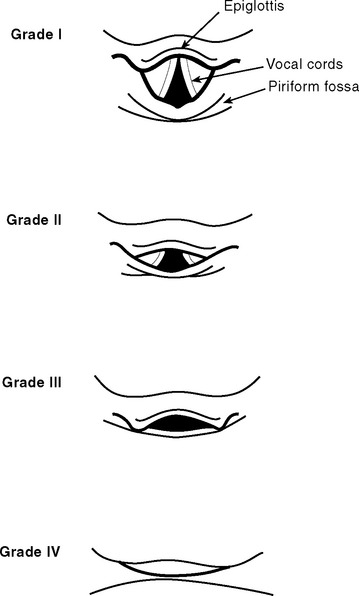
The airway should be assessed to gauge the likelihood of difficulty with laryngoscopy and intubation (Fig. 40-2 and see Table 40-1).2 Reports of previous intubations should be reviewed. If difficulty is anticipated, awake fiberoptic intubation should be considered (see subsequent material).
Table 40-1 Indicators of Difficult Intubation
| Sign | Notes |
|---|---|
| Reduced mouth opening | Patient has an interincisor distance of <4 cm. |
| Reduced thyromental distance | Measured with the neck extended; less than 6.0 cm is abnormal; 6.0 to 6.5 cm is borderline. |
| Mallampati score 3 or 4 | See Fig. 40-2. |
| Limited neck movement | Patient is unable to extend the neck at the atlantooccipital junction or flex the neck. |
| Reduced mandibular subluxation | The mandible is normally able to be protruded so that the lower incisors are in front of the upper incisors. |
| Large incisor teeth | Difficulty intubating an edentulous patient is very rare. |
| Large upper incisor teeth are associated with difficulty. |
Necessary equipment and drugs are listed in Tables 40-2 and 40-3, respectively. An 8.5-mm (internal diameter) endotracheal tube is suitable for most adult males and a 7.5-mm tube is suitable for most adult females.
Table 40-2 Equipment for Endotracheal Intubation
| Selection of face masks |
| Selection of oropharyngeal airways |
| Self-inflating manual resuscitator with oxygen reservoir |
| Two laryngoscopes with a variety of curved and straight blades |
| Selection of endotracheal tubes, one opened with its cuff checked |
| Oxygen source and tubing |
| High-pressure suction with Yankauer connector |
| Intubating bougie |
| Endotracheal tube stylet |
| Magill forceps |
| A syringe for cuff inflation |
| Tape or ties for securing the endotracheal tube |
| Head support |
| Equipment for managing difficult intubation, for example: |
| Laryngeal mask airway |
| Fiberoptic bronchoscope |
| Monitoring |
| Pulse oximeter |
| Capnography |
| Electrocardiogram |
| Blood pressure |
| Adequate venous access |
| Drugs for induction of general anesthesia (see Table 40-3) |
Table 40-3 Drugs That Should Be Drawn Up Prior to Rapid-Sequence Endotracheal Intubation
| Hypnotic |
| e.g., etomidate 0.1 to 0.2 mg/kg |
| e.g., ketamine 1 to 2 mg/kg |
| e.g., propofol 0.5 to 2 mg/kg |
| Opioid with rapid onset |
| e.g., fentanyl 0.5 to 5 μg/kg |
| Suxamethonium |
| 1.5 mg/kg |
| Nondepolarizing neuromuscular blocking drug |
| e.g., pancuronium 0.1 mg/kg |
| e.g., vecuronium 0.1 mg/kg |
| Atropine |
| 600 μg/dose |
| Vasopressor |
| e.g., phenylephrine 50 to 100 μg/dose |
| e.g., metaraminol 0.5 to 1 mg/dose |
| Saline flush |
Three staff members are required for the procedure: (1) an operator who stands at the head of the bed and performs preoxygenation, laryngoscopy, and intubation; (2) an assistant on the operator’s left who performs cricoid pressure; (3) an assistant on the operator’s right who administers drugs, retracts the upper lip, and hands the endotracheal tube to the operator.
Rapid-Sequence Intubation
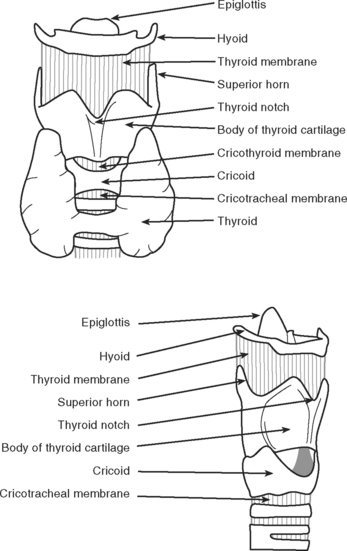
Rapid-sequence intubation involves the induction of general anesthesia and neuromuscular paralysis, followed promptly by endotracheal intubation. The risk of regurgitating and aspirating gastric contents is minimized by the application of cricoid pressure and avoiding bag-mask ventilation.3 The cricoid cartilage (Fig. 40-3) is the only complete cartilaginous ring. Firm pressure on the cricoid cartilage compresses the underlying esophagus and helps to prevent regurgitation of gastric contents.
The technique is performed as follows:
Technique of Direct Laryngoscopy and Intubation
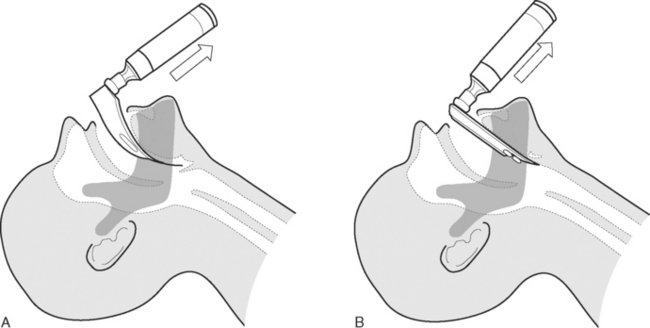
Direct laryngoscopy is usually performed using a curved (MacIntosh) size 3 or 4 laryngoscope. Alternatively, a straight (Miller) blade may be used. Once the patient has been anesthetized, the mouth is held open by the operator’s right hand. Dentures are removed. With the laryngoscope held in the operator’s left hand, the blade is passed down the right side of the tongue and into the oropharynx until the epiglottis comes into view. The correct positions of curved and straight laryngoscope blades are shown in Figure 40-4. The larynx is visualized by lifting (not pivoting) the laryngoscope blade anteriorly, thereby elevating the tongue and epiglottis. The potential views obtained at laryngoscopy are shown in Figure 40-5. The assistant on the operator’s right retracts the patient’s upper lip and passes the endotracheal tube to the operator’s right hand. The endotracheal tube is inserted through the larynx under direct vision. A distance of 21 to 23 cm from the lips for males and 20 to 22 cm from the lips for females is usually appropriate.
Complications
Respiratory
Mild hypoxemia is reasonably common during urgent intubations performed in the ICU. If the patient’s oxygen saturation (SPo2) falls significantly (<90%) during attempted intubation, bag-mask ventilation should be commenced while maintaining cricoid pressure. Further attempts at intubation should be delayed until the SPo2 has recovered. Persistent unsuccessful attempts at intubation will lead to profound hypoxemia and even death. If intubation is not successful after three attempts (with bag-mask ventilation in between), the procedure should be abandoned, and the patient ventilated by bag-mask until the drugs have worn off, usually in about 10 minutes. If bag-mask ventilation is difficult, an oropharyngeal airway should be inserted. If problems persist, cricoid pressure should be relaxed. Failing this, emergency help should be sought from a senior clinician. Insertion of a laryngeal mask airway may be lifesaving.
Unrecognized esophageal intubation can also lead to profound hypoxemia and even death. It is essential to check that the endotracheal tube is correctly positioned, as described earlier. If a characteristic capnograph trace (see Fig. 8-13A) is not seen within two to three breaths, the tube should be removed and bag-mask ventilation commenced. Even with successful tube placement, the patient’s SPo2 may continue to fall for the first few breaths.
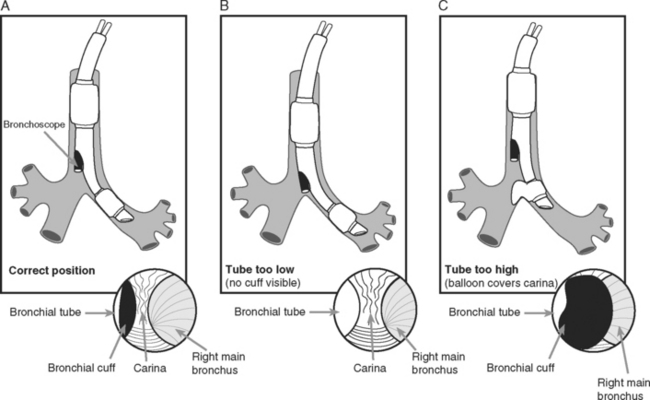
INSERTION OF A DOUBLE-LUMEN ENDOTRACHEAL TUBE
A double-lumen endotracheal tube is occasionally required for differential lung ventilation following single lung transplantation or for lung isolation in cases of massive hemoptysis or bronchopleural fistula. Because of the short length of the right main bronchus (Fig. 40-6), right-sided tubes are more difficult to position and are prone to occluding the origin of the right upper lobe bronchus.4 Thus, a left-sided tube should be used in almost all circumstances, including selective ventilation of the right lung. For adult males, a 41F or 39F tube is usually appropriate; for adult females, a 39F or 37F tube is usually appropriate.
Technique of Insertion
Assessment of Correct Tube Position
Following “blind” insertion, as described earlier, approximately 25% of double-lumen tubes are incorrectly positioned and cannot be used to ventilate the lungs selectively.5 Furthermore, when examined bronchoscopically, a significant proportion (15% in one study5) of “functioning” tubes are critically malpositioned. Thus, careful clinical and bronchoscopic assessment is indicated.
Clinical Assessment
Bronchoscopic Assessment
The fiberoptic bronchoscope is passed down the tracheal lumen. With correct positioning, the carina and right main bronchus should be clearly visualized. The origin of the left main bronchus is obscured by the endobronchial lumen, but the proximal margin of the (blue) endobronchial cuff should be just visible (see Fig. 40-6A). The bronchoscopic findings when the tube has been advanced too far or not far enough are shown in Figure 40-6B and C, respectively).
FIBEROPTIC LARYNGOSCOPY AND BRONCHOSCOPY
Fiberoptic laryngoscopy is usually indicated to facilitate tracheal intubation in patients who are known to be difficult to intubate by direct laryngoscopy. The indications for bronchoscopy in the ICU are listed in Table 40-4. Relative contraindications to bronchoscopy include severe coagulopathy, pulmonary arterial hypertension, and bronchospasm. In general, diagnostic bronchoscopy should be avoided in patients with severely impaired gas exchange because it may cause further respiratory embarrassment. By contrast, therapeutic bronchoscopy—for instance, for treating lobar collapse due to mucus plugging—may significantly improve gas exchange.
Table 40-4 Indications for Fiberoptic Bronchoscopy in the ICU
| Diagnostic |
| Diagnosis of pneumonia |
| Diagnosis of bronchopleural fistula |
| Identification of a bleeding site |
| Identification of injury following airway trauma |
| Therapeutic |
| Relief of mucus plugging |
| Removal of foreign body |
| Identification of the correct placement of double-lumen endotracheal tube |
| Lung isolation to treat massive hemoptysis or bronchopleural fistula |
| Placement of fibrin glue to treat bronchopleural fistula |
ICU, intensive care unit.